Hepatitis B virus (HBV) is a common cause of liver disease throughout the world. An estimated one third of the world's population has serologic evidence of past infection, and the virus causes more than 1 million deaths annually. (1) In the United States, the incidence of HBV infection declined from about 14 cases per 100,000 population in the mid-1980s to about three cases per 100,000 population in 1998. (2) However, there are still 1.25 million adults and children in the United States with chronic HBV infection.
HBV is transmitted through blood and other body fluids, including semen and saliva. The virus is 100 times more infectious than human immunodeficiency virus (HIV) and, unlike HIV, it can live outside the body in dried blood for longer than a week. (3) In Southeast Asia, China, and sub-Saharan Africa, HBV infection usually is acquired perinatally or in early childhood, leading to a high prevalence of chronic infection (5 to 20 percent). In contrast, 80 percent of infections in the United States, Canada, and Western Europe occur in adults via sexual contact or intravenous drug use, leading to a much lower baseline prevalence (0.1 percent). In the United States, groups at increased risk for HBV infection have been identified (Table 1). (4)
Because newborns have an immature immune system, 90 percent of infants infected perinatally progress to chronic infection. Progression to chronic HBV infection occurs in 25 to 30 percent of persons infected before five years of age, and in 3 to 5 percent of those infected later in childhood or as adults. Immunosuppressed patients are at greater risk of becoming chronically infected. (1,5,6)
Virologic Characteristics
HBV belongs to the Hepadnaviridae family of viruses. Its genome consists of partially double-stranded circular DNA. The DNA is enclosed in a nucleocapsid, or core antigen, which is surrounded by a spherical envelope (surface antigen). The entire virion is known as the Dane particle. In addition to the core and surface proteins, the HBV genome encodes a DNA polymerase that also acts as a reverse transcriptase.
In the hepatocyte nucleus, the viral genome is converted into covalently closed circular DNA (cccDNA). This cccDNA is the template for messenger RNA (mRNA). The mRNA transcribes viral proteins as well as "pre-genomic" RNA that is reverse transcribed into the HBV DNA of new virions. Without the reverse transcriptase, new virions cannot be produced, and replication ceases. The core gene also produces a circulating peptide, the "e" antigen, that is associated with high levels of viral replication. These antigens, as well as corresponding antibodies produced by the immune system, serve as useful laboratory markers of past, current, or chronic infection (Tables 2 (5) and 3 (7)).
Acute Infection
Acute HBV infection is subclinical in 70 percent of adults and 90 percent of children younger than five years. The incubation period after infection lasts one to four months. Symptoms of acute HBV infection include nausea, anorexia, fatigue, low-grade fever, and right upper quadrant or epigastric pain. Clinical jaundice appears as constitutional symptoms are resolving. Extrahepatic manifestations of acute HBV infection include myalgias, joint pain, and urticaria. Symptoms of acute disease resolve by one to three months, although some persons have prolonged fatigue. Treatment for acute infection is generally supportive, although some patients require hospitalization.
Hepatic transaminase levels (alanine transaminase [ALT] and aspartate transaminase [AST]) reflect hepatocellular injury and range from several hundred to 20,000 IU per L. These values tend to rise one to two weeks before the onset of jaundice. Serum bilirubin values are usually less than 20 mg per dL (342 [micro]mol per L). Mild anemia is common, as is relative lymphocytosis. More severe disease results in an elevation in the prothrombin time and a decrease in the serum albumin level. HBV is not cytopathic, and liver injury is caused by the host's immune response against infected hepatocytes.
