This study evaluated the effectiveness of five human monoclonal antibodies in comparison with human polyclonal antibodies, F(ab')^sub 2^, amantadine, and zanamivir in a mouse model of lethal influenza A virus infection. A single intranasal administration of antibodies was done for immunoprophylaxis. Zanamivir was administered intranasally and amantadine was administered orally. Mice were fully protected by a single dose of 30 mg/kg intravenous Ig administered at least 3 days before challenge. This treatment was equivalent to zanamivir. F(ab')^sub 2^ were less effective (p
Introduction
Outbreaks of influenza A virus (IAV) are one of the main causes of respiratory tract infection in the general population. They are also responsible for a high mortality rate among elderly persons and in immunocompromised patients.1 Influenza virus A is considered as a major incapacitating agent for the armed forces.2 Inactivated vaccines are able to control the spread and the severity of influenza infection, but the constant antigenic change of the viruses associated with the poor protective effect of vaccine explains the efforts currently under way to develop new strategies of protection.3
Chemical compounds such as amantadine, rimantadine, and zanamivir are effective in preventing influenza A virus infection,4 but they are not always efficient because resistant strains emerge.5 They must be administered in short delay after contamination. In addition, amantadine has unwanted neurological side effects. Administration of a single dose of intravenous (Iv) Ig or F(ab')^sub 2^ is efficient for the treatment and the prophylaxis of IAV infection.6 Duration of protection has been demonstrated for administration of these antibodies performed 24 hours before challenge. Immunoprophylaxis could be an attractive alternative for the control of flu. The risk of transmission of blood-borne pathogens is not well evaluated. To reduce the doses of antibodies used and amount, and this putative infectious risk, a new monoclonal human antibody has been recently produced in France by Technopharm Laboratories (Paris, France).
In this study, we are presenting the first results obtained with this antibody for the prophylaxis of a lethal flu infection in mice. Results were compared with those obtained by IvIg, F(ab')^sub 2^, amantadine, and zanamivir.
Materials and Methods
Viral Strain
The IAV was strain A/Scotland/74 (H3N2). It was initially isolated from a patient and grown in MDCK cells. This strain has never been cultured in eggs. Because mice are not natural hosts for the influenza virus, it was adapted to BALB/c mice by serial lung passages.6
Virus stock for respiratory infection was prepared from lung homogenates of infected mice, diluted in PBS (Sigma-Aldrich, Saint Quentin Fallavier, France), and stored at -80 deg C until use. Infectious titer of the virus stock was quantified on MDCK cells. Initial concentration was 2 x 101 plaque-forming units (pfu)/ml.
The doses necessary to achieve 100% mortality (LD^sub 100^) and 50% mortality (LD^sub 50^) 10 days after infection were determined after intranasal infection of 20 BALB/c mice per group. LD^sub 100^ was obtained with 2 x 10^sup 5^ pfu/ml and LD^sub 50^ with 5 x 10^sup 4^ pfu/ml.
Mice
Female BALB/c mice (Charles River Breeding Laboratories, Saint-Aubin-les-Elbeuf, France) were maintained under pathogen-free conditions until they were used at the age of 5 to 6 weeks.
Human Polyvalent Immunoglobulins (IvIg)
Human polyvalent immunoglobulins IvIg) were obtained from Biotransfusion (Les Ulis, France: IvIg lot 500 750 20). F(ab')^sub 2^ were obtained from les Laboratoires Francais du Fractionnement et des Biotechnologies (Les Ulis, France). They then underwent pepsin digestion and purification by Staphylococcus aureus protein A-Sepharose chromatography (Affi-gel Hz immunoaffinity kit, Bio-Rad, Ivry-sur-Seine, France).
IvIg and F(ab')^sub 2^ were diluted in PBS. Stock preparations (50 (mu)g/(mu)l for IvIg and 30 (mu)g/(mu)l for F(ab')^sub 2^) were then stored at -80 deg C.
