Comparison With an Acetylcholine Test
Study objectives: This study was performed to compare the results of accelerated exercise following mild hyperventilation and a standard acetylcholine (ACh) test for the induction of coronary artery spasm in patients with drug-induced coronary artery spasm. Methods and results: The subjects were 74 patients with angiographically confirmed coronary artery spasm who were examined using accelerated exercise (ie, exercise that was accelerated every minute according to the protocol of Bruce and Horsten) following mild hyperventilation and who were not receiving any medication. ACh was injected in incremental doses of 20 [micro]g and 50 [micro]g into the right coronary artery and incremental doses of 20 [micro]g, 50 [micro]g, and 100 [micro]g into the left coronary artery. Positive coronary spasm was defined as [is greater than or equal to] 99% luminal narrowing. Accelerated exercise following a mild hyperventilation test was as useful for detecting evidence of ischemia as was an ACh test (48 patients [64.9%] vs 49 patients [66.2%], respectively; not significant). No difference was observed between ischemic changes on ECG as a result of the newly combined method and the occurrence of ACh-induced spasm. ACh-induced coronary vasospasm occurred in 61 patients (82.4%). In the remaining 13 patients, intracoronary administration of ergonovine provoked coronary spasms. No serious irreversible complications were detected as a result of this newly combined method.
Conclusions: The effectiveness of our newly combined procedure is equivalent to that of an ACh test to diagnose patients with coronary artery spasm.
(CHEST 2001; 119:155-162)
Key words: accelerated exercise; acetylcholine; coronary spastic angina; hyperventilation
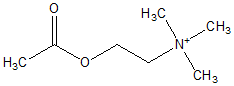
Abbreviations: ACh = acetylcholine; HV + TM = mild hyperventilation followed by accelerated treadmill exercise
Several noninvasive procedures for the induction of coronary artery spasm, such as hyperventilation, cold stress, and exercise tests, have been clinically employed,[1-8] However, coronary artery spasm is diagnosed by angiography. Acetylcholine (ACh) and ergonovine are effective for the demonstration of coronary artery spasm in the cardiac laboratory.[9-12] The ACh test, compared to tests with ergonovine, has the advantages of transient pharmacologic reaction, spontaneous relief without the administration of isosorbide dinitrate in most cases, and detection of multiple spasms.
Noninvasive procedures may demonstrate ischemic changes in patients with variant angina, but it is difficult to diagnose coronary artery spasm and non-variant angina with these procedures.
This study was performed to compare the clinical usefulness of our newly combined noninvasive procedure (ie, mild hyperventilation followed by accelerated treadmill exercise[13-15] [HV + TM]) and an invasive ACh test in patients with drug-induced coronary artery spasm and nonvariant angina.
MATERIALS AND METHODS
Study Patients
Between July 1993 and June 1998, we systematically performed spasm provocation tests with ACh and accelerated exercise following a hyperventilation test in patients with coronary spastic angina. During this period, 141 consecutive patients received diagnoses of coronary spastic angina by intracoronary administration of either ACh or ergonovine. From this group of patients, we excluded 57, a group comprising 10 patients who had undergone ergonovine testing alone, 20 patients who had spontaneous ST-segment elevation, and 27 patients who had luminal narrowings of [is greater than] 90%. Before starting the study, the hyperventilation test, with a frequency rate of 24 to 30 breaths/min for 5 min, was performed in the morning between 9:00 AM and 11:00 AM without the administration of medication. Ten patients with coronary spastic angina had ischemic ECG changes during and/or after hyperventilation tests, and we excluded these 10 patients from this study. Thus, we examined 74 consecutive patients with angiographically confirmed coronary artery spasm, and no patients had spontaneous ST-segment elevation before the study. These patients were divided into two groups. The organic stenosis group (stenosis, [is greater than or equal to] 75%) consisted of 24 patients (23 men and 1 woman; mean [[+ or -] SD] age, 63.2 [+ or -] 6.3 years; age range, 48 to 74 years). The nonorganic stenosis group (stenosis, [is less than] 75%) consisted of 50 patients (45 men and 5 women; mean age, 61.6 [+ or -] 8.7 years; age range, 33 to 78 years). The subjects were studied to determine the sensitivity of the two spasm provocation tests. All 74 patients exhibited attacks of chest pain while at rest, especially at night or in the early morning, and they sometimes complained of chest pain on effort during daily life. Before the study, 24-h Holter monitoring was performed in all 74 patients. Moreover, we tried to perform the ECG during chest pain attacks while patients were in the hospital, if possible. As a control group, the HV + TM test was performed in 46 patients (20 men and 26 women; mean age, 61.9 [+ or -] 8.2 years; age range, 40 to 72 years) who had normal or near-normal coronary arteries and who did not experience a coronary spasm as a result of the intracoronary administration of ACh. All 46 patients were studied because they had experienced chest pain or discomfort at rest and/or during exercise.
