Instructions
This booklet is designed to be used with forms that you can personalize to meet your individual needs. To use the forms, print them out.
If you do not have a printer, or would rather complete the forms using a printed booklet, please contact the NDIC Information Clearinghouse at ndic@info.niddk.nih.gov and request a copy of the booklet, Medicines for People with Diabetes.
Contents
* Find Your Diabetes Medicines
* Do I Need To Take Diabetes Medicine?
* Why Do I Need Medicines for Type 1 Diabetes?
* Why Do I Need Medicines for Type 2 Diabetes?
* What Are the Four Types of Diabetes Pills?
* What Do I Need To Know About Insulin?
* Might I Take More Than One Diabetes Medicine At a Time?
* What Should I Know About Low Blood Sugar?
* How Do I Know if My Diabetes Medicines Are Working?
* How To Find More Help
* Acknowledgments
(*) Information about the diabetes medicines in this booklet is current as of November 1998. In the future, information about these diabetes medicines may change and new diabetes medicines will be approved. We will update this document as changes are made.
Do I need to take diabetes medicine?
What if I have type 1 diabetes?
Type 1 is the type of diabetes that people most often get before 30 years of age. All people with type 1 diabetes need to take insulin (IN-suh-lin) because their bodies do not make enough insulin. Insulin helps turn sugar from food into energy for the body to work.
What if I have type 2 diabetes?
Type 2 is the type of diabetes most people get as adults after the age of 40. But you can get diabetes at a younger age.
Healthy eating, exercise, and losing weight may help you lower your blood sugar (also called blood glucose) when you find out you have type 2 diabetes. If these treatments do not work, you may need one or more types of diabetes pills to lower your blood sugar. After a few more years, you may need to take insulin shots because your body is not making enough insulin.
You, your doctor, and your diabetes teacher should always find the best diabetes plan for you.
Why do I need medicines for type 1 diabetes?
Most people make insulin in their pancreas. If you have type 1 diabetes, your body does not make insulin. Insulin helps sugar from the foods you eat get to all parts of your body and be used for energy.
Because your body no longer makes insulin, you need to take insulin in shots. Take your insulin as your doctor tells you. The section, What Do I Need to Know About Insulin?, provides more information on insulin.
Why do I need medicines for type 2 diabetes?
If you have type 2 diabetes, your pancreas usually makes plenty of insulin. But your body cannot correctly use the insulin you make. You might get this type of diabetes if members of your family have or had diabetes. You might also get type 2 diabetes if you weigh too much or do not exercise enough.
After you have had type 2 diabetes for a few years, your body may stop making enough insulin. Then you will need to take diabetes pills or insulin.
You Need To Know:
* Diabetes medicines that lower blood sugar never take the place of healthy eating and exercise.
* If your blood sugar gets too low more than a few times in a few days, call your doctor.
* Take your diabetes pills or insulin even if you are sick. If you cannot eat much, call your doctor.
What are the types of diabetes pills?
Many types of diabetes pills can help people with type 2 diabetes lower their blood sugar. Each type of pill helps lower blood sugar in a different way. The diabetes pill (or pills) you take is from one of these groups. You might know your pill (or pills) by a different name.
* Sulfonylureas (SUL-fah-nil-YOO-ree-ahs). Stimulate your pancreas to make more insulin.
* Biguanides (by-GWAN-ides). Decrease the amount of sugar made by your liver.
* Alpha-glucosidase inhibitors (AL-fa gloo-KOS-ih-dayss in-HIB-it-ers). Slow the absorption of starches you eat.
* Meglitinides (meh-GLIT-in-ides). Stimulate your pancreas to make more insulin.
* Thiazolidinediones (THIGH-ah-ZO-li-deen-DYE-owns). Make you more sensitive to insulin.
Your doctor might prescribe one pill. If the pill does not lower your blood sugar, your doctor may
* Ask you to take more of the same pills, or
* Add a new pill or insulin, or
* Ask you to change to another pill or insulin.
Fill out a medicine planning form.
