Abstract
Acne rosacea is a multifactorial, somewhat mercurial disorder that can be a challenge to control with standard pharmacologic agents. Laser and light sources have been increasingly utilized, particularly for control of the generalized erythema, flushing, and telangiectasia of rosacea. This paper will review the clinical studies presented in the literature specifically treating patients with rosacea. Long-pulsed dye lasers and intense pulsed light devices can offer patients effective treatment without the purpura of short-pulsed dye lasers. Long-term efficacy has not been studied but maintenance therapy may be necessary to control the vascular manifestations of this disease.
Introduction
The typical age of onset of rosacea is 30 to 50 years old and it occurs more often in those of northern and western European descent with a fair complexion. In a Swedish survey, it was estimated that females are affected more than males by a 3:1 ratio. (1)
Rosacea is a complicated inflammatory disease of the skin characterized by both vascular and acneform components with the cheeks and nose most commonly involved. It may also commonly involve the chin and forehead, and less often nonfacial regions such as the neck, ears, and scalp. Clinical manifestations may include transient erythema, persistent centrofacial erythema, telangiectasia, papules, and pustules. In severe cases, granulomatous changes and lymphedema may lead to the development of rhinophyma. Other secondary symptoms are burning and stinging, ocular manifestations (blepharitis and conjunctivitis), plaques, and a dry appearance. Four subtypes of rosacea have been recently introduced by the National Rosacea Society: erythema-totelangiectatic, papulopustular, phymatous, and ocular (2) (Table 1). Patients may exhibit features of more than one subtype simultaneously.
The etiology of rosacea is not fully understood. There appears to be a genetic tendency but other factors have been implicated in the mechanisms of this disease. Some suggested causative agents include Helicobacter pylori bacterium (3,4) and Demodex folliculorum, (5) but true causal relationships have not been clearly identified with these or any other infectious agent. In those with erythemotelangiectatic rosacea, the disease is exacerbated by exposure to caffeine, alcohol, spicy foods, emotional stress, exercise, and extreme temperatures. Wilkin et al demonstrated that rosacea patients blush longer and faster after drinking warm liquids than people who do not have rosacea. (2) The mechanism of this apparent vascular hyper-responsiveness is unknown. In addition to vascular dysfunction, disturbances in inflammatory and immunomodulatory processes have also been recognized in this disease. Histopathologic studies suggest inflammation of the pilosebaceous follicle may play a central role in the pathogenesis of rosacea. Powell and colleagues noted 31 of 33 biopsies of patients with papules and pustules showed evidence of folliculitis. (6)
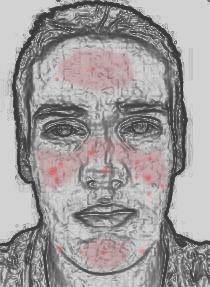
Given the diversity in subtypes, symptoms, and in potential abnormal pathways in rosacea, it is not surprising that there is no uniform paradigm in treating this disease. Numerous medical treatments are available and must be tailored to subtype and symptoms. This paper will focus on laser and light therapies available for the first 2 subtypes of rosacea. Vascular lasers and light therapies are most effective for the erythematotelangiectatic subtype of rosacea (Figure 1).
Pulsed Dye Lasers
Laser therapy for acne rosacea has been utilized for the reduction of the telangiectasia and erythema seen in rosacea. Both short- and long-pulsed dye laser therapy with wavelengths of 585 or 595 nm have been examined for rosacea patients. These wavelengths correspond closely to the absorption peak of oxyhemoglobin (577 nm), and target superficial small vessels. Pulse durations from 450-[micro]s to 6 msec have been utilized in published rosacea studies (Table 2).
