Introduction: The treatment of recurrent pleura] effusion or recurrent pneumothorax frequently involves the creation of a pleurodesis. Ultrasound is being used more frequently to assess the presence of pleural fluid or pneumothorax. With ultrasound, the gliding sign displays the gliding of the visceral pleura over the parietal pleura during respiration. The absence of a gliding sign is indicative of a pneumothorax.
Hypothesis: We hypothesized that the presence of pleurodesis would be indicated by the absence of a gliding sign on ultrasound.
Methods: To create a pleurodesis, a single intrapleural injection of transforming growth factor-132 at a dosage of 1.70 [micro]g/kg or doxycycline at a dosage of 10 mg/kg in a volume of 2.0 mL was administered randomly to one side of a New Zealand White rabbit. Prior to death on day 14 after intrapleural injection, all rabbits underwent an ultrasonic examination at three marked sites on each side of the chest. At each site, three ultrasonic features (gliding sign, pleural thickening, and pleural effusion) were evaluated and graded. The gliding sign was graded as follows: 0 = gliding sign definitely present, 1 = gliding sign questionable, 2 = gliding sign absent.
Results: In a preliminary study for developing skill in assessing the gliding sign, the correlation between the gliding sign and the pleurodesis score in 16 rabbits was highly significant (r = 0.568, p = 0.02). In the subsequent main study with 18 additional rabbits, the correlation between the gliding sign score and the pleurodesis score was even better (r = 0.806, p = 0.00009). The gliding sign was definitely present on the noninjected side in all rabbits
Conclusions: The presence of a pleurodesis is indicated by the absence of a pleural guiding sign on ultrasound.
Key words: gliding sign; pleural effusion; pleurodesis; pneumothorax; ultrasound
Abbreviation: TGF = transforming growth factor
**********
Pleurodesis is the fusion of the visceral and parietal pleura. Pleurodesis usually results from pleural inflammation produced by an injury to the pleura. The treatment of recurrent pleural effusion or recurrent pneumothorax frequently involves an attempt to create a pleurodesis. (1) In clinical practice, a pleurodesis is most commonly created by injecting a sclerosing agent into the pleural space through a chest tube. (2)
The assessment of the presence of a pleurodesis is difficult. In most clinical articles on pleurodesis for pleural effusion, its presence is assessed by the presence or absence of pleura] fluid. However, this assessment only indicates whether fluid has reaccumulated but does not indicate if a pleurodesis has occurred. Neither standard chest radiographs nor CT scans demonstrate whether pleurodesis has occurred.
Advances in technology have greatly improved the imaging capabilities of ultrasound. Ultrasound has been proved to be a reliable, efficient, and informative imaging modality for the evaluation of a wide variety of chest diseases. (3-7) Using ultrasound, the parietal pleura and the visceral pleura are normally seen as two thin, bright echogenic lines just beneath the chest wall. The two pleural lines normally glide over one another during respiratory movements in real-time ultrasonography. This movement is termed the gliding sign of the pleura. The absence of a gliding sign with ultrasonography has been used to diagnose pneumothorax. (7-12)
We hypothesized that the assessment of the pleural gliding sign with ultrasound would be an efficient imaging modality for the evaluation of pleurodesis, and the presence of a pleurodesis would be indicated by the absence of a gliding sign. The objective of this study was to investigate whether ultrasound can be used for the diagnosis of pleurodesis.
MATERIALS AND METHODS
Pleurodesis Model
The protocol was approved by the animal care committee of Vanderbilt University, Nashville, TN. A chest tube was inserted into a pleural space of New Zealand White rabbit (1.5 to 2.0 kg) using a method previously described. (13,14) The right or left pleural spaces were selected randomly to receive the chest tube. The other pleural cavity was used as the control. There was a sham incision (< 2 cm) on the control side so that the ultrasonographer would not know which side received the pleurodesis agent. To create different grades of pleurodesis, a single intrapleural injection of either transforming growth factor (TGF)-[[beta].sub.2], 1.70 [micro]g/kg (Genzyme; Framingham, MA) or doxycycline, 10 mg/kg in a volume of 2.0 mL (Fujisawa; Deerfield, IL) was administered in a random fashion to each rabbit via its chest tube.