The diagnosis of coronary spastic angina was made in patients meeting all of the following criteria: (1) retrosternal burning or squeezing chest pain accompanied with cold sweating mainly at rest; (2) rapid relief of pain ([is less than] 5 min) after the administration of sublingual nitroglycerine; and (3) drug-induced coronary artery spasm ([is greater than or equal to] 99%).
Table 1 shows the coronary artery lesions detected by coronary arteriography after the administration of nitroglycerine in both groups. In the organic stenosis group, 20 patients had one-vessel disease, 4 patients had two-vessel disease, and none had three-vessel disease or [is greater than] 90% stenosis. No patients had a history of myocardial infarction or heart failure. Al drugs, except for nitroglycerine, were discontinued for [is greater than or equal to] 24 h before the study began, and nitroglycerine also was discontinued [is greater than or equal to] 6 h before the study began. There were no differences concerning risk factors between the two groups. However, the rate of habitual smoking was significantly higher than other risk factors in both groups. According to the assessment of attack frequency before the administration of a calcium antagonist, in this study we subdivided the patients into the following three groups: (1) sporadic anginal attack (ie, less than one attack per month), defined as low disease activity; (2) more than or equal to one attack but less than four attacks per month, defined as moderate disease activity; and (3) more than or equal to four attacks per month, defined as high disease activity. No patients had more than or equal to two sporadic anginal attacks per day. Overall, more than half of the patients studied had low disease activity.
[TABULAR DATA 1 NOT REPRODUCIBLE IN ASCII]
Written informed consent was obtained from all patients before the study, and the protocol of this study was in agreement with the guidelines of the ethics committees at our institutions.
Spasm Provocation Test
As previously reported,[16] patients were excluded and the spasm provocation test was not performed if patients had left main narrowing (ie, [is greater than] 50%), three-vessel disease, two-vessel disease with total occlusion, heart failure (New York Heart Association functional class III or IV), and renal failure (creatinine level, [is greater than] 2.0 mg/dL), or if isosorbide dinitrate was initially used to relieve the spasm in the coronary artery tested.
Coronary arteriography was performed in the fasting state with the Sones technique through the brachial artery between 10:00 AM and 4:00 PM without the patient receiving medication for 24 h, except for nitroglycerine, which was stopped 6 h before the study began. Control coronary arteriography of the left coronary artery was performed in the right anterior oblique with caudal projection, and arteriography of the right coronary artery was performed in the left anterior oblique with cranial projection; visualization was aided by the injection of 8 to 10 mL Iopamiron (Schering; Bracco, Italy). A bipolar electrode catheter (USCI-Bard; Billerica, MA) was inserted into the right ventricular apex through the femoral or antecubital vein and was connected to a temporary pacemaker set at a rate of 45 beats/min.