Antibody Titration
Titration of IvIg and F(ab')^sub 2^ against the influenza viral strain was done by means of a commercially available hemagglutination inhibition (HI) test. In brief, 25 (mu)l of serial dilution of IvIg or of F(ab')^sub 2^ were mixed in round-bottom polystyrene microtiter plates with 25 (mu)l of HA antigens (906013 strain A/Kumamoto/ 22/76 and 906014 strain B/Kanagawa/3/76, Laboratoires Eurobio, Paris, France) standardized at 4 hemagglutination units. The mixture was incubated for 1 hour at room temperature prior to the addition of 50 (mu)l of 1% chicken erythrocytes. Plates were then agitated slightly and the HI titer was recorded after 1 hour of incubation at room temperature. HI titer was 1/8 against influenza A and 1/64 against influenza B, in both IvIg and F(ab')^sub 2^.(6)
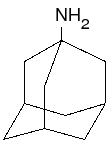
Production of Human Monoclonal Antibodies (Mab)
Human B lymphocyte Production
Human Mab were produced as follows: Patients (volunteers) were immunized with antiflu vaccine or were patients recovering from an influenza infection. Blood punctures were done at day 0, 8, 15, or 21 after vaccination on EDTA tubes. A half dilution of the blood was done in PBS. Diluted blood has been then added to the medium for lymphocytes separation (MI 7829E, BioWhittaker-Cambrex, Emerainville, France). The ratio was 1:3 medium and 2:3 blood. Centrifugation was done at 3000 rpm for 20 minutes. The lymphocyte ring was then slowly recovered, and cells were transferred in RPMI 1640 medium containing 1% L-glutamine, 0.1% gentamicin, 50 (mu)M 2-mercaptoethanol, and 10% fetal calf serum (complete RPMI 1640). The suspension was then centrifuged at 1300 rpm for 6 minutes. Supernatant was removed and pellet was suspended in complete RPMI 1640 to obtain a final concentration of 1 to 2 x 10^sup 6^ cells/ml. Cell suspensions were cultured overnight (37 deg C, 5% CO^sub 2^ to allow monocyte adhesion.
During the same time, sheep red blood cells were added to 2-aminoethyl-isothiouronium bromide (AET, Sigma-Aldrich) at the ratio (v/v) 1:4. The mixture was incubated for 1 hour at 37 deg C and 5 mL of PBS were added. After a 10-minute centrifugation at 1300 rpm, the supernatant was removed. An aliquot of the pellet (red blood cells and AET) was suspended in complete RPMI 1640. The preparation was incubated overnight at 4 deg C.
Lymphocytes from human white blood cell cultures were recovered and diluted in an equal volume of 4% sheep red blood cells-AET. A half volume of fetal calf serum was then added. After slight homogenization, the mixture was centrifuged at 800 rpm for 5 minutes and left I hour in an ice bath (0 deg C). The supernatant was then removed and the pellet was suspended in media for lymphocyte separation (1/3 media:2/3 pellet). As previously described, the lymphocyte ring was aspirated and suspended in 15 mL of complete RPMI 1640. The pellet was washed twice in complete RPMI 1640 to obtain cells ready for culture.
Plasmocytes differentiation
After the addition of 0.04% Pansorbine and 2.5 ng/ml interleukin (IL) 2, cells were incubated for 3 days (37 deg C, 5% CO2). After centrifugation, the pellet was suspended in complete RPMI 1640 and cells were redistributed in cell culture dishes. IL-2 (2.5 ng/ml) and IL-10 (100 ng/ml) were then added and cells were cultured for 5 days (37 deg C, 5% CO2).
Cell Fusion
Plasmocyte cells were recovered after centrifugation (6 minutes, 1200 rpm). They were then mixed with IR 983 F/TEC myeloma cells6 in minimal essential medium REGA3 (19993-- 013, Life Technologies, Cergy Pontoise, France). The cell ratio was 1:1. Cells were then recovered after centrifugation. Fusion was done after suspension of the cells in 1 mL of polyethylene glycol 4000 (7 mL of PBS, 5 g of polyethylene glycol, and 1 mL of dimethylsulfoxide). Culture of single hybridoma cells was performed in Dulbecco's modified Eagle's medium (M12914F, BioWhittaker).
Immunoglobulins were recovered after separation in a Sepharose column containing human anti-K and anti-lambda antiglobulins (TEC 146 and 147, Technoparm).7
Characterization of the Mab
The supernatants of the hybridoma were characterized by the enzyme-linked immunosorbent assay method.