Lowe et al was the first to report the specific use of a vascular laser, the 585-nm pulsed dye laser, for treatment of rosacea in 1991. (7) Twenty-seven patients with a history of rosacea, refractory to either oral antibiotics or metronidazole gel, were treated with a 585 flash lamp pumped dye laser (Candela Corp SPTL--1) at 450-msec pulsed width and a 5 mm spot size. Within 1 to 3 treatment sessions, almost all treated areas improved to an excellent (10) or good degree (14) utilizing fluences of 6.0 to 7.5 J/[cm.sup.2]. In another prospective study by Clark et al utilizing the 450-msec pulsed dye laser (Candela Corp SPTL--1b, Wayland, MA) in 12 patients, a split-face controlled study demonstrated similar results with 50% reduction in erythema, 55% reduction in flushing, and 75% reduction in telangiectasia after an average of 3 treatments with fluences of 5.5 to 7.5 J/[cm.sup.2]. (8) A trend toward reduction in inflammatory lesions was also noted in this study. Purpura occurred in all patients lasting 7 to 10 days, post inflammatory hyperpigmentation occurred in half of the patients, and 2 patients had small macular atrophic scars. These findings were similar to Tan's study that used similar laser parameters with lower fluences. (9) Tan had fewer patients with post inflammatory hyperpigmentation (6/40) and no incidence of scarring. Lonne-Rahm conducted a study of 32 patients with rosacea, all with positive results from a lactic acid "stinger" test. (10) Three months after a single treatment with a 585-nm, 450-[micro]sec PDL utilizing fluences of 6.0 to 6.75J/[cm.sup.2], 24 of 32 patients had a negative stinger test and all but one had a decreased stinger test score. The authors concluded that laser treatment of rosacea has a clear medical benefit in the reduction in unpleasant symptoms of sensitive skin. A fifth study with the 585-nm short-pulsed dye laser (Candela Corp, SPTL--1, Wayland, MA), however, contradicted other studies, concluding that this laser was of limited value in the treatment of rosacea utilizing similar parameters of 450 msec and a mean fluence of 6.5J/[cm.sup.2] in 10 patients. (11)
[FIGURE 1 OMITTED]
Two subsequent studies have examined newer long-pulsed dye lasers for the vascular manifestations of rosacea, which have the potential to treat vascular ectasias without the purpura of the short-pulsed dye lasers. Newer generation lasers also incorporate cooling devices to cool the epidermis before, during, or after the laser pulse therapy enabling higher fluences while protecting the epidermis. Tan treated 16 patients with a 595-nm PDL (V beam, Candela Corp, Wayland, MA) with a 7-mm sport size, a 1.5-msec pulse duration, and fluences ranging from 9.5 to 11.5 J/[cm.sup.2] depending on tissue response for 2 monthly treatment sessions. (12) All patients experienced a significant improvement in their quality of life and a reduction in their degree of flushing and other symptoms. Despite this success, all patients experienced immediate, deliberate purpura as part of the chosen study design because gentler, subpurpuric thresholds had been shown to be less effective in earlier studies. Complications included transient hyperpigmentation (31.2%) and crusting (25%) and, as described earlier, postoperative purpura. Due to the high complication rate and prolonged down time, this treatment may not be the treatment of choice for the majority of patients, despite its efficacy. A second study with a long-pulsed dye laser by Jasmin utilized a 595-nm PDL (V Beam, Candela Corp) with subpurpuric pulse widths of 6 msec, a 7-mm spot size, and titrated fluences from 7 to 9 J/[cm.sup.2]. (13) Immediate purpura lasting only a few seconds was the treatment endpoint. Pretreatment cooling was achieved by cryogen spray for 30 msec. After one treatment, 2 of 12 patients had 75% improvement, 2 had 50% to 75% improvement, and 5 hand 25% to 50% improvement. There was no lasting post treatment purpura, and there were no complications.
Although subpurpuric PDL therapy with pulse durations of 6 msec or greater, will generally require more than one treatment (2 to 6) to substantially reduce the vascular manifestations of rosacea, in our experience, most patients will choose this option rather than undergo purpura, downtime, and increased risk of complications. When the primary target is the facial erythema of rosacea, larger spot sizes (10 mm) should be chosen to avoid reticulation. (7,14) Two to three laser passes may be required for optimal efficacy. For facial telangiectasia, effective treatment with a long-pulsed dye laser may require stacking of 3 to 4 laser pulses. (15) The endpoint should be vessel blanching or transient thrombosis. When stacking laser pulses, the laser surgeon may want to use lower fluences being careful not to damage or destroy tissue. If a plateau in response is noted with long-pulsed dye lasers, the 0.5-msec pulsed dye laser may then be utilized with expected purpuric sequelae. The smaller 40- to 60-mm vessels involved in flushing are expected to be more susceptible to this pulse width. (16) For these stubborn cases, or if patients have time for only one treatment, short-pulsed dye lasers are generally quite effective.