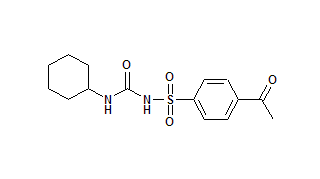
Sulfonylureas
These pills do two things:
* They help your pancreas make more insulin, which then lowers your blood sugar.
* They help your body use the insulin it makes to better lower your blood sugar.
For these pills to work, your pancreas has to make some insulin. Sulfonylureas can make your blood sugar too low, which is called hypoglycemia (HY-po-gly-SEE-mee-ah). The section, What Should I Know About Low Blood Sugar, provides more information on low blood sugar.
How often should I take sulfonylureas?
Some sulfonylureas work all day, so you take them only once a day. Others you take twice a day. Your doctor will tell you how many times a day you should take your diabetes pill(s). Ask if you are not sure.
When should I take sulfonylureas?
The time you take your pill depends on which pill you take and what your doctor tells you. If you take the pill once a day, you will likely take it just before the first meal of the day (breakfast). If you take the medicine twice a day, you will likely take the first pill just before your first meal, and the second pill just before the last meal of the day (supper). Take the medicine at the same times each day. Ask your doctor when you should take your pills.
What are possible side effects of sulfonylureas?
* A low blood sugar reaction (hypoglycemia).
* An upset stomach.
* A skin rash or itching.
* Weight gain.
What Are Side Effects?
* Side effects are changes that may happen in your body when you take a medicine. When your doctor gives you a new medicine, ask what the side effects might be.
* Some side effects happen just when you start to take the medicine. Then they go away.
* Some side effects happen only once in a while. You may get used to them or learn how to manage them.
* Some side effects will cause you to stop taking the medicine. Your doctor may try another one that doesn't cause you side effects.
Biguanides
Biguanides are another type of diabetes medicine. Metformin (met-FOR-rain) is a biguanide that helps lower blood sugar by making sure your liver does not make too much sugar. Metformin also lowers the amount of insulin in your body.
You may lose a few pounds when you start to take metformin. This weight loss can help you control your blood glucose. Metformin can also improve blood fat and cholesterol levels, which are often not normal if you have type 2 diabetes.
A good thing about metformin is that it does not cause blood sugar to get too low (hypoglycemia) when it is the only diabetes medicine you take.
How often should I take metformin?
Two or three times a day.
When should I take metformin?
With a meal. Your doctor should tell you which meals to take it with.
What are possible side effects?
Taking metformin might cause
* Metformin can make you sick if you drink more than about 2 to 4 alcoholic drinks a week. If you drink more than that, tell your doctor. You should probably not take metformin.
* If you already have a kidney problem, taking metformin may make it worse. Make sure that, before you start taking metformin, your doctor knows your kidneys work well.
* If you are vomiting, have diarrhea, and can't drink enough fluids, you may need to stop taking metformin for a few days.
* Once in a while people on metformin can become weak, tired, or dizzy and have trouble breathing. If you ever have these problems, call your doctor or get medical help right away.
* You may have nausea, diarrhea, and other stomach symptoms when you first start taking metformin. These usually go away.
* You may notice a metallic taste in your mouth.
What To Know About Having Surgery or Medical Tests with Dye:
* If you are having surgery, tell the doctor you take metformin. You should be told to stop taking metformin the day of the surgery. Then you should not take metformin again until you are eating and your kidney are working normally.
* If you are having a medical test with dye, tell the doctor you take metformin. You may be told to stop taking metformin the day of the test and not take metformin again for 48 hours.
Alpha-glucosidase inhibitors
There are now two alpha-glucosidase inhibitors, acarbose (AK-er-bose) and miglitol (MIG-leh-tall). Both medicines block the enzymes that digest the starches you eat. This action causes a slower and lower rise of blood sugar through the day, but mainly right after meals.
Neither acarbose nor miglitol causes blood sugar to get too low (hypoglycemia) when it is the only diabetes medicine you take.
How often should I take acarbose or miglitol
Three times a day, at each meal. Your doctor might ask you to take the medicine less often at first.
When should I take acarbose or miglitol?
With the first bite of a meal.
What are possible side effects?
Taking this pill may cause stomach problems (gas, bloating, and diarrhea) that most often go away after you take the medicine for a while.