Isotype Detennination
Wells were coated with anti-human IgG or IgM monoclonal rat antibodies (LO-HM-7 batch 4923 or LO-HG-24 batch 5700, Technopharm, Paris, France). After saturation, immune complexes were revealed by rat peroxidase-labeled Mab directed against human kappa or lambda light chains (LO-HK-3 batch 5330 or LO-HL2 batch 4451, Technopharm).
Positive control was a human serum from an immunized volunteer. Negative control was the culture cell medium.
Determination of Specificity
Antibodies were tested for specificity against three influenza virus strains: H1N1 (A/Beijing/262/95X-127), H3N2 (A/Sidney/5/97 IVR-108), and B (B/Harbin/7/94). After saturation, immune complexes were revealed by rat peroxidase-labeled Mab directed against human kappa or lambda light chains (LO-HK-3 batch 5330 or LO-HL2 batch 4451, Technopharm).
Positive control was a human serum from an immunized volunteer. Negative control was the culture cell medium.
Mice Infection
The protocol used for infection with influenza virus has been previously described.5 Mice, grouped by 10, were anesthetized by a light inhalation of ether and were inoculated intranasally with 50 (mu)l of a virus suspension containing LD^sub 100^. Prophylaxis treatments were applied with chemical compounds or with antibodies as described in "Local Passive Immunotherapy" and "Chemoprophylaxis." A control group of 10 mice was infected with LD^sub 100^ IAV alone.
Morbidity and Mortality
Mortality was observed during 14 days. Daily assessments for weight was made during a 10-day period.
When all of the mice survived, the effectiveness of the different treatments was estimated, in each group, by the comparison of the difference of the mean of the weight of all of the animals observed during the entire period.
Local Passive Immunotherapy
Antibodies were administered intranasally to the anesthetized mice to deliver topically the compounds in the lungs. Mab used for passive prophylaxis were administered 1 day before infection at the single dose of 20 (mu)g/mouse (1. 1 mg/kg). Selection of antibodies is described in "Specificity Determination." IvIg and F(ab')^sub 2^ were administered as follows: IvIg: a single dose of 3.7, 7.5, 15, 30, or 60 mg/kg was administered at 3, 6, 18, 24, 48, 72, or 96 hours and 7 days before infection. F(ab')^sub 2^: a single dose of F(ab')^sub 2^ was administered at 24, 48, or 72 hours before the viral infection. Doses used were 3, 6, 9, or 18 (mu)g/kg.
Chemoprophylaxis
Zanamivir (Relenza, Glaxo Wellcome Production, France) was administered intranasally twice a day at the regimen of 5 or 25 mg/kg 24 hours before infection and then twice daily for 5 days beginning after infection.8 Amantadine (Symmetrel, DuPont Merck Pharma, Quebec, Canada) was given orally starting 1 day before experimental infection until 5 days after, at the dose of 600 mg/kg once per day.
Both chemical compounds were used as reference for the effectiveness of prophylaxis.8-13
Statistical Analyses
The weight of the mice was compared using Student's t test. Results were interpreted using the Fisher and Yates tables.
Definition of Protection
Since experiments were done with a lethal infectious dose, mice were considered as protected when they survived the infection.
Results
MAb
Isotype Determination
Seven IgM kappa and three IgM lambda were produced: IgM kappa were FAL11-1A9, 1D8, 1G8, 1H2, 1H4,2G7,3B1.IgMA were FALL112C3, 3D2, and FAL8-1G4.
Specificity Determination
Among the 10 antibodies, only three, FAL11-2C3, 3D2, and FAL8-IG4, had specificity against A(H3N2), A(H1N1), and B influenza viruses. These three antibodies were evaluated for prophylaxis in mice.
FAL11-1A9, 1D8, 1G8, 1H2, 1H4, 2G7, and 31B1 did not interact with influenza antigens. FAL11 - 1A9 was used as negative control.
Protection Conferred by Mab
Among the three reactive clones of Mab tested, only FAL11 -- 2C3 was able to protect all of the mice from a lethal infection. FAL8- 1G4 protected four mice among the 10 infected. FAL11-- 3D2 did not protect the mice (Table 1).