Acute HBV infection leads to fulminant hepatic failure from massive hepatocellular necrosis in about 1 percent of infections. Rarely, patients with an "exuberant" immune response present with clinical symptoms but progress to hepatic decompensation, including encephalopathy and coagulopathy. Mortality is high, and liver transplantation often is necessary. (8)
Chronic Infection
Chronic HBV infection is defined as hepatitis B surface antigen (HBsAg) positivity for at least six months (Table 4). (9) Current thinking endorses the concept of four distinct stages of HBV infection, which may be used to describe acute and chronic disease. (5,9)
The first stage, the "immune tolerant" phase, is characterized by high levels of HBV DNA replication, hepatitis B e antigen (HBeAg) positivity, and normal serum transaminase levels. In the acutely infected child or adult, this stage represents the incubation period before immune response to HBV. In neonates, the immune-tolerant stage may last for years to decades.
The second stage reflects the "immune response," which is the inflammatory process that results in the destruction of HBV-infected cells, elevating transaminase levels. Persistence of the immune response phase beyond six months is considered chronic HBV infection. This stage carries the highest risk of progression to cirrhosis and hepatocellular carcinoma. Chronic HBV infection has been associated with polyarteritis nodosa, a systemic vasculitis, and membranous or membranoproliferative glomerulonephritis. (8)
The third stage, the "inactive carrier" state, is thought to mark the end of active viral replication. HBeAg becomes negative, hepatitis B e antibody (anti-HBe) appears (seroconversion), and transaminase levels normalize. A low level of HBV DNA still may be present. The majority of adults with acute HBV infection enter this stage rapidly. In most chronically infected neonates and some children and adults, the conversion rate is 5 to 15 percent per year; a higher rate is associated with increasing age and elevated ALT levels. (5) From 10 to 30 percent of carriers will have disease flares similar to acute HBV infection. These flares may be caused by other viral infections, or they may be secondary to viral reactivation and an unregulated immune response. The latter situation can occur during interferon therapy for HBV infection or after the withdrawal of corticosteroids or chemotherapy for other diseases. (10)
The fourth, or "immune," stage is characterized by the clearance of HBsAg. HBV DNA is usually undetectable, and reactivation or reinfection is uncommon. Progression from the third to the fourth stage occurs in approximately 3 percent of HBV-infected persons per year. (8)
Natural History and Complications
It has been estimated that 12 percent of patients with chronic HBV infection develop cirrhosis annually, and that a smaller percentage develop hepatocellular carcinoma. (8) The absolute lifetime risk of death from cirrhosis or hepatocellular carcinoma is 15 to 25 percent. (4)
As with acute HBV infection, cirrhosis and hepatocellular carcinoma are not the result of a direct effect of the virus but develop because of an immune-mediated inflammatory response. This response results in the destruction and regeneration of liver cells, eventually leading to chromosomal mutations and unchecked cellular growth.
Screening for Hepatocellular Carcinoma
Screening patients with chronic HBV infection for hepatocellular carcinoma using alpha-fetoprotein measurements or ultrasonography remains controversial. Hepatocellular carcinoma may not develop for 25 to 30 years after chronic infection develops, although it occasionally appears earlier. Men are at greater risk than women.