Thiazolidinediones
This type of medicine helps your muscles make better use of your insulin. The only medicine now in this group is called troglitazone (tro-GLIT-uh-zone).
Troglitazone doesn't cause blood sugar to get too low when it is the only diabetes medicine you take.
How often should I take troglitazone?
Usually once a day.
When should I take troglitazone?
With the same meal at the same time each day. Ask your doctor when you should take it. Your body uses this medicine best if you take it with your largest meal of the day.
What are possible side effects of troglitazone?
* Most people can take troglitazone without any side effects. A small number of people may get liver problems or liver failure from troglitazone. Before you start taking troglitazone, your doctor should do a test to make sure your liver is healthy. If you start taking troglitazone, your doctor should regularly check how your liver is working.
* If you take birth control pills, you should know that troglitazone might make your birth control pills less effective in preventing pregnancy. Make sure your doctor knows that you take birth control pills.
You Need To Know
* Do not change or stop taking your diabetes medicine without first talking to your doctor.
* Your doctor might ask you to switch from pills to insulin shots if your pancreas stops making enough insulin.
Meglitinides
Meglitinides (meh-GLIT-in-ides) are a new type of diabetes medicine. Repaglinide (re-PAG-lyn-ide) is the name of a meglitinide. This medicine helps your pancreas make more insulin right after meals, which lowers blood sugar. Your doctor might prescribe repaglinide by itself or with metformin (another diabetes medicine) if one medicine alone does not control your blood sugar levels.
A good thing about repaglinide is that it works fast and your body uses it quickly. This fast action means you can vary the times you eat and the number of meals you eat more easily using repaglinide than you can using other diabetes medicines.
How often should I take repaglinide?
Your doctor will tell you to take repaglinide before you eat a meal. If you skip a meal, you should not take the dose of repaglinide.
When should I take repaglinide?
From 30 minutes before to just before a meal. Repaglinide lowers blood sugar the most 1 hour after you take it, and it is out of the bloodstream in 3 to 4 hours.
What are possible side effects of repaglinide?
* A low blood glucose reaction (hypoglycemia).
* Weight gain. What do I need to know about insulin?
If your pancreas no longer makes enough insulin, then you need to take insulin as a shot. You inject the insulin just under the skin with a small, short needle. You cannot take insulin as a pill.
Why can't I take insulin as a pill?
Insulin is a protein. If you took insulin as a pill, your body would break it down and digest it before it got into your blood to lower your blood sugar.
How does insulin work?
Insulin lowers blood sugar by moving sugar from the blood into the cells of your body. Once inside the cells, sugar provides energy. Insulin lowers your blood sugar whether you eat or not. You should eat on time if you take insulin.
How often should I take insulin?
Most people with diabetes need at least two insulin shots a day for good blood sugar control. Some people take three or four shots a day to have a more flexible diabetes plan.
When should I take insulin?
You should take insulin 30 minutes before a meal if you take regular insulin alone or with a longer-acting insulin. If you take insulin lispro (Humalog), an insulin that works very quickly, you should take your shot just before you eat.
Are there several types of insulin?
Yes. There are five main types of insulin. They each work at different speeds. Many people take two types of insulin.
The five types of insulin are
Quick acting, insulin lispro (Humalog) Starts working in 5 to 15 minutes. Lowers blood sugar most in 45 to 90 minutes. Finishes working in 3 to 4 hours.
Short acting, Regular (R) insulin Starts working in 30 minutes. Lowers blood sugar most in 2 to 5 hours. Finishes working in 5 to 8 hours.
Intermediate acting, NPH (N) or Lente (L) insulin Starts working in 1 to 3 hours. Lowers blood sugar most in 6 to 12 hours. Finishes working in 16 to 24 hours.
Long acting, Ultralente (U) insulin Starts working in 4 to 6 hours. Lowers blood sugar most in 8 to 20 hours. Finishes working in 24 to 28 hours.
NPH and Regular insulin mixture Two types of insulins mixed together in one bottle. Starts working in 30 minutes. Lowers blood sugar most in 7 to 12 hours. Finishes working in 16 to 24 hours.