After the intrapleural injection, the chest tube was aspirated at 24-h intervals for any pleural fluid. The chest tube was removed under light sedation when the pleural fluid drainage was < 5 mL over the preceding 24 h. Gentamicin (2 mg/kg; American Pharmaceutical Partners; Schaumburg, IL) was administered IM during the surgery and at 24-h intervals as long as the chest tubes were in place.
Thoracic Ultrasound
Prior to surgery, all rabbits underwent an ultrasonic examination at three marked sites (one anteriorly in the midclavicular line, one laterally in the mid axillary line, and one posteriorly in a line below the scapula) on each side of their chest in the seated position. At each site, three ultrasound features (gliding sign, pleural thickening, and pleural fluid) were evaluated and graded as shown in Table 1. The total score for each side is the sum of the three scores for each of the three sites. Other ultrasonic findings were noted. Each rabbit was again examined using ultrasound 14 days after the intrapleural injection. Thoracic ultrasound was performed by an experienced radiologist (E.D.) [ATL Ultramark 9; Philips; Bothell, WA] with a compact, linear 10-5 MHz probe. The ultrasonographer was blinded as to which side received the pleurodesis agent. Prior to ultrasonic examination, the fur over the entire thoracic area of each rabbit was removed.
Pleurodesis Scoring
Immediately after the final ultrasound examination, the animals were killed with carbon dioxide after sedation. After death, the thorax was removed en bloc and the lungs were expanded by the injection of 50 mL of 10% neutral-buffered formalin into the exposed trachea via a plastic catheter (6 mm in diameter) as previously described. (13,14) The trachea was then ligated and the entire thorax submerged into 10% neutral-buffered formalin solution for at least 48 h before the pleurodesis was graded. A consensus pleurodesis score was reached by two investigators (K.B.L. and R.W.L.) blinded to the treatment group and the scores on ultrasound. The degree of pleurodesis was semiquantiffed by the scheme outlined in Table 2, a modified version of the scoring system we have used in previous studies. (14) The only modification of this scoring system from the previously used eight-point system is that categories 1 through 4 in the previous system were all combined with the same score (1) since there is no pleural symphysis in any of the first four categories in the system used previously. Any evidence of hemothorax, pleural fluid, or pleural thickening was recorded if present.
Statistical Analysis
All data are presented as mean [+ or -] SD unless otherwise stated. Linear regression was used to analyze the correlation between the pleurodesis score (dependent variable) and the ultrasound scores (independent variable). All data were analyzed with statistical software (SigmaStat V3.0; SPSS; San Rafael, CA); t tests were used to compare the pleurodesis scores in the two different study groups, while the [chi square] test was used to compare the frequency the two different sides and the two different pleurodesing agents were used; p < 0.05 was considered significant.
RESULTS
In the preliminary study, 16 rabbits were studied in order to develop skill in assessing the gliding sign. For these 16 rabbits, there was a significant correlation (r = 0. 568, p = 0.02) between the pleurodesis score and the total gliding sign score (Table 3, Fig 1). At the time of the ultrasonic examination before the rabbits had received either agent intrapleurally, the gliding score was 0 and there was no pleural fluid thickening or fluid in any of the rabbits. Although the radiologist was blinded as to which side received the intrapleural injection, he identified no abnormalities in the gliding, the presence of pleural thickening, or pleural fluid on the noninjected site in any of the rabbits (Table 4).