Provocation of coronary spasm was performed with an intracoronary injection of ACh. ACh chloride (Zeria Seiyaku; Tokyo, Japan), 30 mg/2 mL, dissolved in warm 0.9% saline solution was administered over 20 s. ACh was injected in incremental doses of 20 [micro]g and 50 [micro]g into the right coronary artery and in incremental doses of 20 [micro]g, 50 [micro]g, and 100 [micro]g into the left coronary artery with at least a 3-min interval between each injection. Coronary arteriography was performed when ST-segment changes, chest pain, or both occurred or when 1 min had elapsed after the completion of each injection. Intracoronary injection of ACh into the responsible vessel was not performed if a coronary spasm occurred spontaneously during coronary angiography. When ACh did not provoke spasm, intracoronary injection of ergonovine then was administered 10 min after the last ACh test. Ergonovine (Fuji Rebio; Tokyo, Japan), 0.2 mg/mL, in 0.9% warm saline solution was slowly injected into the right coronary artery with a maximal dose of 40 [micro]g/40 mL and into the left coronary artery with a maximal dose of 64 [micro]g/64 mL over 4 min. Coronary arteriography was performed when significant ST-segment changes, chest pain, or both developed or when 6 min had elapsed after the initiation of each injection. The time interval between each injection was [is greater than] 5 min. When coronary spasm was provoked and did not spontaneously resolve within 3 min after the completion of ACh and ergonovine injection, or when hemodynamic instability due to coronary spasm occurred, 2.5 to 5.0 mg of isosorbide dinitrate was administered into the responsible vessel. In all patients, coronary arteriography after the administration of 2.5 to 5.0 mg of isosorbide dinitrate was performed in multiple projections at the end of the study to estimate atherosclerotic lesions.
The percentage of luminal diameter narrowing of coronary arteries was measured by an automatic edge-contour detection computer analysis system (CARDIO 500; Kontron Instrument; Tokyo, Japan). The size of the coronary catheter was used to calibrate the image (in millimeters), and the measurement was performed in the same projection of coronary angiography at each stage. A positive coronary spasm was defined as [is greater than or equal to] 99% luminal narrowing. A focal spasm was defined as a discrete transient vessel narrowing localized in the major coronary artery of [is greater than or equal to] 99%. A diffuse spasm was diagnosed when a transient vessel narrowing of [is greater than or equal to] 99% compared with the baseline coronary angiography was observed from the proximal to distal segment in the three major coronary arteries. Catheter-induced coronary spasms were excluded from this study. The arterial segment of coronary arteries and the percentage of luminal diameter narrowing were determined according to the classification of the American Heart Association committee report.[17] The degree of ST-segment depression was measured 80 ms after the J point. We considered a result to be positive when at least one of the following ischemic ECG changes was demonstrated during and/or after the ACh test: (1) ST-segment elevation of [is greater than or equal to] 0.2 mV in at least two related leads; or (2) ST-segment depression of 0.1 mV of a horizontal or downsloping type or [is greater than or equal to] 0.2 mV of a junctional type.
During the study, arterial BP and one ECG lead (ie, lead II) were continuously monitored on an oscilloscope with a polygraph (Nihon Kohden; Tokyo, Japan). A standard 12-lead ECG was recorded every 30 s with a radiolucent carbon electrode used as the chest lead electrode.
HV + TM
All forms of medication were discontinued at least 24 h before the study began except for sublingual nitroglycerine, which was stopped at least 6 h before the procedures. After recording a baseline measurement for the 12-lead ECG and for BP, the newly combined HV + TM protocol, which consisted of 5 min of mild hyperventilation with a frequency rate of 24 to 30 breaths/ min followed by a modified treadmill exercise test the acceleration of which was increased every minute according to the protocol of Bruce and Horsten,[18] was performed between 9:00 AM and 11:00 AM within a week before or after the cardiac catheterization procedure. During the tests, 12-lead ECG was continuously monitored with an oscilloscope and BP was measured with a cuff sphygmomanometer at 1-min intervals. When angina was provoked, sublingual nitroglycerine (0.3 mg) was administered. The 12-lead ECG was recorded at 1-min intervals for 10 min after the procedures. The degree of ST-segment depression was measured 80 ms after the J point. The test result was considered positive when at least one of the following ischemic ECG changes was demonstrated: (1) ST-segment elevation of [is greater than or equal to] 0.2 mV in at least two related leads during and/or after the procedure; or (2) ST-segment depression of [is greater than or equal to] 0.1 mV of a horizontal or downsloping type, or [is greater than or equal to] 0.2 mV of a junctional type, during and/or after the procedure.