Does insulin work the same all the time?
After a short time, you will get to know when your insulin starts to work, when it works its hardest to lower blood sugar, and when it finishes working.
You will learn to match your mealtimes and exercise times to the time when each insulin you take works in your body.
How quickly or slowly insulin works in your body depends on
* Your own response.
* The place on your body where you inject insulin.
* The type and amount of exercise you do and the length of time between your shot and exercise.
Where on my body should I inject insulin?
You can inject insulin into several places on your body. Insulin injected near the stomach works fastest. Insulin injected into the thigh works slowest. Insulin injected into the arm works at medium speed. Ask your doctor or diabetes teacher to show you the right way to take insulin and in which parts of the body to inject it.
How should I store insulin?
* If you use a whole bottle of insulin within 30 days, keep that bottle of insulin at room temperature. On the label, write the date that is 30 days away. That is when you should throw out the bottle with any insulin left in it.
* If you do not use a whole bottle of insulin within 30 days, then store it in the refrigerator all the time.
* If insulin gets too hot or cold, it breaks down and does not work. So, do not keep insulin in very cold places such as the freezer, or in hot places, such as by a window or in the car's glove compartment during warm weather.
* Keep at least one extra bottle of each type of insulin you use in your house. Store extra insulin in the refrigerator.
What Are Possible Side Effects of Insulin?
* A low blood sugar reaction (hypoglycemia).
* Weight gain.
Might I take more than one diabetes medicine at a time?
Yes. Your doctor may ask you to take more than one diabetes medicine at a time. Some diabetes medicines that lower blood sugar work well together. Here are examples:
Two diabetes pills
If one type of pill alone does not control your blood sugar, then your doctor might ask you to take two kinds of pills. Each type of pill has its own way of acting to lower blood sugar. Here are pills used together:
* A sulfonylurea and metformin.
* A sulfonylurea and acarbose.
* Metformin and acarbose.
* Repaglinide and metformin.
Diabetes pills and insulin
Your doctor might ask you to take insulin and one of these diabetes pills:
* Insulin and a sulfonylurea. * Insulin and metformin.
* Insulin and troglitazone.
What should I know about low blood sugar?
Sulfonylureas, meglitinides, and insulin are the types of diabetes medicines that can make blood sugar go too low. Low blood sugar can happen for many reasons:
* Delaying or skipping a meal.
* Eating too little food at a meal.
* Getting more exercise than usual.
* Taking too much diabetes medicine.
* Drinking alcohol.
You know your blood sugar may be low when you feel one or more of the following:
* Dizzy or light-headed.
* Hungry.
* Nervous and shaky.
* Sleepy or confused.
* Sweaty.
If you think your blood sugar is low, test it to see for sure. If your blood sugar is at or below 70 mg/dl, eat one of these items to get 15 grams of carbohydrate:
* 1/2 cup (4 oz.) of any fruit juice.
* 1 cup (8 oz.) of fat-free or low-fat milk.
* 4 teaspoons of granulated white sugar.
* 1/3 cup (3 oz.) regular soda.
* 6 to 7 small Lifesavers[R] or 4 large Lifesavers[R].
* Glucose gel or tablets (take the amount noted on package to add up to 15 grams of carbohydrate).
Test your blood sugar again 15 minutes later. If it is still below 70 mg/dl, then eat another 15 grams of carbohydrate. Then test your blood sugar again in 15 minutes.
If you cannot test your blood sugar right away but you feel symptoms of low blood sugar, eat one of the items listed above.
If your blood sugar is not low, but you will not eat your next meal for at least an hour, then have a snack with starch and protein. Here are some examples:
* Crackers and peanut butter or cheese.
* Half of a ham or turkey sandwich.
* A cup of milk and crackers or cereal.
Fill out a medicine planning form.
How do I know if my diabetes medicines are working?
Learn to test your blood sugar. Ask your doctor or diabetes teacher about the best testing tools for you and how often to test. After you test your blood sugar, write down your blood sugar test results. Then ask your doctor or diabetes teacher if your diabetes medicines are working. A good blood sugar reading before meals is between 70 and 140 mg/dl.