No randomized trials of patients with chronic HBV infection have been performed to determine if early detection and resection of hepatic tumors has an effect on mortality. Nonetheless, the American Association for the Study of Liver Disease (AASLD) recommends screening for hepatic tumors every six months when chronic HBV infection is present in men older than 45 years, in patients with biopsy-proven cirrhosis, and in patients with a family history of hepatocellular carcinoma. (9) They also note that annual screening for hepatocellular carcinoma in low-risk patients should be considered. (9)
Prevention
HBV vaccine has had an enormous impact. From the late 1980s to 2001, the incidence of acute hepatitis B in the United States decreased from more than 300,000 cases per year to 79,000 cases per year.11 Predictably, the largest decreases have occurred in children and health care workers--the two groups with the highest rates of vaccination. (2)
Vaccination is recommended for all children and adolescents, adults in certain ethnic groups, health care workers, and other high-risk groups (Table 1). (4) [Evidence Level C, consensus/expert guidelines] A three-injection series induces protective antibody levels in 95 percent of children and 90 percent of adults. Those who fail to respond may be re-vaccinated; in this group, 30 to 50 percent will achieve protective levels. (12)
Because HBV vaccine is so effective, the Centers for Disease Control and Prevention recommends initiation of the series even if completion cannot be guaranteed. Booster vaccination is recommended only for immunocompromised persons who do not respond after the initial series. The only contraindication to vaccination is a history of anaphylaxis after a previous dose of the vaccine or a known previous anaphylactic reaction to yeast. (4)
In the United States, screening for HBV infection in the absence of symptoms or liver function abnormalities is indicated only in pregnant women and in the sexual partners or household contacts of known HBsAg-positive patients. Some investigators argue convincingly that the high prevalence of HBV infection observed in sexually transmitted disease (STD) clinics and prisons indicates a need for testing in those populations. Others advocate screening immigrants from areas where HBV-infection is endemic. (2,12)
Hepatitis B and Pregnancy
Testing for HBsAg is recommended for all pregnant women at the first prenatal visit. A positive result mandates the administration of HBV immune globulin and HBV vaccine to the infant within 12 hours of birth. These interventions reduce the risk of perinatal transmission of HBV to less than 3 percent. (13) In the absence of prophylaxis, the risk of perinatal transmission is 10 percent if the mother is positive for HBsAg alone but 90 percent if the mother is HBeAg positive. (14)
Women who are HBsAg negative may be vaccinated safely during pregnancy. No current evidence supports the use of cesarean delivery to reduce vertical transmission of HBV. Recent data suggest that breastfeeding by mothers with chronic HBV infection does not appear to increase the risk of viral transmission to their infants. (15)
Treatments for Chronic HBV Infection
Family physicians should become familiar with the evaluation of patients with newly diagnosed HBV infection, including the recommended laboratory work-up (Table 5). (9) The decision to treat chronic HBV generally is based on a combination of clinical, laboratory, and histologic factors (Table 6). (9,16)
Treatments are not curative because they rarely produce permanent remission of the disease. Therefore, the goals of therapy are long-term suppression of viral replication and prevention of end-stage liver disease. (16) Markers of successful therapy include HBeAg seroconversion, decreased or undetectable levels of HBV DNA, and lack of disease progression.
Approved drugs and agents in development for the treatment of chronic HBV infection fall into two categories: immune modulators, namely recombinant interferon alfa-2b (Intron A); and direct inhibitors of HBV replication, including lamivudine (Epivir) and adefovir dipivoxil (Hepsera). Dosing information is provided in Table 7. (9,16,17) An AASLD treatment protocol recommends testing for HBsAg, HBeAg, and HBV DNA at baseline, at the end of treatment, and six months afterward. (9)
INTERFERON ALFA-2B
Approved in the United States as therapy for chronic HBV infection in 1992, interferon alfa-2b is thought to work by affecting viral replication and, as an immunomodulator, by up-regulating cytokines involved in the response to infection. Predictors of successful therapy include low HBV DNA levels, elevated transaminase levels, lack of fibrosis on liver biopsy, female sex, and absence of HIV coinfection. (16) Contraindications to interferon alfa-2b therapy include preexisting neutropenia, thrombocytopenia, severe uncontrolled depression, decompensated cirrhosis, and current alcohol or drug abuse. Because interferon alfa-2b has numerous side effects, tolerance is a problem in many patients.