For pH and gas analysis, arterial blood samples were taken before and after hyperventilation from 12 patients and were measured with an autoanalyzer (COMPACT 2; AVL; Graz, Austria).
Data Analysis
All data were presented as the mean [+ or -] SD. The [chi square] test was used for differences in parameters during exercise and for differences in the prevalence of ischemic changes and chest symptoms. A p value [is less than] 0.05 was considered to be statistically significant.
RESULTS
ACh Spasm Provocation Test
As shown in Table 2, in the organic stenosis group 18 patients had 34 vessel spasms that involved 15 right coronary arteries, 6 circumflex arteries, and 13 left anterior descending arteries. Focal spasms were observed in 28 vessels, and diffuse spasms were observed in 6 vessels. Six patients had no spasm following the intracoronary injection of ACh. However, ergonovine induced coronary spasms in all six patients. ACh provoked coronary spasms of the fixed stenosis in 22 of 28 lesions. Coronary spasm was provoked in all fixed lesions by intracoronary injection of either ACh or ergonovine. Coronary spasm also was induced in 12 vessels without fixed stenosis. Moreover, 10 patients with and without fixed lesions had coronary spasms on injection of both ACh and ergonovine. In the nonorganic stenosis group, 43 patients had 89 vessel spasms, while coronary spasm was not induced in 7 patients following the intracoronary injection of ACh. These included 39 right coronary arteries, 17 circumflex arteries, and 33 left anterior descending arteries. Focal spasms were observed in 37 vessels, and diffuse spasms were determined in 52 vessels. The intracoronary injection of ergonovine provoked spasms in the remaining seven patients. In the right coronary artery, in the organic stenosis group, ST-segment elevation in the inferior leads was observed in 12 patients. Twelve patients showed no ST-T changes. The amount of ACh used was 20 [micro]g in 5 patients and 50 [micro]g in 19 patients. In the nonorganic stenosis group, ST-segment elevation in the inferior leads was observed in 19 patients, while ST-segment depression was observed in 5 patients. Twenty-six of these patients demonstrated no ST-T changes. The amount of ACh used was 20 [micro]g in 7 patients and 50 [micro]g in 43 patients. In the left coronary artery, in the organic stenosis group, ST-segment elevations were observed in seven patients. Six patients showed ST-segment depression, and no ST-T changes were observed in 11 patients. The amount of ACh used was 20 [micro]g in 6 patients, 50 [micro]g in 5 patients, and 100 [micro]g in 13 patients. In the nonorganic stenosis group, 12 patients demonstrated ST-segment elevation, 13 patients demonstrated ST-segment depression, and 25 patients had no ST-T changes. Intracoronary injection of 20 [micro]g of ACh was administered to 2 patients, 50 [micro]g was administered to 11 patients, and 100 [micro]g was administered to 37 patients. Chest pain was experienced by 79.2% of patients in the organic stenosis group and by 82.0% of patients in the nonorganic stenosis group.
(*) Values given as No. (%). RCA = right coronary artery; LCX = left circumflex artery; LAD = left anterior descending artery.
HV + TM
No chest pain and no ischemic change occurred before accelerated exercise had begun. In the organic stenosis group, 21 patients (13 patients with ST-segment elevation and 8 with ST-segment depression) exhibited ischemic findings on electrocardiography, as shown in Table 3. On the contrary, in the nonorganic stenosis group, 27 patients (4 patients with ST-segment elevation and 23 with ST-segment depression) showed evidence of ischemia. Chest pain was observed in 21 of 24 patients (87.5%) in the organic stenosis group and in 29 of 50 patients (58.0%) in the nonorganic stenosis group. ST-segment elevation was more frequent in the organic stenosis group, while ST-segment depression was more common in the nonorganic stenosis group. In this study, no patients showed ST-segment elevation in both leads, or in the inferior or anterior leads. In the control group, no patients had positive responses with HV + TM. Thus, the specificity of the newly combined HV + TM test was 100%.
