This information is intended far general use only. The clinical implications are specific to the abstracted article only. Individuals intending to put these findings into practice are strongly encouraged to review the original article to determine its applicability to their setting.
Postoperative pain in pediatric ambulatory genitourinary surgery
Ambulatory Surgery
December 2004
Ambulatory pediatric surgery can be successful if postoperative pain is managed well and if the children are able to resume daily activities quickly. Ibuprofen, a nonsteroidal anti-inflammatory drug, reduces hormones that cause inflammation and pain in the body. The purpose of this randomized, prospective, double-blind study was to investigate the effects of preoperative oral ibuprofen on pediatric patients' postoperative pain and resumption of normal activities after ambulatory genitourinary surgery. (1)
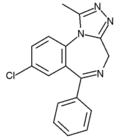
Fifty-four boys ranging in age from younger than one year to 14 years who were scheduled to undergo genitourinary surgery (ie, circumcision, hydrocele, cryptorchidism, hypospadias repair, antegrade sclerotherapy for varicocele) at an outpatient surgery unit of a university hospital in Belgium between November 2000 and February 2001 were entered into the study. The patients were randomly assigned to one of two groups. Patients in both groups received premedication (ie, 0.5 to 1 mg alprazolam for children eight years of age or older, 0.25 to 0.5 mg/kg midazolam for children younger than eight years of age). In addition, patients in the experimental group (n = 28) received 10 mg/kg ibuprofen, while patients in the control group (n = 26) received a placebo liquid. Induction of anesthesia was performed by inhalation of sevoflurane. Within the first two hours after recovery, all patients received 20 mg/kg paracetamol orally, intravenously, or rectally or 10 mg/kg ibuprofen orally.
Pain was measured at the first and second postoperative hours and on the first and second day home. A self-report faces pain scale and the Children's Hospital of Eastern Ontario Pain Scale (ie, CHEOPS behavioral scale) that identifies six groups of behavior patterns (ie, crying, facial expression, verbalizing, movement of the torso, movement of the legs, touching of the wound) in one- to five-year-old children were used. Parents were contacted by telephone on the first and second postoperative day to complete a questionnaire that assessed their child's pain, nausea and vomiting, use of analgesia, and quality of sleep and play for that day. Quality of sleep was assessed using an ordinal scale ranging from very good (ie, zero) to very bad (ie, four). Common statistical procedures, including chi-square and Mann-Whitney U tests, were used to compare the differences between the two groups.
Findings. Twenty-two boys (41%) were four years old or younger, 13 (24%) were five to nine years old, and 19 (35%) were 10 to 14 years old. Overall, there was no significant difference in pain intensity between the two groups; however, there was a significant difference for 10- to 14-year-old boys in the experimental versus the control group in both the parents' (P = .3; z = -2.6) and boys' (P = .024; z = -2.53) assessments. In the postanesthesia care unit, more experimental group patients aged 10 to 14 years received pain medication (P = .04; [X.sup.2] = 3.99) and received pain medication more frequently (P = .03; z = -2.08) than patients in the control group. No significant differences were found regarding nausea and vomiting in the hospital or at home. Additionally, there were no significant differences in sleep quality between the groups. Children in the experimental group had significantly worse quality of play on the first postoperative day than children in the control group (P = .02; z = -2/193).
Clinical implications. This study did not show a difference in postoperative pain, nausea and vomiting, or sleep and play quality up to two days after ambulatory genitourinary surgery that could be attributed to the preoperative administration of oral ibuprofen. The researchers point out that this may be related to the small number of patients included in the study. Perioperative nurses should be prepared to assist in conducting additional studies related to preemptive analgesia.
