Vascular birthmarks are commonly encountered in children and are classified as either hemangiomas or vascular malformations[1,2] (Table 1). Hemangiomas are benign neoplastic proliferations of vascular endothelial cells characterized by spontaneous involution. In contrast, vascular malformations are not neoplasms but permanent morphogenic abnormalities of capillaries, veins, arteries or lymphatic vessels. Flat lesions (vascular malformations) tend to persist, while raised lesions (hemangiomas) tend to regress.
Diffuse Neonatal Hemangiomas
Widely disseminated, 2 to 15 mm, red to blue-black papular hemangiomas present at birth should alert the clinician to the possibility of associated visceral hemangiomas in the syndrome of diffuse neonatal hemangiomatosis. Gastrointestinal, hepatic, central nervous system and pulmonary visceral hemangiomas may be present, and high-output cardiac failure may occur by two to nine weeks of age. Evaluation of these patients includes a complete blood count, auscultation for bruits, liver edge palpation, ultrasonographic or CT scans of suspicious areas and evaluation of urine and stool for occult blood. Treatment includes hepatic lobectomy (if the Ever is involved), vessel ligation or embolization, high-dose corticosteroids (2 to 4 mg per kg per day), interferon alfa-2a and treatment for high-output cardiac failure. Lesions spontaneously involute in some patients.
Benign Neonatal Hemangiomatosis
Cases of widespread cutaneous hemangiomas without visceral involvement are classified as benign neonatal hemangiomatosis. Extensive facial hemangiomas may be associated with intracranial involvement, and evaluation by CT or magnetic resonance imaging is mandatory to determine the presence of structural abnormalities of the brain.
Blue Rubber Bleb Nevus Syndrome
Infants with multiple cutaneous cavernous hemangiomas may have concurrent gastrointestinal tract hemangiomas in the blue rubber bleb nevus syndrome. Painful, soft, compressible, 1.0 to 50 mm blue rubbery nodules with a wrinkled surface are present at birth and increase both in size and number with age.[10] Manual compression of these lesions expresses blood, leaving behind an empty wrinkled sac that rapidly refills. Small intestinal or colonic hemangiomas may be suspected in patients with anemia or positive stool guaiac specimens. Surgical excision of symptomatic cutaneous or gastrointestinal lesions remains the treatment of choice. Sclerosing techniques and laser irradiation may also be useful, but corticosteroids are ineffective.
Cobb Syndrome (Cutaneomeningospinal Angiomatosus)
Lumbosacral hemangiomas or port-wine stains may be associated with underlying spinal angiomas in Cobb syndrome (cutaneomeningospinal angiomatosus). Neurologic symptoms usually develop in later childhood or adolescence, but early spinal angiography may detect spinal angiomas, which may be surgically excised more easily before they have enlarged.
Maffucci's Syndrome (Hemangiomatosis Osteolytica)
Maffucci's syndrome (hemangiomatosis osteolytica) is a congenital syndrome characterized by hemangiomas at birth, skeletal deformities and enchondromas (benign cartilagenous growths). Malignant degeneration occurs in both the enchondromas and hemangiomas, and suspicious lesions should be biopsied. Diagnosis of this syndrome is confirmed by clinical, radiographic and pathologic evidence of hemangiomas and enchondromas.[11] Treatment is symptomatic, and the vascular lesions respond to surgery, irradiation and sclerotherapy. Orthopedic evaluation of bony abnormalities is especially important in the adolescent period.
Treatment
In general, the goals of hemangioma treatment are to prevent loss of life or function, and to prevent scarring, either before or as a result of therapy. The physician should also consider psychosocial issues when deciding on the best course of treatment, Most hemangiomas require no specific therapy other than patient education and reassurance. Frequent follow-up of an infant with a growing hemangioma will ensure adequate treatment of potential sequelae. Spontaneous involution often leads to ulceration; however, permanent scarring occurs in less than 5 percent of children affected with ulceration.
Bleeding and infection also complicate involution and should be treated with direct pressure, wet compresses and antibacterial soap, and oral antibiotics when cellulitis is present.[12] Treatment with FPDL and topical antibiotics may hasten recovery. Less than 10 percent of hemangiomas require therapy for specific indications[2,3,12] (Table 2). Although the therapeutic management of hemangiomas has included cryotherapy and radiation therapy, these methods have been surplanted by steroids, interferon alfa-2a, laser, surgery, embolization, sclerosing agents and antifibrinolytics.
The carbon dioxide laser is effective in treating subglottic hemangiomas unresponsive to corticosteroids and may prevent the need for tracheostomy in patients with airway obstruction. Because of the increased risk for scarring with both carbon dioxide and argon lasers, these lasers are not recommended in the initial treatment of cutaneous hemangiomas. Application of eutectic mixture of local anesthetic (EMLA) cream is effective in reducing the pain associated with FPDL treatment; however, the Nd:YAG, carbon dioxide and argon lasers require local or general anaesthesia.[5]
Surgery. Surgical excision is occasionally advocated as primary treatment of hemangiomas. Surgical excision is dearly indicated in the management of visceral or ocular lesions unresponsive to corticosteroids, and in the cosmetic revision of redundant skin remaining after spontaneous involution of deeper hemangiomas.[12,20] Embolization is a primary treatment for inoperable lesions, and it may be used preoperatively to minimize intraoperative blood loss. Potential side effects include cerebrovascular accident from the backflow of particles into the internal carotid artery.