Table 3--Incidence of Ischemic Changes and Chest Symptoms During HV + TM(*)
(*) Values given as No. (%) or No.
([dagger]) p < 0.01 vs nonorganic stenosis group.
Dynamic Parameters During Exercise
There were no differences between the two groups concerning heart rate, BP, or rate pressure products (organic stenosis group, 24,122 [+ or -] 6,811; nonorganic stenosis group, 24,446 [+ or -] 6,368; difference not significant). In the organic stenosis group, 6 of 24 patients (25.0%) reached their target heart rate during exercise, while in the nonorganic stenosis group 17 of 50 patients (34.0%) reached their target heart rate during exercise.
Correlations Between Disease Activity and the Incidence of Ischemic Findings
As shown in Table 4, we compared positive responses on ECG by HV + TM and ACh testing and by spasm induced by ACh. Patients with higher disease activity exhibited more ischemic evidence with both procedures. However, there were no differences concerning ischemic evidence in the disease activity between the two procedures. More than half of the patients with low disease activity demonstrated ischemic ECG changes by HV + TM. However, in patients with low disease activity, the incidence of provoked coronary artery spasms was significantly higher than the frequency of positive ECG changes resulting from the newly combined HV + TM test or the ACh test.
Table 4--Comparison of Frequency of Ischemic Findings on ECG in Two Methods According to the Degree of Disease Activity(*)
(*) Values given as No. (%).
([dagger]) p < 0.05 vs others.
Overall Results
The overall results are shown in Table 5. There are no differences between the ACh test and HV + TM test concerning ischemic ECG changes or chest pain. However, in patients with nonorganic stenosis, the occurrence of chest pain as a result of ACh testing was significantly higher than that of the newly combined HV + TM test. Coronary spasms were induced by the intracoronary injection of ACh in 61 patients (82.4%). The remaining 13 patients showed coronary spasms with the intracoronary administration of ergonovine. Coronary spasm was induced in the right coronary artery in 11 of these patients, and the remaining 2 patients had coronary spasms in the left anterior descending artery.
Table 5--Comparisons of Ischemic Evidence Between the Two Procedures(*)
(*) Values given as No. (%). NS = not significant.
Arterial blood pH increased from 7.42 to 7.63, while arterial blood [PO.sub.2] increased from 86 to 119 mm Hg and arterial blood [PCO.sub.2] decreased from 39 to 20 mm Hg. Sufficient alkalosis was obtained by mild hyperventilation.
Complications
No serious irreversible complications were observed during the ACh test or HV + TM test. However, during the HV + TM test, two patients demonstrated serious arrhythmias, one patient demonstrated complete atrioventricular block, and one patient demonstrated nonsustained ventricular tachycardia. After the administration of isosorbide dinitrate, the arrhythmias disappeared quickly. Two patients had four or more anginal attacks per month (ie, high disease activity).
DISCUSSION
In the majority of previous studies,[1,2,4,6,7,19] regarding the effectiveness of the induction of coronary artery spasm in patients with vasospastic angina, all subjects exhibited variant angina. However, in this study, all patients demonstrated coronary spastic angina with nonvariant angina, and no patients had spontaneous ST-segment elevation. Moreover, almost all patients had single-vessel or nonsignificant coronary stenosis, more than half of the patients had sporadic anginal attacks (ie, less than one attack per month), and no patients had more than or equal to two sporadic anginal attacks per day. In these patients with nonvariant angina, we compared the clinical usefulness of two methods, invasive and noninvasive tests. In patients with coronary artery spasm and variant angina, evidence of ischemia can be obtained readily by noninvasive procedures. However, it is difficult to detect evidence of ischemia by noninvasive methods in patients with coronary artery spasm and nonvariant angina.