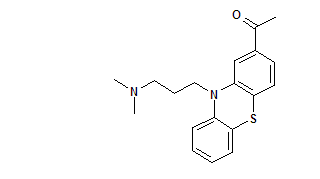
[FIGURE 1 OMITTED]
We learned several things during our studies with the first set of rabbits. We noticed that the gliding sign was difficult to assess when the rabbits were breathing rapidly, so after the first few rabbits were studied we sedated the rabbits with acepromazine (9. mg/kg; Boehringer Ingelheim; St. Joseph, MO) prior to ultrasonic examination. We also observed that a false-positive gliding sign was frequently seen if the gliding sign was assessed too closely to the diaphragm. Accordingly, the subsequent assessment of the gliding sign was not near the diaphragm.
Our accuracy in evaluating pleurodesis with ultrasound increased after this initial experience. Eighteen additional rabbits were used for the main study. One rabbit was excluded from the analysis of the gliding sign because it had > 75% of its hemithorax occupied with a hemothorax at autopsy. The ultrasonic pleural fluid score in this rabbit was 12. With the remaining 17 rabbits, there was an excellent correlation (r = 0.806, p = 0.00009) between the pleurodesis score and the total gliding score (Table 3, Fig 2). The mean pleurodesis scores between the preliminary study (3.6 [+ or -] 1.4) and the main study (4.0 [+ or -] 1.1) were comparable (p > 0.05). Other details of these two groups are shown on Table 5.
[FIGURE 2 OMITTED]
The evaluation of pleural thickening with ultrasound was disappointing. Significant pleural thickening was observed in only two rabbits by ultrasound. A complete pleurodesis was noted in both these rabbits at autopsy. However, we did not find definite pleural thickening on ultrasound in most of the rabbits that had complete pleurodesis. The pleural fluid scores were also not particularly revealing probably because they had effective pleural fluid drainage before ultrasonic examination. One rabbit had a pleural fluid score of 12, and this was the rabbit that was excluded from the study because it had a hemothorax. Only five other rabbits had pleural fluid scores of [greater than or equal to] 2 (none were > 3), and none of them had a significant volume of fluid when their pleural spaces were examined after death. There was not a significant correlation between the pleurodesis score and either the total pleural thickening score or the total pleural fluid score (Table 4).
DISCUSSION
The present study demonstrates that ultrasound is an accurate imaging modality for the evaluation of pleurodesis, in that the absence of pleural gliding on ultrasound correlates well with the presence of a pleurodesis. To our knowledge, this is the first study to demonstrate the efficacy of ultrasound in the diagnosis of pleurodesis.
Until recently, the evaluation of whether a pleurodesis was present was inferred indirectly from the lack of recurrence of pleural fluid or pneumothorax. (15) Although chest radiographs and CT scans can identify pleural thickening and pleural calcification, these imaging modalities cannot demonstrate whether there is fusion of the visceral and parietal pleura, the hallmark of pleurodesis. (16)
Ultrasound has inherent limitations for thoracic imaging because sound waves are reflected by bone and air spaces (such as in lung parenchyma). However, it provides immediate information with real-time imaging and can give information not available from a standard radiograph or CT scan. As advances in its technology have occurred, ultrasound has been increasingly used for evaluating a wide variety of chest diseases. Because of their superficial locations, ultrasound is particularly sensitive in imaging the chest wall, pleura, and pleural space. (3-7) The present study shows that ultrasound is useful in demonstrating whether pleurodesis is present.
To-and-fro movement of the visceral and parietal pleural surfaces can be seen with ultrasonic imaging during the respiratory cycle. This motion is termed the pleural gliding sign. If there is air in the pleural space such that the visceral and parietal pleural are not in contact with each other, the gliding sign is absent. In previous studies, (8,10-12,17-19 the absence of a gliding sign on ultrasound was found to be reliable in the detection of pneumothorax. In a prospective, operator-blinded study, Liehenstein and Menu (8) found that absence of lung gliding was a useful sign for detecting pneumothorax, with a sensitivity of 95.3%, a specificity of 91.1%, and a negative predictive value of 100%. Another study (18) in an Italian emergency department setting showed that ultrasonography performed on 36 patients with blunt thoracic trauma had a sensitivity of 94% and specificity of 100% for the diagnosis of pneumothorax with chest CT as the "gold standard." Kirkpatrick et al (19) suggested that ultrasound is more sensitive than supine anteroposterior chest radiography in the detection of small pneumothoraces.
