IN SPRING, blooming flowers and lush green trees can make you feel lucky to be alive--or hopelessly miserable, if you're one of the nearly 40 million people who will sneeze and sniffle their way through the next few months.
Allergies are year-round nuisances, but spring packs an especially powerful wallop for those susceptible to tree and grass pollens, mold, and dust mites. Since living in a sterile bubble is impractical, it's best to discover what's new--and what's natural--in allergy relief.
watch on the rhinitis
SEASONAL allergic rhinitis affects about 20 percent of American adults and accounts for nearly 17 million office visits a year to health-care providers, according to the American Academy of Allergy, Asthma & Immunology. Symptoms include nasal stuffiness; sneezing; and itching of the nose, roof of the mouth, and ears. Rhinitis sufferers are also prone to allergic conjunctivitis, an inflammation of the eyes that makes them red, itchy, and watery.
In addition, chronic rhinitis may potentially progress to asthma, according to the World Health Organization. "The inflammation that occurs with allergy and asthma is very similar," explains AAAAI spokesman Gailen D. Marshall, M.D., Ph.D., director of the division of clinical immunology and allergy for the University of Mississippi Medical Center in Jackson. If you have allergies, tell your doctor about any new symptoms, such as frequent coughing (especially during exercise or at night), excessive shortness of breath, or wheezing.
Allergic diseases in general have increased substantially in recent years. Researchers have yet to determine what exactly accounts for the rise--"but it's not genetic," says Marshall, because it's happening too quickly. Likely culprits include environmental issues such as indoor and outdoor pollution, excessive use of antibiotics, and a jump in levels of psychological stress.
And to what do all these allergy patients react? Pollens, mostly.
the inside, and outside, scoop
"CLASSICALLY, spring is tree-pollen season," says Marshall. "As trees bloom and pollinate, all this pollen is in the wind." Then there are grass pollens, which become plentiful in the late spring and early summer. Next come weed pollens, at their highest levels in the late summer and early fall. (Pollen seasons occur earlier in warmer climates, later in colder ones.)
Many people with allergic rhinitis are also sensitive to other allergens, such as mold or dust mites found in common house dust. "It's more and more common that if someone has an allergy to one [substance], they acquire allergies to others," Marshall says. "If the only time you have problems is in the spring, it's likely pollen, and you can focus on that. But if you go up in the attic and start to sniffle, there's a good chance you also have mold and/or dust-mite sensitivity."
So on those blustery or attic-visiting days when you're sneezing, blinking, and bemoaning, what's going on inside? In response to an offending allergen, the immune system thinks it's under attack and produces a certain type of antibody, called IgE. ("Think of 'E' for 'evil,'" Marshall tells his patients.)
The IgE antibody arms white blood cells known as mast cells, which are located in your nose, lungs, eyelids, and other areas. "With continuous pollen exposure, the antibody triggers mast cells to release chemical mediators--the histamines and leukotrienes--that cause you to itch, sneeze, drain, and get congested," says Marshall.
home and other remedies
THE EASIEST WAY to sidestep an attack is to avoid the allergen. If pollen is your nemesis, don't go outside when it peaks--usually between 10 a.m. and 4 p.m. If you have to roam on a high-pollen day, take a shower when you return home, as pollen can collect on your skin and hair, and make symptoms worse.
While at home, try to reduce humidity levels, because dust mites and mold spores thrive in a damp environment. "Ideal is less than 50 percent humidity," says Marshall. "The outside mold, you can't control--the inside mold you can."
Once a reaction occurs, the following therapies can offer relief:
Antihistamines that were formerly prescription--only have become available over-the-counter, says Jeffrey S. Goldsmith, M.D., an internist at Santa Monica-UCLA Medical Center and assistant clinical professor of medicine at UCLA David Geffen School of Medicine. These are often the preferred treatment for mild and intermittent symptoms; choose a non-sedating antihistamine, such as Ioratadine (Claritin, Alavert).
Decongestants are effective at unstuffing noses, but oral decongestants should be used with caution, advises Marshall, who cites possible side effects, such as insomnia and increased blood pressure. Topical decongestants--nasal sprays like Afrin--don't have these risks, but after three or four days they can cause "rebound" congestion.
Cromolyn sodium is a mast-cell stabilizer that's sold over-the-counter as a nasal solution; brand names include Nasalcrom and Intal. It's not as immediate-acting as an antihistamine, but still quite useful at preventing cells from secreting histamine, says Goldsmith; administered prior to allergen exposure, nasal cromolyn may reduce the initial allergic reaction. Side effects are uncommon and usually mild.
Saline nasal mists are "very soothing," says Marshall. "Pollens bind to the mast cells inside the nose, and the saline washes those pollens out." Mists can be concocted at home, he notes, but should be made fresh every day: "Use 114 teaspoon of table salt and 114 teaspoon of baking soda (not powder) in 8 ounces of lukewarm water. Squirt this up your nose with a dropper, put it in a spray bottle, or pour a little into your hand and snort it." You can also purchase a neti pot, which is specifically designed for nasal irrigation.