Effect of smoking on incisionat hernia
Archives of Surgery
February 2005
Smoking has been demonstrated to be a risk factor for wound complications after surgery, including recurrence of groin hernia. Incisional hernias are a late complication of abdominal surgery that occurs in the abdomen in the area of an old surgical scar. Breakdown or loss of fascial closure allows for the protrusion of an organ, such as the bowel or intestines, through the wall that normally contains it. Based on a previous study in which smoking was identified as an independent predictor of inguinal hernia recurrence, it is hypothesized that smoking is associated with incisional hernia after laparotomy. The objective of this cohort study was to identify and assess factors predictive of incisional hernia after laparotomy. (2)
Between January 1997 and December 1998, a total of 1,066 laparotomies and relaparotomies, including open gastroduodenal, biliary, and pancreatic procedures, as well as procedures on the small bowel, colon, and rectum, were performed on 916 patients at a university hospital in Denmark. In October 2001, 33 to 57 months after the surgery, clinical examinations for incisional hernia were conducted, and variables predictive of incisional hernia were assessed. Data on variables related to
* the patients' histories,
* characteristics of the disease,
* the patients' preoperative clinical conditions, and
* operative severity and findings
were collected prospectively and postoperatively and entered into a database. Additional supplemental data, including a detailed smoking history and any information suggesting or indicating that an increase in intra-abdominal pressure could have occurred (eg, hard labor; treatment for chronic obstructive pulmonary disease, constipation, prostate hypertrophy) were included in the database.
An incisional hernia was defined as a palpable defect of the fascia under or adjacent to an incision of the abdominal wall with a protrusion through the defect on Valsalva maneuver. If the clinician's examination disclosed an incisional hernia, data regarding discomfort, pain, and treatment were recorded. Multiple logistic regression technique was used to analyze the data.
Findings. Four hundred ninety-one patients (54%) died before examination, 22 patients (2%) were lost to follow-up, and 93 patients (10%) failed to meet for the follow-up examination; thus, 310 patients were examined. The incidence of incisional hernia was 26% (81 of 310). Multiple regression analysis disclosed that older age, male gender, daily smoking, postoperative wound complication, and relaparotomies were independently associated with incisional hernia. Smokers had a fourfold higher risk of incisional hernia than nonsmokers (odds ratio = 3.93, 95% confidence interval 1.82-8.49).
Clinical implications. The results of this study revealed that smoking is an independent, significant risk factor for incisional hernia. Perioperative nurses should use this information in their efforts to educate patient about the risks of smoking.
Preventing postoperative nausea and vomiting
Canadian Journal of Anesthesia
May 2005
Nausea (ie, the sensation of the urge to vomit) and vomiting or emesis (ie, the involuntary expulsion of gastric contents) are common postoperative complications in patients who have undergone general anesthesia. Administering ondansetron, an antiemetic medication, in combination with another antiemetic that acts through different receptors or with a type 3 serotonin (ie, 5-HT3) receptor antagonist in combination with dexamethasone has been shown to reduce the incidence of postoperative nausea and vomiting (PONV). The objective of this randomized, prospective study was to investigate whether the combination of ondansetron and dexamethasone is superior to ondansetron alone in reducing both the incidence and the intensity of PONV in patients at high risk for this complication. (3)
Patients aged 18 to 70 years who were scheduled to undergo elective procedures under general anesthesia from November 2001 to July 2002 (N = 453) were divided into two study groups (ie, a low-risk group [group L] and a high-risk group [group H]) based on a stratified risk score for PONV that was determined by gender, smoking status, history of PONV and/or motion sickness, and postoperative administration of opioids. The presence of zero, one, two, three, or four of these risk factors correspond to approximately 10%, 20%, 40%, 60%, and 80% risk for PONV.
Patients in group L (n = 87) did not receive any prophylactic antiemetic medications. Patients in the high risk group (n = 366) were randomly assigned to one of two groups. One group (ie, group H-O) received 4 mg ondansetron plus a placebo (n = 185) and the other group (ie, group H-OD) received 4 mg ondansetron plus 8 mg dexamethasone (n = 181). All study medications were given intravenously at the time of induction.
All patients were monitored for the occurrence of emetic symptoms and possible side effects on three occasions within the first 24 hours after their emergence from general anesthesia. Postoperative nausea and vomiting were rated on a numerical scale (ie, 0 = symptoms not present, 1 = mild symptoms, 2 = intermediate symptoms, 3 = strong symptoms). Additionally, any antiemetic medication given during the observation period was recorded. Common statistical techniques, including Student's t test and Fisher exact test, were used to analyze the data.
Findings. The incidence of PONV was 9% in group L, 31% in those receiving ondansetron (ie, H-O group) and 22% in those receiving ondansetron and dexamethasone (ie, H-OD group). The average maximal intensity of the episodes of nausea was significantly greater in the H-O group compared to the H-OD group (0.56 versus 0.33, P = .022). Additionally, the average number of PONV episodes per patient was greater in the H-O group than in the H-OD group (0.69 versus 0.44; P = .034).