Other vascular lasers are available for treating telangiectasias of the face, but there are very few studies specifically examining their use in rosacea. In addition to PDLs, small superficial vessels can be treated with potassium titanyl-phosphate lasers (KTP) and diode-pumped frequency-doubled lasers (532 nm). In a study by Silver, 47 rosacea patients were treated with the KTP laser. (17) In nearly 40% of patients, one treatment reduced facial telangiectasia by 70% or more. Deeper and larger blue facial vessels require longer wavelength lasers such as the 810 diode laser, the long-pulsed Alexandrite, and the long-pulsed 1064-nm neodymium: yttrium-aluminum-garnet laser. (18)
Intense Pulsed Light (IPL) Therapy
IPL therapy has been shown in many studies to be efficacious in treatment of the manifestations of photoaging such as erythema, telangiectasias, dyschromia, and sallow complexion. Complications are rare and there is generally no downtime. IPL devices deliver a broad spectrum of wavelengths (515 to 1200 nm), which can be altered by cut-off filters to adjust to the patient's skin type and lesion depth. The variable pulse duration of IPL devices (0.5 to 100 msec) also allows for targeting of different sized vessels at different depths. The large spot size of most IPL devices also facilitates treatment of the entire face quickly, a benefit in treating the erythema and flushing of rosacea. (16)
Three recent studies have examined the use of IPL in rosacea. Angermeier studied 188 patients (74 with rosacea), over a 2-year period, treated with IPL (PhotoDerm[R]VL). (14) After an average of 2 treatments, facial clearing of 75% to 100% was noted in the majority (93%) of patients. Adverse events were seen in 18% of patients and included purpura, persistent edema, and transient hypopigmentation. Taub treated 32 patients with rosacea with a series of IPL treatments (Vasculight Plus, Lumenis Inc, Santa Clara, CA). (19) The average number of treatments was 3.6 spaced a minimum of 3 weeks apart utilizing parameters of 2.4/4.0 msec double pulse with a 20-msec delay time and fluences ranging from 32 to 36 J/[cm.sup.2] with a 570 filter or 27 to 32 J/[cm.sup.2] with a 560 filter. Twenty-eight patients (26 males, 2 females) completed the study and evaluated their response to treatment with questionnaires. Of these, redness was better or much better in 83%, flushing and skin texture was better or much better in 75%, and acneform outbreaks were better or much better in 64% of the patients. In a smaller study of 4 female patients with rosacea-associated erythema, Mark looked objectively and quantitatively at blood flow with a scanning laser Doppler before and 1 month after IPL treatments. (20) The IPL (Photoderm VL, Lumenis, Needham, MA) treatments entailed a series of 5 sessions at 3-week intervals utilizing a 515-nm filter, a single pulse duration of 3 msec, and fluences between 22 and 25 J/[cm.sup.2]. A 30% decrease in blood flow was demonstrated along with a 29% decrease in actual area of the cheek occupied by telangiectasia. A decrease in the intensity of erythema of 21% was also noted. No significant complications were reported in either study. Some clinicians have recommended treating rosacea patients with IPL after inducing flushing and/or performing second and third passes with the Nd:YAG laser and 350-msec pulsed dye laser. (21) However, there are no published clinical studies documenting the benefit of these suggestions.
Photodynamic therapy (PDT) with IPL, preceded by application of topical aminolevulinic acid (Levulan[R] Kerastick[R]) for 15 to 60 minutes, is currently approved for treatment of actinic keratoses. Its use in rosacea is being evaluated and early experience appears promising. (22) This treatment can be particularly helpful in the rosacea patient with concomitant photodamage (Figure 2). Future clinical studies of PDT for rosacea are needed to determine optimal parameters and the degree and duration of benefit.
Summary
There are many laser and light devices which have demonstrated efficacy in reducing some of the vascular manifestations of rosacea. The non-purpuric pulsed dye lasers increase compliance and reduce complications, but multiple treatment sessions may be necessary. Pulse stacking or repeat passes may increase efficacy without adverse effect. IPL sources are also patient friendly and offer added benefit to those patients with solar damage. The advent of photodynamic therapy holds promise in improved control of rosacea, but is as yet unproven. A combination of laser and light source therapy may optimize results in patients with both telangiectasia and generalized flushing. (18,23)
[FIGURE 2 OMITTED]
Further long-term clinical studies are necessary to determine the optimal parameters and the benefit of laser and light sources for rosacea. Because the disease is chronic and intermittent, patients should not expect a complete remission after a series of laser or light treatments. Indeed, patients should be informed that laser and light therapies, while effective for rosacea, do not offer a cure. The need for an initial series of treatments followed by a maintenance program of topical agents and periodic laser or light treatments should be emphasized to all patients. A maintenance program for generalized erythema could involve a laser or light treatment every 4 to 6 months. If patients are forewarned to expect maintenance therapy, they will not be disappointed, but rather grateful for the opportunity to control an embarrassing disease.