Overall, 46 percent of patients treated with interferon alfa-2b have HBeAg seroconversion in the first year after treatment. (8) Hepatitis B surface antibody (anti-HBs) develops in 8 percent of treated patients. Follow-up studies (five to 10 years) in North America and Europe have demonstrated 80 to 95 percent persistence of HBeAg negativity. (6) Response rates and durability of response are significantly lower in neonates and Asians. To date, long-term follow-up has demonstrated two different patterns of benefit from interferon alfa-2b therapy in patients with chronic hepatitis B: (1) reduction in mortality from hepatocellular carcinoma in Asian patients, and (2) decreased mortality from decompensated cirrhosis in North American and European patients. (6)
LAMIVUDINE
A nucleoside analog, lamivudine was first used to treat HIV infection and was approved for the treatment of HBV infection in 1999. This agent competitively inhibits reverse transcriptase, thereby terminating proviral DNA chain extension. A 1998 Chinese double-blind trial (18) showing substantial histologic improvement after one year of treatment in adult patients was soon followed by a U.S. study (19) demonstrating decreased HBV DNA levels, diminished transaminase levels, and loss of HBeAg in adult patients with chronic hepatitis B. A more recent study (20) showed that lamivudine also is effective in children with chronic HBV infection.
The advantages of lamivudine over interferon alfa-2b include oral administration, high degree of tolerability, and safety in patients with decompensated cirrhosis. Lamivudine can be used as first-line therapy or following interferon failure. Disadvantages include uncertainty about the duration of therapy and the long-term durability of response. In addition, lamivudine-resistant strains of HBV develop at a rate of 15 to 20 percent per year of therapy. Despite the persistence of HBeAg, resistant virus appears to be less infective than wild-type virus, and continuing lamivudine therapy still results in improvement of laboratory and histologic markers of HBV infection. (21)
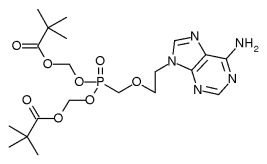
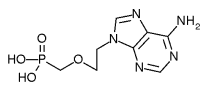
ADEFOVIR DIPIVOXIL
As early as 2000, adefovir dipivoxil was noted to be effective in suppressing HBV strains that had developed resistance to lamivudine. (22) In September 2002, this nucleotide analog was approved for the treatment of HBV infection. (23)
Two recent clinical trials of adefovir dipivoxil in HBeAg-negative and HBeAg-positive patients demonstrated significant improvements in histologic, virologic, and biochemical markers after 48 weeks of treatment; no adefovir dipivoxil-resistant HBV strains were noted, and the drug's safety profile was similar to that for placebo. (24,25) [References 24 and 25--Evidence level A, randomized controlled trials] Dosing adjustment is recommended for patients with renal insufficiency.
Where adefovir dipivoxil fits into the treatment of HBV infection--as first-line monotherapy, combination therapy, or salvage therapy for lamivudine-resistant infection--remains to be determined. Because of its tolerability and oral route of administration, it is likely that this agent will supplant interferon alfa-2b as first-line therapy in most patients.
Future Prospects
The decline in the rate of new HBV infections in the United States over the past two decades is encouraging, and new oral agents for treatment are in clinical trials. However, problems must be resolved before hepatitis B can be eradicated. One obstacle is the unsubstantiated fear of neurologic side effects of HBV vaccines. A recent large case-control study (26) failed to demonstrate a connection between the recombinant vaccine and an increased risk of multiple sclerosis, which had been suggested by earlier case reports. Another obstacle is the current failure to offer hepatitis vaccination in STD clinics and correctional facilities, as well as to other high-risk groups. (12)
TABLE 1
Groups at Increased Risk for HBV Infection
Persons with a history of sexually transmitted disease
Household contacts of HBV-infected persons
Health care workers
Hemodialysis patients
Intravenous drug users
Infants born to HBV-infected mothers
Immigrants and children of immigrants from hyperendemic areas
Men who have sex with men
Persons who have more than one sexual partner in a six-month period
Sexual partners of HBV-infected persons
HBV = hepatitis B virus.
Information from reference 4.