Clinical implications. The results of this study confirmed that ondansetron is effective for preventing PONV in high-risk patients and that a combination of ondansetron plus dexamethasone is superior to ondansetron alone in reducing PONV in patients deemed to be at high risk. Perioperative nurses should understand that a validated risk score is an important step within this multimodal approach in the management of PONV.
Preventing PONV with acustimulation
Canadian Journal of Anesthesia
May 2005
Postoperative nausea and vomiting frequently occurs in patients who have undergone middle ear surgery. Several methodologies have been effective in decreasing PONV, including
* medications, such as serotonin antagonists;
* a multimodal approach involving the identification of high risk groups;
* use of an anesthetic technique least likely to cause vomiting;
* administration of a combination of antiemetics; and
* stimulation of the P6 acupoint (ie, an acupuncture point on the wrist) by various methods, including the use of a capsicum plaster.
Capsicum plaster has been used after abdominal hysterectomy, and it appears to be a simple, inexpensive, and easily available method to control PONV; however, its role has not been fully evaluated. The objective of this prospective, randomized, double-blind, and placebo-controlled study was to compare the efficacy of capsicum plaster at the P6 acupoint to ondansetron in preventing PONV in patients undergoing surgery on the middle ear under general anesthesia. (4)
Patients undergoing middle ear surgery at a university-affiliated hospital in northern India (N = 120) were randomly assigned to one of three groups. All patients received 2 mg lorazepam by mouth the night before surgery, and their P6 acupoints were marked on both forearms. Thirty minutes before induction of anesthesia, the capsicum plaster was cut into a 1-cm by 1-cm patch and affixed at the P6 acupoint on both forearms of patients in the acustimulation group (n = 38). Patients in the control group (n = 40) received an inactive adhesive plaster on the same acupoints, and patients in the ondansetron group (n = 39) received the inactive adhesive plaster and 4 mg IV ondansetron. A rescue antiemetic (ie, 4 mg IV ondansetron) was given to patients who experienced persistent PONV. The plaster was removed six hours after surgery, and the incidence of PONV was evaluated within six hours and 24 hours after transfer to the postoperative unit. The Fisher exact test for categorical data and analysis of variance were used to analyze the data.
Findings. Three patients were excluded from the study because they required administration of dexamethasone in the postoperative period--for bronchospasm in two cases and facial nerve injury in one case. In the first six hours after surgery, the incidence of nausea was significantly higher in the control group (ie, 50%) versus the acustimulation (21%) and the ondansetron (28%) groups (P < .05). Approximately 38% of the patients in the control group required rescue antiemetics compared to 24% in the acustimulation group (P > .05) and 18% in the ondansetron group (P < .05).
Clinical implications. This study revealed that stimulation of the P6 acupoint with capsicum plaster is an effective method for preventing PONV after middle ear surgery and is comparable to IV administration of ondansetron for the first six hours after surgery. The cost of capsicum plaster is negligible, and this method appears to be simple, inexpensive, and effective for preventing PONV after middle ear surgery, so perioperative managers and nurses should encourage surgeons to consider its use.
NOTES
(1.) G A Bogaert et al, "Influence of preoperative oral ibuprofen on postoperative pain and normal activities in children after ambulatory genito-urinary surgery," Ambulatory Surgery 11 (December 2004) 27-31.
(2.) L T Sorensen et al, "Smoking is a risk factor for incisional hernia," Archives of Surgery 140 (February 2005) 119-123.
(3.) D Rusch et al, "Prospective application of a simplified risk score to prevent postoperative nausea and vomiting," Canadian Journal of Anesthesia 52 (May 2005) 478-484.
(4.) M N Misra, A J Pullani, Z U Mohamed, "Prevention of PONV by acustimulation with capsicum plaster is comparable to ondansetron after middle ear surgery," Canadian Journal of Anesthesia 52 (May 2005) 485-489.
GEORGE ALLEN
RN, PHD, CNOR, CIC
DIRECTOR OF INFECTION CONTROL
DOWNSTATE MEDICAL CENTER
BROOKLYN, NY
COPYRIGHT 2005 Association of Operating Room Nurses, Inc.
COPYRIGHT 2005 Gale Group