Insulin remains the preferred method for treatment of type 2 diabetes during pregnancy, providing the glycemic control required to prevent the severe birth defects, toxicity, pregnancy losses, and complications associated with poorly controlled diabetes during pregnancy.
Gestational diabetes mellitus (GDM) is not associated with an increased incidence of birth defects, but can be associated with the characteristic toxicities of the diabetic milieu. Insulin remains the treatment of choice for GDM, but this may change: Evidence that glyburide is a safe, effective, and less costly alternative to insulin in some patients with GDM is accumulating.
Overall, oral antidiabetic agents are a diverse group of drugs, which in general should be avoided during organogenesis because of insufficient data on their use in human pregnancy.
* First-generation sulfonylureas. These include chlorpropamide and tolbutamide, which are not thought to cause congenital defects, but more studies are needed before they are completely excluded as possible teratogens. These agents have long elimination half-lives (up to 36 hours) and long durations of action. They cross the placenta and may cause persistent hyperinsulinemia and hypoglycemia in the newborn.
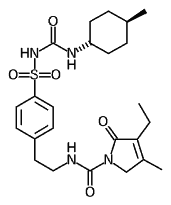
* Second generation sulfonylureas. Glipizide (Glucotrol and generic formulations) and micronized glyburide (Micronase and generic formulations) have shorter half-lives than do nonmicronized glyburide and glimepiride (Amaryl) (2-4 hours vs. 9-10 hours). There appears to be much less fetal exposure with glyburide and glipizide than with the first-generation agents chlorpropamide and tolbutamide, probably because second-generation drugs have shorter elimination times and higher protein binding. There has not been enough experience during organogenesis to assess the teratogenic potential of second-generation sulfonylureas, so they should not be used in pregnancy to treat type 2 diabetes.
Several studies of glyburide treatment of GDM starting late in the second trimester demonstrated benefits in terms of glycemic control and cost. Although more data are needed, glyburide may offer a clinically beneficial alternative to insulin in the treatment of GDM.
* Alpha-glucosidase inhibitors. First-trimester experience with acarbose (Precose) and miglitol (Glyset), which lower postprandial hyperglycemia by delaying glucose absorption, is very limited, so they are not recommended for the treatment of type 2 diabetes in pregnancy or GDM. They have been used for GDM, but patient tolerance is a major limiting factor. (Flatulence, diarrhea, and abdominal pain are common side effects.)
* Biguanides. Spontaneous ovulation and conception may occur with use of metformin, which is frequently used to treat polycystic ovary syndrome. In developing countries, where the proper use of insulin is often problematic, metformin has been used in pregnancy, sometimes in combination with sulfonylureas, for the treatment of GDM. However, this is not recommended in developed countries because the long-term effects and safety of the drug have not been adequately studied. Exposure to metformin during organogenesis has not been associated with an increase in the incidence of birth defects.
* The meglitinides. Nateglinide (Starlix) and repaglinide (Prandin), insulin secretagogues, have very short elimination half-lives (1-1.5 hours) and high plasma protein binding (98% or more)--features that limit the amount of drug transferred to the embryo and fetus. Although animal data suggest that inadvertent exposure early in gestation probably does not represent a major risk for the embryo, there is no human pregnancy experience with these agents, so they should not be used in pregnancy.
* Thiazolidinediones. Pioglitazone (Actos) and rosiglitazone (Avandia) decrease insulin resistance. Transfer of these drugs across the placenta is limited by their extensive plasma protein binding. However, pioglitazone has three active metabolites, with long elimination half-lives, suggesting that these metabolites may cross the placenta. Because of very limited human pregnancy experiences, these drugs are not recommended for pregnant diabetics. Neither is teratogenic in animals, so the risk from inadvertent exposure early in gestation is probably very low.
During lactation, four of the sulfonylureas (chlorpropamide, tolbutamide, glipizide, and glyburide), acarbose, and metformin appear to be compatible with breast-feeding. The other agents have not been studied during this period and are best avoided.
BY GERALD G. BRIGGS, B.PHARM.
GERALD G. BRIGGS, B.Pharm., is pharmacist clinical specialist, Women's Hospital, Long Beach (Calif.) Memorial Medical Center; clinical professor of pharmacy, University of California, San Francisco; and adjunct professor of pharmacy, University of Southern California, Los Angeles. He is also coauthor of the reference book "Drugs in Pregnancy and Lactation."
COPYRIGHT 2004 International Medical News Group
COPYRIGHT 2004 Gale Group