References
1. Berg M, Liden S. An epidemiological study of rosacea. Acta Derm Venereol (Stockh). 1989;69:419-23.
2. Wilkin J, Dahl M, Detmar M, et al. Standard classification of rosacea: report of the National Rosacea Society Expert Committee on the Classification and Staging of Rosacea J Eur Acad Dermatol Venerol. 2001;15(5):441-4.
3. Diaz C, O'Callaghan CJ, Khan A, et al. Rosacea: a cutaneous marker of helicobacter pylori infection? Results of a pilot study. Acta Derm Venereol. 2003;83(4):282-6.
4. Bamford JT, Tilden RL, Blankush JL. Effect of treatment of helicobacter pylori infection on rosacea. Arch Dermatol. 1999;135(6):659-63.
5. Georgala S, Katolouis AC, Kylafis GD et al. Increased density of demodex and bacteria folliculorum and evidence of delayed hypersensitivity reaction in subjects with papulopustular rosacea. J Eur Acad Dermatol Venereol. 2001;15(5):441-4.
6. Powell FC. Rosacea and the pilosebaceous follicle. Cutis. 2004;74:9-12, 32-34.
7. Lowe NJ, Behr KL, Fitzpatrick R, Goldman M, Ruiz-Esparza J. Flash lamp pumped dye laser for rosacea-associated telangiectasia and erythema. J Dermatol Surg Oncol. 1991;17:522-525.
8. Clark SM, Lanigan SW, Marks R. Laser Treatment of etythema and telangiectasia associated with Rosacea. Lasers Med Sci. 2002;17:26-33.
9. Tan ST, Bialostocki A, Armstrong JR. Pulsed dye laser therapy for rosacea. The British Association of Plastic Surgeons. 2004;57:303-310.
10. Lonne-Rahm S, Nordlind K, Edstrom DW, Ros AM, Berg M. Laser treatment of rosacea. A pathoetiological study. Arch Dermatol. 2004;140:1345-1349.
11. Berg M, Edstrom DW. Flash lamp pulsed dye laser (FPDL) did not cure papulopustular rosacea. Lasers Surg Med. 2004;34:266-268.
12. Tan SR, Tope WD. Pulsed dye laser treatment of rosacea improves erythema, symptomatology, and quality of life. J Am Acad Dermatol. 2004;51:592-599.
13. Jasim ZF, Woo WK, Handley JM. Long-pulsed (6-ms) pulsed dye laser treatment of rosacea-associated telangiectasia using subpurpuric clinical threshold. Dermatol Surg. 2004;30:37-40.
14. Angermeier MC. Treatment of facial vascular lesions with intense pulsed light. J Cutan Laser Ther. 1999;1:95-100.
15. Yengar V, Chatrath V, Rohrer TE. Does pulse stacking improve results for treatment with variable pulsed dye lasers? Laser Surg Med. 2003;(suppl 15):80.
16. Bikowski J, Goldman M. Rosacea: where are WE now? J Drugs Dermatol. 2004;3(3):251-261.
17. Silver BE, Liveshots YL. Preliminary experience with the KTP/532 nm laser in the treatment of facial telangiectasia. Cosmetic Dermatol. 1996;25:229-36.
18. Pelle MT, Crawford GH, James WD. Rosacea: II. Therapy. J Am Acad Dermatol. 2004;51:499-512.
19. Taub AF. Treatment of rosacea with intense pulsed light. J Drugs Dermatol. 2003;3:254-259.
20. Mark KA, Sparacio M, Voigt A, et al. Objective and quantitative improvement of rosacea-associated erythema after intense pulsed light treatment. Dermatol Surg. 2003;29:600-604.
21. Nase G. Latest advances: triple-pass rosacea laser tx. Dermatology Times. 2005; March: 66-67.
22. Katz BE. PDT safely combats acne, rosacea. Dermatol Times. 2005; March: 62.
23. Krivda M. Getting the red out. Skin and Aging. 2003; August: 73-80.
Address for Correspondence
Kimberly J. Butterwick MD
Dermatology/Cosmetic Laser
Associates of La Jolla
7630 Fay Avenue
La Jolla, CA 92037
Phone: 858-459-7011
Fax: 858-459-7017
Kimberly J. Butterwick MD, (a) Lorren S. Butterwick, (a) Amy Han MD (b)
a. La Jolla Spa MD, La Jolla, CA
b. Department of Dermatology, Case Western Reserve School of Medicine/University Hospitals of Cleveland, Cleveland, OH
COPYRIGHT 2006 Journal of Drugs in Dermatology, Inc.
COPYRIGHT 2006 Gale Group