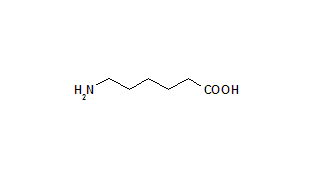
Antifibrinolytics. Aminocaproic add (Amicar) and tranexamic acid (Cyclokapron) are antifibrinolytic agents with limited roles in the treatment of Kasabach-Merritt syndrome that is unresponsive to high-dose corticosteroids or interferon alfa-2a therapy.[5] These agents inhibit plasminogen activator and plasmin. Side effects include nausea, vomiting, diarrhea and, in the case of aminocaproic add, rare instances of renal insufficiency and myopathy.
Figure 3a supplied by Eric A. Wulfsberg, M. D., Director of Dysmorphology and Clinical Genetics, University of Maryland School of Medicine, Baltimore.
REFERENCES
[1.] Mulliken JB, Glowacki J. Hemangiomas and vascular malformations in infants and children: a classification based on endothelial characteristics. Plast Reconstr Surg 1982;69:412-22.
[2.] Weston WL, Lane AT. Pediatric and geriatric dermatology In: Fitzpatrick TB, ed. Dermatology in general medicine. 4th ed. New York: McGraw-Hill, 1993:2949-51.
[3.] Hurwitz S. Vascular disorders of infancy and childhood. In: Hurwitz S. Clinical pediatric dermatology: a textbook of skin disorders of childhood and adolescence. 2d ed. Philadelphia: Saunders, 1993:242-77.
[4.] Gloviczki P, Stanson AW, Stickler GB, Johnson CM, Toomey BJ, Meland NB, et al. Klippel-Trenaunay syndrome: the risks and benefits of vascular interventions. Surgery 1991;110:469-79.
[5.] Alster TS, Wilson F. Treatment of port-wine stains with the flashlamp-pumped pulse dye laser: extended clinical experience in children and adults. Ann Plast Surg 1994;32:478-84.
[6.] Sherwood KA. The use of topical anesthesia in removal of port-wine stains in children. J Pediatr 1993;122(5 Pt 2):S36-40.
[7.] Amir J, Metzker A, Krikler R, Reisner SH. Strawberry hemangioma in preterm infants. Pediatr Dermatol 1986;3:331-2.
[8.] Liang MG, Frieden IJ. Perineal and lip ulcerations as the presenting manifestation of hemangioma of infancy. Pediatrics 1997;99:256-9.
[9.] Enjolras O, Mulliken JB. The current management of vascular birthmarks. Pediatr Dermatol 1993;10:311-3.
[10.] Moodley M, Ramdial F. Blue rubber bleb nevus syndrome: case report and review of the literature. Pediatrics 1993;92:160-2.
[11.] Collins PS, Han W, Williams LR, Rich N, Lee JF, Villavicencio JL. Maffucci's syndrome (hemangiomatosis osteolytica): a report of four cases. J Vasc Surg 1992;16:364-71.
[12.] Fishman SJ, Mulliken JB. Hemangiomas and vascular malformations of infancy and childhood. Pediatr Clin North Am 1993;40:1177-200.
[13.] Sloan GM, Reinisch JF, Nichter LS, Saber WL, Lew K, Morwood DT. Intralesional corticosteroid therapy for infantile hemangiomas. Plast Reconstr Surg 1989;83:459-67.
[14.] Bilyk JR, Adamis AP, Mulliken JB. Treatment options for periorbital hemangioma of infancy. Int Ophthalmol Clin 1992;32:95-109.
[15.] Schweigerer L, Fotsis T. Angiogenesis and angiogenesis inhibitors in paediatric diseases. Eur J Pediatr 1992;151:472-6.
[16.] Morad AB, McClain KL, Ogden AK. The role of tranexamic acid in the treatment of giant hemangiomas in newborns. Am J Pediatr Hematol Oncol 1993;15:383-5.
[17.] Ezekowitz RA, Mulliken JB, Folkman J. Interferon alfa-2a therapy for life-threatening hemangiomas of infancy. N Engl J Med 1992;326:1456-63 [Published erratum appears in N Engl J Med 1994; 330:300 and 1995;333:595-6].
[18.] Ettlinger JJ, Fleming PJ, Joffe HS, Kennedy CT Cavernous haemangioma with Kasabach-Merritt syndrome: treatment with alpha-interferon. J R Soc Med 1996;89:55P-6P.
[19.] Landthaler M, Hohenleutner U, el-Raheem TA. Laser therapy of childhood haemangiomas. Br J Dermatol 1995;133:275-81.
[20.] Wagner A. Lumps and bumps in childhood. Curr Prob Derm 1996;8:137-88.
FERN A. WIRTH, M.D., is chief resident in dermatology at the University of Maryland School of Medicine, Baltimore. Dr. Wirth is a graduate of Tufts University School of Medicine, Boston, and completed a residency in internal medicine at New England Deaconess Hospital, also in Boston.
MARK H. LOWITT, M.D., is assistant professor of dermatology at the University of Maryland School of Medicine and chief of dermatology at the Veterans Affairs Medical Center in Baltimore. Dr. Lowitt graduated from Tulane University School of Medicine, New Orleans, and completed residencies in internal medicine at New England Deaconess Hospital in Boston and in dermatology at the University of Maryland School of Medicine.
Address correspondence to Fern A. Wirth, M.D., University of Maryland Department of Dermatology 405 W Redwood St., 6th Floor Baltimore, MD 21201. Reprints are not available from the authors.
COPYRIGHT 1998 American Academy of Family Physicians
COPYRIGHT 2000 Gale Group