TABLE 7
FDA-Approved Treatments for Chronic HBV Infection
Recombinant interferon alfa-2b (Intron A)
Recommended dosage: adults--5 million IU SC per day, or 10 million IU SC three times per week; children--3 million IU per [m.sup.2] SC three times in the first week, 6 million IU per m2 SC three times per week after that (not recommended for children younger than one year)
Recommended duration of therapy: HBeAg-positive patients--16 weeks; HBeAg-negative patients--one year
Cost for 16 weeks of therapy: $5,600 *
Cautions: Interferon alfa-2b may cause or aggravate fatal or life-threatening neuropsychiatric, autoimmune, ischemic, or infectious disorders. Patients should be monitored closely with periodic clinical and laboratory evaluations.
Lamivudine (Epivir)
Recommended dosage: adults--100 mg orally per day; children--3 mg per kg orally per day (maximum: 100 mg per day)
Recommended duration of therapy: HBeAg-positive patients--one year but may be longer in those with HBeAg seroconversion; HBeAg-negative patients with chronic HBV infection--longer than one year, although duration has not been established
Cost for one month of therapy: $156
Cautions: Lactic acidosis and severe, possibly fatal, hepatomegaly have been reported. If lamivudine is prescribed for patients with unrecognized or untreated HIV infection, rapid emergence of HIV resistance is likely.
Adefovir dipivoxil (Hepsera)
Recommended dosage: adults--10 mg orally per day
Recommended duration of therapy: one year
Cost for one year of therapy: $528
Cautions: Discontinuation of adefovir dipivoxil therapy may result in severe acute exacerbation. Chronic use may result in nephrotoxicity in patients at high risk for underlying renal dysfunction. Lactic acidosis and severe hepatosplenomegaly with steatosis have been reported. Rapid emergence of HIV resistance may occur in patients with unrecognized or untreated HIV infection. This drug is not FDA-approved for use in children.
FDA = U.S. Food and Drug Administration; HBV = hepatitis B virus; SC = subcutaneously; HBeAg = hepatitis B e antigen; HIV = human immunodeficiency virus.
*--Approximate cost provided by the author.
Information from references 9, 16, and 17.
REFERENCES
(1.) Zuckerman JN, Zuckerman AJ. The epidemiology of hepatitis B. Clin Liver Dis 1999;3:179-87.
(2.) Goldstein ST, Alter MJ, Williams IT, Moyer LA, Judson FN, Mottram K, et al. Incidence and risk factors for acute hepatitis B in the United States, 1982-1998: implications for vaccination programs. J Infect Dis 2002;185:713-9.
(3.) Ott MJ, Aruda M. Hepatitis B vaccine. J Pediatr Health Care 1999;13:211-6.
(4.) Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines 2002. MMWR Recomm Rep 2002;51(RR-6):1-78.
(5.) Lee WM. Hepatitis B virus infection. N Engl J Med 1997;337:1733-45.
(6.) Lok AS, Heathcote EJ, Hoofnagle JH. Management of hepatitis B: 2000--summary of a workshop. Gastroenterology 2001;120:1828-53.
(7.) Viral hepatitis B. Accessed September 17, 2003, at: http://www.cdc.gov/ncidod/diseases/hepatitis/b/ Bserology.htm.
(8.) Befeler AS, Di Bisceglie AM. Hepatitis B. Infect Dis Clin North Am 2000;14:617-32.
(9.) Lok AS, McMahon BJ. Chronic hepatitis B. Hepatology 2001;34:1225-41.
(10.) Perrillo RP. Acute flares in chronic hepatitis B: the natural and unnatural history of an immunologically mediated liver disease. Gastroenterology 2001;120:1009-22.
(11.) Hepatitis B vaccination--United States, 1982-2002. MMWR Morb Mortal Wkly Rep 2002;51:549-52,563.
(12.) Kahn J. Preventing hepatitis A and hepatitis B virus infections among men who have sex with men. Clin Infect Dis 2002;35:1382-7.
(13.) Euler GL, Copeland JR, Rangel MC, Williams WW. Antibody response to postexposure prophylaxis in infants born to hepatitis B surface antigen-positive women. Pediatr Infect Dis J 2003;22:123-9.