We hypothesized that the gliding sign would also be absent if pleurodesis was present. In this situation, the fusion of the visceral and parietal pleural should prevent the pleural surfaces from gliding over each other. Our hypothesis was confirmed in the present study showing a high correlation between the pleurodesis score and the total gliding sign score.
There was a definite learning curve in assessing pleurodesis via ultrasound in the present study. In our initial studies, we found that the gliding sign was difficult to evaluate when the rabbit breathed very rapidly. Subsequently, we found that the evaluation was more easily performed when the animal was administered light anesthesia, resulting in a lower respiration rate. We also noted the gliding sign was falsely present when the examination was performed too close to the diaphragm. The movement of the diaphragm made it appear that the gliding sign was present. As our experience in assessing pleurodesis with ultrasound increased, we noted closer correlations between the gliding sign score and the pleurodesis score. In one rabbit, a gliding sign was present at both the lateral and posterior sites, but was definitely absent at the anterior site. At death, pleural symphysis was present only at the anterior aspect of the hemithorax.
We believe the results of this study have significant clinical implications. Management of recurrent pleural effusion and pneumothorax is a common clinical problem. These conditions are frequently treated by an attempt to create a pleurodesis. Until recently, there has been no effective way to demonstrate the presence of pleurodesis with imaging studies. The present study demonstrates that ultrasound is effective in demonstrating pleurodesis in rabbits. If, indeed, pleurodesis can be demonstrated in humans by ultrasound, it could have multiple applications, such as (1) to assess whether pleurodesis is present in patients treated with various sclerosing agents for pneumothorax or recurrent pleural effusion, (2) to compare the effectiveness of various sclerosing agents, (3) to compare the speed with which various sclerosing agents produce a pleurodesis, and (4) to assess whether a pleurodesis is present before thoracoscopy is attempted.
There are several limitations to our study. It should be noted the evaluation for pleurodesis by ultrasound is dependent on the skill of the operator. In the present study, the results improved as we became more experienced. Nevertheless, we believe that the technique is easily learned by nonradiologists. Another possible difficulty is evaluating pleurodesis in the obese patients. In a recent study (20) of ICU patients in whom ultrasound was used to identify pleural fluid, difficulties were encountered in obese patients. It should be noted that the gliding sign is also absent with pneumothorax, and accordingly pneumothorax could be misdiagnosed as pleurodesis. We feel that this is unlikely, however, since the air with a pneumothorax is in the superior part of the chest. Another limitation is that pleurodesis could not be assessed within a few centimeters of the diaphragm. We feel that this will not be a significant problem in humans because their chest cavities are so much larger.
In conclusion, this study showed the absence of pleural gliding as evaluated by ultrasound correlates well with the presence of a pleurodesis in rabbits. To assess the gliding sign accurately, one should make sure the examined subject breathes slowly, and avoid evaluating the pleural gliding sign too close to the diaphragm.
ACKNOWLEDGMENT: We thank the Genzyme Corporation (Framingham, MA) for providing the TGF-[[beta].sub.2] used in these experiments.