In variant angina, pharmacologic agents such as ACh or ergonovine are effective in reproducing ST-segment elevation in patients in whom spontaneous ST-segment elevation was demonstrated. However, Bertrand et al[20] reported that methylergonovine induced coronary artery spasm in only 38% of patients who had experienced angina at rest in a French study. We reported[21] also that the frequency of provoked coronary spasm by the intracoronary administration of ACh was 66.9% in patients who experienced angina at rest in a Japanese study. A standard spasm provocation test alone may not always provoke coronary spasm in patients who experience angina at rest. In this study, ACh provoked coronary spasm in 61 of 74 patients (82.4%) with coronary spastic angina. Intracoronary injection of ACh did not provoke coronary spasm in 13 patients with coronary spastic angina whose spasms were induced by the intracoronary administration of ergonovine. Pharmacologic agents have some limitations for the provocation of coronary artery spasms in patients with vasospastic angina because of circadian variation and disease activity.
We recently reported[22] the clinical characteristics of female patients with coronary spastic angina in Japan and compared them with those of male patients. In this study, most patients with coronary spastic angina were men, and, moreover, the incidence of habitual smoking was also high.
Possible Mechanism With the Newly Combined Test
The precise mechanism of the newly combined HV + TM test for the induction of ischemia might be a dual vasoconstrictive phenomenon. One factor was that alkalosis induced by hyperventilation increased the coronary tone,[23] and another factor was that stimulating the [Alpha]-adrenergic tone by accelerated exercise produced coronary spasm.[24] Because a gradual warming-up exercise, such as that given in the standard Bruce and Horsten[18] protocol, may have a potential to produce a walk-through phenomenon in patients with coronary spastic angina, we selected HV + TM rather than the standard Bruce and Horsten protocol.
Comparison With the Previous Reports
According to previous studies,[25-27] noninvasive spasm provocation tests such as vigorous hyperventilation or bicycle exercise produced ischemic ECG change in about 60 to 80% of patients with variant angina. In these studies, all patients exhibited variant angina. However, in our series, no patients demonstrated spontaneous ST-segment elevation before the study. Regardless of low disease activity, the HV + TM test was as effective as an ACh test.
In 1997, Nakao et al[28] reported the usefulness of a hyperventilation test in a large number of patients with coronary spastic angina, the sensitivity of which was 61.7% (127 of 206 patients) and the specificity of which was 100%. However, if patients had low disease activity (ie, less than one or less than five sporadic attacks per week), positive response was very low (29% or 39%). In contrast, 84% of the patients with high disease activity (ie, five or more attacks per week) had positive responses. Compared with these data, even if patients had very low disease activity (ie, [is less than] 0.25 or less than one sporadic attack per week), the positive response to HV + TM in this study was remarkably high (57% or 72%). Furthermore, 93% of the patients who experienced one or more attack per week had positive responses by our method. Disease activity in our series was remarkably lower than that shown in previous reports. Considering these results, the prevalence of ischemic changes detected by our newly combined HV + TM method was superior to that of previously reported noninvasive methods.
The newly combined HV + TM test had some limitations for detecting evidence of ischemia in patients with coronary artery spasm and no significant organic stenosis, while in patients with coronary artery spasm and organic stenosis, HV + TM was as effective as an ACh test.
If patients with higher spasmodicity, such as those with variant angina, had been studied, more frequent and higher positive responses and more serious complications likely would have been found. Therefore, we recommend that HV + TM should be performed in patients with variant angina if a positive response was not produced by the hyperventilation test or the exercise test alone.