Ask your doctor or diabetes teacher about how low or how high your blood sugar should get before you take action. For many people, blood sugar is too low below 70 mg/dl and too high above 240 mg/dl.
One other number to know is the result of a blood test your doctor does called hemoglobin A1c (HE-muh-glow-bin A-1-C) or glycated hemoglobin (GLY-kay-ted HE-muh-glow-bin). It shows your blood sugar control during the last 2 to 3 months. For most people, a good hemoglobin A1c is 7 percent.
How To Find More Help
Diabetes Teachers (nurses, dietitians, pharmacists, and other health professionals)
* To find a diabetes teacher near you, call the American Association of Diabetes Educators toll-free at 1-800-TEAMUP4 (1-800-832-6874).
Recognized Diabetes Education Programs (teaching programs approved by the American Diabetes Association)
* To find a program near you, call 1-800-DIABETES (1-800-342-2383) or look at its Internet home page http://www.diabetes.org and click on "Diabetes Info."
Dietitians
* To find a dietitian near you, call The American Dietetic Association's National Center for Nutrition and Dietetics at 1-800-366-1655 or look at its Internet home page http://www.eatright.org and click on "Find a Dietitian."
Acknowledgments
The individuals listed here provided editorial guidance or facilitated field testing for this publication. The National Diabetes Information Clearinghouse would like to thank these individuals for their contributions.
American Association of Diabetes Educators Chicago, IL
Shelly Amos, L.R.D. Nez Perce Nutrition Lapwai, ID
Noreen Cohen, M.S., R.D., L.D. Humana Health Care Plans San Antonio, TX
Paula Dubcak, R.N., C.D.E. Humana Health Care Plans San Antonio, TX
Lois Exelbert, R.N., M.S., C.D.E., A.C.C.E. Joslin Center for Diabetes Baptist Hospital of Miami Miami, FL
Ruth Farkas-Hirsch, R.N., M.S., C.D.E. (on behalf of American Diabetes Association) University of Washington, Diabetes Care Center Seattle, WA
Lawana Geren, R.N., C.D.E. Humana Health Care Plans San Antonio, TX
Gwen Hosey, M.S., A.N.P., C.D.E. IHS Portland Area Diabetes Program at Washington Bellingham, WA
Joslin Center for Diabetes Community Medical Center Toms River, NJ
Melinda Maryniuk, M.Ed., R.D., C.D.E. Joslin Diabetes Center Boston, MA
Pat Mathis, M.S., R.N., C.D.E. Marianne Sack, R.N., C.D.E. So Others Might Eat Washington, DC
Kathy O'Keeffe, M.S., R.D., L.D., C.D.E. Carolina Diabetes and Kidney Center Sumter, SC
Carolyn Ross, R.D., M.S., C.D.E. PHS Indian Hospital Cass Lake, MN
Lisa Spence, M.S. Purdue University West Lafayette, IN
Judy Tomassene, M.P.H., M.S., R.D. Seattle Indian Health Board Seattle, WA
Madelyn L. Wheeler, M.S., R.D., F.A.D.A., C.D.E. Indiana University School of Medicine Diabetes Research and Training Center Indianapolis, IN
National Diabetes Information Clearinghouse
1 Information Way Bethesda, MD 20892-3560 E-mail: ndic@info.niddk.nih.gov
The National Diabetes Information Clearinghouse (NDIC) is a service of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). The NIDDK is part of the National Institutes of Health under the U.S. Public Health Service. Established in 1978, the clearinghouse provides information about diabetes to people with diabetes and their families, health care professionals, and the public. NDIC answers inquiries; develops, reviews, and distributes publications; and works closely with professional and patient organizations and government agencies to coordinate resources about diabetes.
Publications produced by the clearinghouse are reviewed carefully for scientific accuracy, content, and readability.
This e-text is not copyrighted. The clearinghouse encourages users of this e-pub to duplicate and distribute as many copies as desired.
NIH Publication No. 99-4222 January 1999
e-text last updated: February 1999
COPYRIGHT 1999 National Institute of Diabetes & Digestive & Kidney Diseases
COPYRIGHT 2004 Gale Group