REFERENCES
(1) Light RW. Pleural diseases. 3rd ed. Philadelphia, PA: Lippincott, Williams and Wilkins, 2000
(2) Light RW, Vargas FS. Pleural sclerosis for the treatment of pneumothorax and pleural effusion. Lung 1997; 175:213-223
(3) Yang PC. Application of colour Doppler ultrasound in the diagnosis of chest diseases. Respirology, 1997; 2:281-288
(4) Beckh S, Bolcskei PL, Lessnau KD. Real-time chest ultrasonography: a comprehensive review for the pulmonologist. Chest 2002; 122:1759-1778
(5) Wernecke K. Ultrasound study of the pleura. Eur Radiol 2000; 10:1515-1523
(6) Mathis G. Thorax sonography: part 1. Chest wall and pleura. Ultrasound Med Biol 1997; 23:1131-1139
(7) Tsai TH, Yang PC. Ultrasound in the diagnosis and management of pleural disease. Curr Opin Pulm Med 2008; 9:282-290
(8) Lichenstein DA, Menu Y. A beside ultrasound sign ruling out pneumothorax in the critically ill: lung sliding. Chest 1995; 108:1345-1348
(9) Eibenberger KL, Dock WI, Ammann ME. Quantification of pleural effusion: sonography versus radiography. Radiology 1994; 191:681-684
(10) Chan SS. Emergency bedside ultrasound to detect pneumothorax. Acad Emerg Med 2003; 10:91-94
(11) Dulchavsky SA, Schwarz KL, Kirkpatirck AW, et al. Prospective evaluation of thoracic ultrasound in the detection of pneumothorax. J Trauma 2001 Feb; 50:201-205
(12) Rowan KR, Kirkpatrick AW, Lie D, et al. Traumatic pneumothorax: detection with thoracic US; correlation with chest radiography and CT-initial experience. Radiology 2002; 225:210-214
(13) Light RW, Cheng DS, Lee YCG, et al. A single intrapleural injection of transforming growth factor [beta]-2 produces an excellent pleurodesis in rabbits. Am J Respir Crit Care Med 2000; 162:98-104
(14) Lee YCG, Teixeira LR, Devin CJ, et al. Transforming growth factor-[[beta].sub.2] induces pleurodesis significantly faster than talc. Am J Respir Crit Care Med 2000; 163:640-644
(15) American Thoracic Society. Management of malignant pleural effusion. Am J Respir Crit Care Med 2000; 162:1987-2001
(16) Webb WR, Higgins CB. Thoracic imaging: pulmonary and cardiovascular radiology. Philadelphia, PA: Lippincott, Williams and Wilkins, 2004
(17) Reuss J. Sonographic imaging of the pleura: nearly 30 years experience. Eur J Ultrasound 1996; 3:125-139
(18) Soldati G, Iacconi P. The validity of the use of ultrasonography in the diagnosis of spontaneous and traumatic pneumothorax, J Trauma 2001; 51:423
(19) Kirkpatrick AW, Ng AKT, Dulchavsky SA, et al. Sonographic diagnosis of a pneumothorax inapparent on plain radiography: confirmation by computed tomography. J Trauma 2001; 50:750-752
(20) Mayo PH, Goltz HR, Tafreshi M, et al. Safety of ultrasound-guided thoracentesis in patients receiving mechanical ventilation. Chest 2004; 125:1059-1062
* From the Division of Allergy, Critical Care, and Pulmonary Disease (Drs. Dikensoy, Misra, Bilaceroglu, Lane, and Light), Vanderbilt University and Saint Thomas Hospital, Nashville, TN; the Department of Radiology and Radiological Sciences (Dr. Donnelly), Vanderbilt University, Nashville, TN; and the Department of Pulmonary and Critical Care Medicine (Dr. Zhu), The First Affiliated Hospital of Zhongshan (Sun Yat-Sen) University, Guangzhou, ROC.
Supported by the Saint Thomas Foundation, Nashville, TN. Manuscript received December 9, 2004; revision accepted January 21, 2005.
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (www.chestjournal. org/misc/reprints.shtml).
Correspondence to: Richard W. Light, MD, FCCP, Director of Pulmonary Disease Program, Saint Thomas Hospital, 4220 Harding Rd, Nashville, TN 37205; e-mail: rlight98@yahoo.com
COPYRIGHT 2005 American College of Chest Physicians
COPYRIGHT 2005 Gale Group