Clinical Implications
Our newly combined HV + TM method is as safe and reliable for the induction of ischemic changes in patients who experience angina at rest and in those with coronary artery spasm as is an ACh test. If the HV + TM method is performed to screen for coronary artery spasms, a part of the cardiac catheterization procedures may be avoided in clinical situations. As shown in Figure 1, if ST-segment elevation was revealed by this procedure, patients had a higher potential for developing significant organic stenosis, while if ST-segment depression was observed, patients exhibited higher prevalences of no stenosis or near-normal coronary arteries. Moreover, if patients exhibited no ischemic changes, they may have had low spasmodicity or near-normal coronary arteries. In these patients, cardiac catheterization procedures were not immediately required to evaluate coronary spasm or atherosclerosis. If myocardial injury or myocardial ischemia on ECG or myocardial scintigraphy were observed, coronary angiography was required to demonstrate coronary spasms and to evaluate fixed lesions. We recommend that medications, including the administration of a calcium channel blocker and/or isosorbide dinitrate, should be started without performing coronary angiography in patients with negative results of HV + TM. However, follow-up tests are necessary whether medications are continued or not in those patients.
[Figure 1 ILLUSTRATION OMITTED]
Limitations
This study had three limitations. One involved the medication administered before the spasm provocation test and the newly combined HV + TM test. For 24 h, all medication except for nitroglycerine was stopped. However, long-acting calcium antagonists may have had residual effects. The second limitation was the time in which the cardiac catheterization procedure was performed. The ACh testing was not performed in the early morning. In the afternoon, the tone of the coronary artery was decreased compared to that in the morning.[29] However, HV + TM was performed in the morning. The third limitation was that the newly combined HV + TM test was insensitive in the detection of multiple spasms. In this study, multiple spasms were not diagnosed in any patients by the newly combined HV + TM test, while 59.4% of all patients had multiple spasms as a result of the ACh test.
ACKNOWLEDGMENT: We acknowledge the helpful comments of Yuji Shigematsu, MD, Mareomi Hamada, MD, and Kunio Hiwada, MD.
REFERENCES
[1] Yasue H, Nagao M, Omote S, et al. Coronary arterial spasm and Prinzmetal's variant form of angina induced by hyperventilation and Tris-buffer infusion. Circulation 1978; 58: 56-62
[2] Girotti LA, Crossato JR, Messuti H, et al. The hyperventilation test as a method for developing successful therapy in Prinzmetal's angina. Am J Cardiol 1982; 49:834-841
[3] Raizner AE, Chahine RA, Ishimori T, et al. Provocation of coronary artery spasm by the cold pressor test. Circulation 1980; 62:925-932
[4] Waters DD, Szlachcic J, Bonan R, et al. Comparative sensitivity of exercise, cold pressor and ergonovine testing in provoking attacks of variant angina in patients with active disease. Circulation 1983; 67:310-315
[5] Bobba P, Vecchio C, Di Guglielmo L, et al. Exercise-induced RS-T elevation: electrocardiographic and angiographic observations. Cardiology 1972; 57:162-171
[6] Specchia G, De Servi S, Falcone C, et al. Coronary arterial spasm as a cause of exercise-induced ST-segment elevation in patients with variant angina. Circulation 1979; 59:948-954
[7] Lahiri A, Subramanian B, Millar-Craig M, et al. Exercise-induced S-T segment elevation in variant angina. Am J Cardiol 1980; 45:887-894
[8] Castello R, Alegria E, Merino A, et al. The value of exercise testing in patients with coronary artery spasm. Am Heart J 1990; 119:259-263
[9] Yasue H, Horio Y, Nakamura N, et al. Induction of coronary artery spasm by acetylcholine in patients with variant angina: possible role of the parasympathetic nervous system in the pathogenesis of coronary artery spasm. Circulation 1986; 74:955-963
[10] Heupler FA. Provocative testing for coronary arterial spasm: risk, method and rationale. Am J Cardiol 1980; 46:335-337