Butterbur (Petasites hybridus) is another natural option. "Based on the research, butterbur looks very promising for allergic rhinitis," says Mark Blumenthal, founder and executive director of the American Botanical Council in Austin, Texas. Petasin, one of the herb's active ingredients, has been demonstrated to inhibit the activity of histamines and leukotrienes, according to a 2004 report in the Annals of Allergy, Asthma & Immunology. Another recent study, performed at the University of Dundee in Scotland and published in Clinical Experimental Allergy, found that 50 milligrams of butterbur twice daily was as effective at reducing rhinitis symptoms as 180 mg daily of the drug fexofenadine (Allegra).
Aller-7, an ayurvedic allergy formula that contains dried lebbek tree bark and dried chebulic myrobalan fruit, might have some potential, says Blumenthal, although research has shown mixed results. A study published in Emerging Drugs found that Aller-7 improved sneezing, running and itching nose and eyes, and headache in patients compared with a placebo. Yet an analysis by the American Botanical Council found no significant results.
Herbs like nettle (Urtica dioica) and elderflower (Sambucus nigra) may offer some respite from allergy season. The Encyclopedia of Herbal Medicine recommends an infusion of 1 teaspoon of each herb to 2 cups of water, taken daily for three months. For excessive nasal congestion, make a steam inhalation of German chamomile (Chamomilla recutita) by infusing 15 grams of the herb or five to 10 drops of essential oil in 3 cups of water, and inhale for 10 minutes. Also, pycnogenol, a supplement made from the bark of a French pine tree (Pinus maritima), may inhibit the release of histamines. Consult a professional herbalist and your doctor if you have asthma or severe allergy symptoms.
Vitamin C supplementation could be useful. "Recent evidence suggests vitamin C may have immune-enhancing effects," says Marshall, who advises boosting your intake at least two weeks before allergy season. About 1,000 mg a clay of vitamin C tends to minimize symptoms of all kinds of allergies, he notes. (For adults, the recommended daily allowance is 75 mg for women and 90 mg for men--and the upper limit is 2,000 mg.)
Homeopathy is based on the principle that small amounts of substances that provoke symptoms can provide relief. Allergic rhinitis has traditionally been treated with allium cepa (for burning nasal discharge), arsenic iodide (constant sneezing), euphrasia (eye problems), or sabadilla (sore throat). Consult a practitioner or use a formula like Boiron's Sabadil, which has allium cepa, euphrasia officinalis, sabadilla, and other ingredients. (For a full explanation of homeopathy, plus more remedies, see page 74.)
Nutrition may affect how you breathe. A diet low in sodium but high in omega-3 fatty acids found in walnuts, flaxseed, and cold-water fish can reduce symptoms of rhinitis, concludes an analysis in the journal Primary Care. And maintaining a healthy level of bacteria in the gut through a diet rich in vegetables and fruits may help the immune system's resistance to allergens, according to a report in Infection and Immunity. When symptoms do hit, eliminating fatty foods, dairy products, sugar, and alcohol will reduce phlegm.
Relaxation is important because stress makes allergy symptoms worse in many people, says Marshall. Meditating, practicing yoga, and listening to pleasant music have been shown to be beneficial.
For updates on allergy management, contact the American Academy of Allergy, Asthma & Immunology (aaaai.org; 800-822-2762) or the Asthma and Allergy Foundation of American (aafa.org; 800-7-ASTHMA). TO determine the National Allergy Bureau's pollen count for your home area or travel destination, visit aaaai.org/nab.
TALK TO YOUR DOC
Some allergy treatments require professional guidance, including these medications and procedures.
Nasal corticosteroids are anti-inflammatory drugs that treat all symptoms of allergic rhinitis. Newer versions, such as Elonase (fluticasone), Nasonex (mometasone), and especially Nasacort (triamcinolone), are faster-acting and better tolerated.
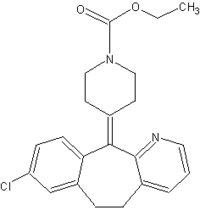
Leukotriene modifiers block the action of substances that lead to inflammation and symptoms like congestion. Depending on the patient, "they're either magic or worthless," says Gailen D. Marshall, M.D. Singulair (montelukast sodium) was first used for the treatment of asthma, but now has the official FDA OK for allergic rhinitis. Other leukotriene modifiers are prescribed "off label" for rhinitis.
Anti-IgE antibody is the latest form of treatment intended to disrupt the allergic chain reaction, sometimes called the allergic cascade. It is expensive, continues to be researched, and is used in moderate to severe cases to reduce asthma symptoms caused by allergies, and only when corticosteroids have proved insufficient.
Immunotherapy isn't new but it can be effective, says Marianne Frieri, M.D., director of allergy immunology training at the Nassau University Medical Center in East Meadow, N.Y. Over time, tiny amounts of an allergen are injected to make the patient less sensitive. "What we call allergy shots work to control allergic rhinitis and can help asthma as well," Frieri notes. "It actually alters the immune-cell response to allergens." in sublingual immunotherapy, or SLIT, the allergens are placed under the tongue. The technique is used in other countries, including England. In a 2004 review in the journal Allergy, researchers concluded that SLIT and the injection technique are almost equivalent.
Acupuncture can relieve allergies, says Michael Spano, L.Ac., a licensed acupuncturist and a clinical resident at Bastyr Center for Natural Health in Seattle. Combining acupuncture with certain Chinese herbal formulas (such as Pe Min Kan Wan) seems to have some benefit, too, he says.
Illustration by HELEN D'SOUZA
COPYRIGHT 2005 Weider Publications
COPYRIGHT 2005 Gale Group