IvIg and F(ab')^sub 2^
A single dose of 30 mg/kg protected all of the animals when administered up to 3 days before infection. The number of survivors decreased to 7 when the same regimen was given 96 hours before challenge. A dose of 15 mg/kg protected all of the animals if administered 6 hours before infection. The number of survivors decreased for longer time intervals: to 9 for 18 or 24 hours and to 6, 3, and 0 when the time intervals were 48, 72, and 96 hours, respectively.
Effectiveness of prophylaxis using 7.5 mg/kg was shorten to 18 hours and decreased rapidly after this time. A high dose of 60 mg/kg was able to protect eight animals if administered 7 days before infection (Table II).
F(ab')^sub 2^
All of the mice were protected against a lethal infection when they received 9 mg/kg F(ab')^sub 2^ 24 hours before challenge. Only three of those treated 3 days before infection with the same regimen were protected. A dose of 3 mg/kg was ineffective.
Compared to 9 mg/kg, a dose of 18 mg/kg doubled the number of survivors when administered at 72 hours (Table III).
Chemoprophylaxis
Both treatments using chemical drugs protected the mice from the lethal effect of the viral inoculum. The effective dose of zanamivir was 25 mg/kg administered twice a day for 6 days. The recommended dose for usual protection against flu (5 mg/kg twice a day) was ineffective in mice for the protection against a lethal infection: mortality was 100% with this regimen (data not shown). Amantadine also protected all of the animals.
Weight Loss Comparison
The comparison of weight observed during the 10-day period after infection (Fig. 1) showed differences between groups as demonstrated in Table IV. There was no statistical difference between IvIg and zanamivir (p = 0.07). This chemical compound was more effective than amantadine (p = 0.03). Treatment using F(ab')^sub 2^ was less effective (p
Protection conferred by the best Mab (FAL11-2C3) was similar to protection observed with amantadine. This Mab was, however, less efficient than both zanamivir (p
Discussion
Influenza A infection causes annual epidemics that affect all age groups and spreads rapidly throughout the population. The economical cost of these outbreaks is very important for the community.14 The best prophylaxis remains vaccination but most cases of flu infection are among nonvaccinated adults and spontaneous mutation of hemagglutinin and neuraminidase can render this vaccination ineffective. During a flu outbreak, it would be of great interest to protect urgently nonvaccinated individuals and immunocompromised patients against viral infection. The intranasal route seems to be the easiest means of administration.
Immunotherapy has been demonstrated to be effective in the treatment of IAV infection,15,16 but its effectiveness in prophylaxis after local intranasal administration has not been tested for instillation performed more than 24 hours before infection.5 Human Mab directed against influenza viruses have never been tested.
Chemical compounds such as zanamivir or amantadine are able to prevent flu infection when administered within 48 hours of illness onset. Both drugs reduce the severity and shorten the duration of the disease. The development of resistant strains has been published.5,17 In this study, zanamivir was used as positive control for the effectiveness of immunoprophylaxis against IAV infection. The dose used as control was 25 mg/kg/ day. It was chosen because mice were not protected against the lethal effect with a regimen of 5 mg/kg/day, Prophylaxis of physiological infection with this dose, however, gave statistically significant reduction in lung virus titers.9
When administered before a lethal infection, passive immunoprophylaxis with all types of antibodies prevented mortality in mice due to a lethal infection. The effectiveness of IvIg and F(ab')^sub 2^ suggests an immunological mechanism by neutralizing the viral binding. This involves a specific interaction between the antibody and the viral particles at the extracellular stages of infection. Both IvIg and F(ab')^sub 2^ have hemagglutinin specificity and inhibit, in vitro, viral hemagglutination. Their effectiveness might be reduced if a new viral strain emerged expressing a new hemagglutinin type. The comparison of weight loss and duration of protection after treatment demonstrate that IvIg was more effective than F(ab')^sub 2^. This difference in duration might be explained by the shorter half-life of F(ab')^sub 2^ in the respiratory tract. This suggests that it might be preferable to use IvIg instead of F(ab')^sub 2^ .