[11] Hackett D, Larkin S, Chierchia S, et al. Induction of coronary artery spasm by a direct local action of ergonovine. Circulation 1987; 75:577-582
[12] Curry RC, Pepine CJ, Sabom MB, et al. Similarities of ergonovine-induced and spontaneous attacks of variant angina. Circulation 1979; 59:307-312
[13] Sueda S, Kawada H, Matsuda S, et al. New protocol for detection of vasospastic angina with almost normal coronary arteries [abstract]. Circulation 1995; 92:I-211
[14] Sueda S, Mineoi K, Ochi T. New non-invasive protocol for detection of vasospastic angina with significant organic stenosis [abstract]. J Am Coll Cardiol 1997; 29:165A
[15] Sueda S, Saeki H, Otani T, et al. Investigation of the most effective provocation test for patients with coronary spastic angina: usefulness of accelerated exercise following hyperventilation. Jpn Circ J 1999; 63:85-90
[16] Sueda S, Saeki H, Otani T, et al. Major complications during spasm provocation tests with an intracoronary injection of acetylcholine. Am J Cardiol 2000; 85:391-394
[17] Austen WG, Edwards JE, Frye RL, et al. A reporting system on patients evaluated for coronary artery disease; report of the Ad Hoc Committee for Grading of Coronary Artery Disease, Council on Cardiovascular Surgery, American Heart Association. Circulation 1975; 51:5-40
[18] Bruce RA, Horsten TR. Exercise stress testing in the evaluation of patients with ischemic heart disease. Prog Cardiovasc Dis 1969; 11:371-390
[19] Waters DD, Chaitman BR, Dupras G, et al. Coronary artery spasm during exercise in patients with variant angina. Circulation 1979; 3:580-585
[20] Bertrand ME, LaBlanche JM, Tilmant PY, et al. Frequency of provoked coronary arterial spasm in 1089 consecutive patients undergoing coronary arteriography. Circulation 1982; 65:1299-1306
[21] Sueda S, Ochi N, Kawada H, et al. Frequency of provoked coronary vasospasm in patients undergoing coronary arteriography with spasm provocation test of acetylcholine. Am J Cardiol 1999; 83:1186-1190
[22] Sueda S, Suzuki J, Watanabe K, et al. Clinical characteristics of female patients with coronary spastic angina: comparison with male patients. Jpn Circ J 2000; 64:416-420
[23] Fleckenstein A, Nakayama K, Fleckenstein-Grun G, et al. Interactions of hydrogen ions, calcium antagonist drugs and cardiac glycosides with excitation-contraction coupling of vascular smooth muscle. In: Betz E, ed. Ionic action on vascular smooth muscle. New York, NY: Springer-Verlag, 1976; 117-125
[24] Ysue H, Omote S, Takizawa A, et al. Exertional angina pectoris caused by coronary arterial spasm: effects of various drugs. Am J Cardiol 1979; 43:647-652
[25] Fujii H, Yasue H, Okumura K, et al. Hyperventilation-induced simultaneous multivessel coronary spasm in patients with variant angina: an echocardiographic and arteriographic study. J Am Coll Cardiol 1988; 12:1184-1192
[26] DeServi S, Falcone C, Gavazzi A, et al. The exercise test in variant angina: results in 114 patients. Circulation 1981; 64:684-688
[27] Crea F, Davies G, Chierchia S, et al. Different susceptibility to myocardial ischemia provoked by hyperventilation and cold pressor test in exertional and variant angina pectoris. Am J Cardiol 1985; 56:18-22
[28] Nakao K, Ohgushi M, Yoshimura M, et al. Hyperventilation as a specific test for diagnosis of coronary artery spasm. Am J Cardiol 1997; 80:545-549
[29] Yasue H, Omote S, Takizawa A, et al. Circadian variation of exercise capacity in patients with Prinzmetal's variant angina: role of exercise-induced coronary arterial spasm. Circulation 1979; 59:938-948
(*) From the Department of Cardiology (Drs. Sueda, Fukuda, and Watanabe), Saiseikai Saijo Hospital Saijo City, Japan; and the Department of Cardiology (Drs. Ochi, Kawada, Hayashi, and Uraoka), Kita Medical Association Hospital, Ozu, Japan. Manuscript received March 28, 2000; revision accepted July 17, 2000.
Correspondence to: Shozo Sueda, MD, Department of Cardiology, Saiseikai Saijo Hospital, Tsuitachi 269-1, Saijo City, Ehime Prefecture 793-0027, Japan
COPYRIGHT 2001 American College of Chest Physicians
COPYRIGHT 2001 Gale Group