(14.) Hunt CM, Sharara AI. Liver disease in pregnancy. Am Fam Physician 1999;59:829-36.
(15.) Hill JB, Sheffield JS, Kim MJ, Alexander JM, Sercely B, Wendel GD. Risk of hepatitis B transmission in breast-fed infants of chronic hepatitis B carriers. Obstet Gynecol 2002;99:1049-52.
(16.) Malik AH, Lee WM. Chronic hepatitis B virus infection: treatment strategies for the next millennium. Ann Intern Med 2000;132:723-31.
(17.) Adefovir (Hepsera) for chronic hepatitis B infection. Med Lett Drugs Ther 2002;44:105-6.
(18.) Lai CL, Chien RN, Leung NW, Chang TT, Guan R, Tai DI, et al. A one-year trial of lamivudine for chronic hepatitis B. N Engl J Med 1998;339:61-8.
(19.) Dienstag JL, Schiff ER, Wright TL, Perrillo RP, Hann HW, Goodman Z, et al. Lamivudine as initial treatment for chronic hepatitis B in the United States. N Engl J Med 1999;341:1256-63.
(20.) Jonas MM, Kelley DA, Mizerski J, Badia IB, Areias JA, Schwarz KB, et al. Clinical trial of lamivudine in children with chronic hepatitis B. N Engl J Med 2002;346:1706-13.
(21.) Lau DT, Khokhar MF, Doo E, Ghany MG, Herion D, Park Y, et al. Long-term therapy of chronic hepatitis B with lamivudine. Hepatology 2000;32(4 pt 1):828-34.
(22.) Perrillo R, Schiff E, Yoshida E, Statler A, Hirsch K, Wright T, et al. Adefovir dipivoxil for the treatment of lamivudine-resistant hepatitis B mutants. Hepatology 2000;32:129-34.
(23.) Baker R. Gilead Sciences wins FDA approval for Hepsera (adefovir dipivoxil). Accessed July 11, 2003, at: http://www.hivandhepatitis.com/hep_b/news/092302a.html.
(24.) Hadziyannis SJ, Tassopoulos NC, Heathcote EJ, Chang TT, Kitis G, Rizzetto M, et al. Adefovir dipivoxil for the treatment of hepatitis B e antigen-negative chronic hepatitis B. N Engl J Med 2003; 348:800-7.
(25.) Marcellin P, Chang TT, Lim SG, Tong MJ, Sievert W, Shiffman ML, et al. Adefovir dipivoxil for the treatment of hepatitis B e antigen-positive chronic hepatitis B. N Engl J Med 2003;348:808-16.
(26.) Ascherio A, Zhang SM, Hernan MA, Olek MJ, Coplan PM, Brodovicz K, et al. Hepatitis B vaccination and the risk of multiple sclerosis. N Engl J Med 2001;344:327-32.
Jeffrey T. Kirchner, D.O. receives a supporting grant from the HIV/AIDS Bureau of the Department of Health and Human Services in Washington, D.C.
KENNETH W. LIN, M.D., is a third-year resident in the Department of Family and Community Medicine at Lancaster (Pa.) General Hospital. Dr. Lin received his medical degree from New York University School of Medicine, New York City.
JEFFREY T. KIRCHNER, D.O., is associate director of the Family Practice Residency Program at Lancaster General Hospital, where he is also medical director of the Comprehensive Care Clinic for HIV. Dr. Kirchner received his medical degree from the Philadelphia College of Osteopathic Medicine and completed a family practice residency at Abington (Pa.) Memorial Hospital.
Address correspondence to Jeffrey T. Kirchner, D.O., Department of Family and Community Medicine, Lancaster General Hospital, 555 N. Duke St., Lancaster, PA 17604 (e-mail: jtkirchn@lancastergeneral.org). Reprints are not available from the authors.
COPYRIGHT 2004 American Academy of Family Physicians
COPYRIGHT 2004 Gale Group