Comparison of weight loss demonstrates that results obtained with IvIg were identical to those obtained with zanamivir, but IvIg simply required a single administration for a 3-day period to achieve protection. Among the monoclonal IgM tested, only FAL11-2C3 was able to confer total protection against IAV. In comparison, FAL8-1G4 had a poor effectiveness. These anti-- bodies were both IgM lambda and did not inhibit hemagglutination in vitro. The effectiveness of FAL11-2C3 on lethality in the model and its ability to interact with influenza antigens demonstrates that this antibody can confer protection against the viral strain used in this experimental protocol. The most interesting fact to observe is that this antibody is not directed against hemagglutinin or neuraminidase. The protection mechanism is not, at this time, clearly established but a nonspecific activity against chicken egg proteins do not seem possible because B cells were cultured in a RPMI 1640-based medium and because virus stock used for infection was obtained from lung homogenates of infected mice. With the lack of antihemagglutinin or antineuraminadase activity, effectiveness could be simply explained by the facilitation of phagocytosis.
The others Mab were not efficient and FALB-1G4, which was not able to protect mice even if reacting in vitro with influenza antigens, was considered as a IgM negative control. Monoclonal IgG were not tested because at this time it was not possible for us to produce such a class of antibodies. Protection by instillation of Mab performed 48 and 72 hours before infection was not tested because of the impossibility, at that time, to produce enough monoclonal human antibodies.
The prophylactic protection obtained with IvIg or IgM demonstrated that both classes of immunoglobulins were able to block the viral infectious process when administered topically. Mazanec et al.18 showed equivalent activities of monoclonal IgG and IgA in protecting the lower respiratory tract of mice infected by the Sendai virus. Because bacterial superinfections are a very frequent complication of flu infection, local passive immunoprophylaxis could also be a good complementary approach for their prevention.
At this time, polyvalent immunoglobulins gave better results than Mab. We hope for better results and work is underway to optimize their preparation. Usually Mab have a higher affinity and a higher specificity than IvIg.19-22 Viral resistance to Mab is possible and many clones should be simultaneously used in commercial preparations. In contrast, IvIg contain a variety of antibodies directed against multiple infectious agents, including influenza viruses of various types and are currently available. In comparison with IvIg, protection by Mab required a dose 20 times lower.
Conclusion
The constant emergence of new IAV associated with the economic cost of epidemics has renewed interest in passive prophylaxis immunization. In this protocol, intranasal administration of antibodies has shown great promise against flu infection and the best results were obtained with IvIg. The Mab presented in this study was able to protect against a lethal inoculum but the weight loss comparison demonstrated that new clones have to be developed. They will be used in combination on the same model to obtain optimum protection and to prevent the hypothetical emergence of resistant strains.
Acknowledgments
We gratefully acknowledge Alan Talmon for his help in the redaction of this manuscript.
References
1. Kaiser L, Hayden FG: Hospitalizing influenza in adults. Curr Clin Top Infect Dis 1999; 19: 112-34.
2. Laurel VL, De Witt CC, Geddie YA, et al: An outbreak of influenza a caused by imported virus in the United States, July 1999. Clin Infect Dis 2001: 32: 1639-42.
3. Saito H, Takenaka H, Yoshida S, et al: Prevention from naturally acquired viral respiratory infection by interferon nasal spray. Rhinology 1985: 23: 291-5.
4. Wilson SZ, Knight V, Wyde PR, Drake S, and Couch RB: Amantadine and ribavirin aerosol treatment of influenza A and B infection in mice. Antimicrob Agents Chemother 1980; 17: 642-8.
5. Barnett JM. Cadman A, Burrell FM, et al: In vitro selection and characterisation of influenza B/Beijing/1/87 isolates with altered susceptibility to zanamivir. Virology 1999; 265: 286-95.
6. Ramisse F, Deramoudt FX, Szatanik M, et al: Effective prophylaxis of influenza A virus pneumonia in mice by topical passive immunotherapy with polyvalent human immunoglobulins or F(ab')2 fragments. Clin Exp Immunol 1998; 111: 583-7.
7. Bazin H: Production of rat monoclonal antibodies with the LOU rat nonsecreting IR983F myeloma cell line. In: Protides of the Biological Fluids, pp 615-18. Edited by Peeters H. Oxford, Pergamon, 1982.
8. Gubareva LV, McCullers JA, Bethell RC, Webster RG: Characterization of influenza A/Hong Kong/ 156/97 (H5NIJ virus in a mouse model and protective effect of zanamivir on HSN 1 infection in mice. J Infect Dis 1998; 178: 1592-6.
9. Fenton RJ, Morley PJ, Owens IJ, et al: Chemoprophylaxis of influenza A virus infections with single doses of zanamivir demonstrates that zanamivir is cleared slowly from the respiratory tract. Antimicrob Agents Chemother 1999; 43: 2642-7.
10. Hayden FG: Prevention and treatment of influenza in immunocompromised patients. Am J Med 1997; 102: 55-60.
11. Kaiser L, Keene ON, Hammond JM, Elliott M, Hayden FG: Impact of zanamivir on antibiotic use for respiratory events following acute influenza in adolescents and adults. Arch Intern Med 2000; 160: 3234-40.
12. Kaiser L. Henry D, Flack NP, Keene 0, Hayden FG: Short-term treatment with zanamivir to prevent influenza: results of a placebo-controlled study. Clin Infect Dis 2000; 30: 587-9.
13. Monto AS, Robinson DP, Herlocher ML. Hinson JM Jr., Elliott MJ, Crisp A: Zanamivir in the prevention of influenza among healthy adults: a randomized controlled trial. JAMA 1999; 282: 31-5.
14. Demicheli V, Jefferson T, Rivetti D, Deeks J: Prevention and early treatment of influenza in healthy adults. Vaccine 2000: 18: 957-1030.
15. Treanor JJ, Tierney EL, Zebedee SL, Lamb RA, Murphy BR: Passively transferred monoclonal antibody to the M2 protein inhibits influenza A virus replication in mice. J Virol 1990; 64: 1375-7.
16. Tamura S, Funato H, Hirabayashi Y, et al: Cross-protection against influenza A virus infection by passively transferred respiratory tract IgA antibodies to different hemagglutinin molecules. Eur J Immunol 1991: 21: 1337-44.
17. Houck P, Hemphill M, LaCroix S, Hirsh D, Cox N: Amantadine-resistant influenza A in nursing homes: identification of a resistant virus prior to drug use. Arch Intern Med 1995; 155: 533-7.
18. Mazanec MB, Lamm ME, Lvn D. Portner A, Nedrud JG: Comparison of IgA versus IgG monoclonal antibodies for passive immunization of the murine respiratory tract. Virus Res 1992; 23: 1-12.
19. Mozdzanowska K, Furchner M, Washko G, Mozdzanowski J, Gerhard W: A pulmonary influenza virus infection in SCID mice can be cured by treatment with hemagglutinin-specific antibodies that display very low virus-neutralizing activity in vitro. J Virol 1997; 71: 4347-55.
20. Mozdzanowska K, Maiese K, Furchner M, Gerhard W: Treatment of influenza virus-infected SCID mice with nonneutralizing antibodies specific for the transmembrane proteins matrix 2 and neuraminidase reduces the pulmonary virus titer but fails to clear the infection. Virology 1999; 254: 138-46.
21. Virelizier JL: Host defenses against influenza virus: the role of anti-hemagglutinin antibody. J Immunol 1975; 115: 434-9.
22. Okuno Y, Matsumoto KI, Isegawa Y. Ueda S: Protection against the mouse adapted A/FM/ 1/47 strain of influenza A virus in mice by a monoclonal antibody with cross neutralizing activity among HI and H2 strains. J Virol 1994; 68: 517-20.
Guarantor: Eric Hernandez, MD PhD
Contributors: Francoise Ramisse, PhD*; Anne Lhonneux, PhD^; Jacques Noury, PhD^; Herve Bazin, MD^; Jean-Didier Cavallo, MD^^; Eric Hernandez, MD PhD^^
*Centre d'Etudes du Bouchet, Laboratoire de Microbiologie. BP3, 91710 Vert-le-- Petit, France.
^Laboratoires Technopharm, 25 Bvd Saint-Jacques, 75014 Paris, France.
^^Hopital d'Instruction des Armees Begin. Laboratoire de Biologie, 69 avenue de Paris, 94160 Saint-Mande, France.
This manuscript was received for review in May 2002 and accepted for publication in June 2002.
Reprint & Copyright (c) by Association of Military Surgeons of U.S., 2003.
Copyright Association of Military Surgeons of the United States Mar 2003
Provided by ProQuest Information and Learning Company. All rights Reserved