Background: Assessment of quality of life has become an increasingly important aspect of the risk-benefit analysis of any therapeutic intervention, particularly in high-risk populations, such as the elderly. Methods: Clinical outcomes of 147 consecutive patients older than 75 years undergoing valve surgery between 1992 and 1995 were reviewed. Long-term quality of life was assessed using a modified version of the Duke University Medical Outcomes Study system. Results: Mean age was 79.3 [+ or -] 4 years, range was 75 to 89 years, and 67% (99/147) were male. Preoperatively, 128 patients (87%) were in New York Heart Association (NYHA) functional class III/IV. Fifty-two percent (77/147) of the operations were nonelective. Concomitant coronary artery bypass grafting was performed in 69 patients (47%). Thirty-day hospital mortality was 7.5% (11/147). Mean follow-up for 98% (133/136) of hospital survivors was 30 [+ or -] 13 months (range, 2 to 55 months). Actuarial survival at 55 months was 71 [+ or -] 6% -- equivalent to a general age-, race-, and gender-matched population reported in the Life Tables of the US National Center for Health Statistics. At the time of follow-up, 112 patients (96%) lived at home, 78% (91/116) defined their health between good to excellent, and 81% (93/114) stated that the operation improved their health status. Ninety-seven percent (112/116) were able to bathe and dress independently, 92% (104/113) could walk at least one block, and 88.5% (100/113) could climb at least one flight of stairs. Moderate to vigorous activities could be performed by 59.2% (67/113). Overall, at the time of follow-up, 81% (95/117) were in NYHA class I/II. Conclusion: In a selected patient population, valve surgery in the elderly is associated with acceptable early morbidity and mortality. Long-term survival and quality of fife are excellent. These facts strongly support the performance of these procedures in patients older than 75 years.
(CHEST 1997; 112:885-94) Key words: elderly; quality of life; valve surgery
Abbreviations: AVR=aortic valve replacement; CABG-corona artery bypass grafting; CPB=cardiopulmonary bypass; CVA=cerebrovascular accident; DVR=double valve replacement; LVEF=left ventricular ejection fraction; MI=myocardial infarction; MOS system=Medical Outcomes Study system; MVR=mitral valve replacement; NYHA=NEW York Heart Association
In the early 1990s, 3% (7.4) million of the US population were older than 80 years.[1] The current life expectancy of octogenarians is in the range of 6.0 to 8.1 years, leading to an expected rise in their number to [is greater than] 10 million (4.3%) within the next 10 years.[1-2] Of these octogenarians, 40% have serious symptomatic heart disease.[2] This trend is reflected in our institution by the increased fraction of elderly patients undergoing open heart surgery from 12 to 22% of total cases over the past decade.
Quality of life encompasses the total well-being of the person. Assessment of quality of life includes evaluation of functional capacity, symptoms, and the patient's perception of well-being.[3] In the era of managed care, quality of life has become an increasingly important end-point measure, being an integral part of the evaluation of the risk-benefit ratio and cost-effectiveness of a variety of therapeutic modalities. Advances in anesthetic and surgical techniques, as well as improved perioperative care, have resulted in a significant improvement in short- and long-term clinical outcome after open heart surgery in the elderly.[4-17], However, very little is reported on the effect of these operations on quality of life. The purpose of this study was to evaluate the clinical outcome of valve surgery in 147 patients older than 75 years undergoing valve surgery, focusing on long-term quality of life.
Materials and Methods
Patients
The study population consisted of 147 consecutive patients older than 75 years undergoing valve surgery in a tertiary teaching hospital between January 1992 and July 1995.
Surgical Techniques
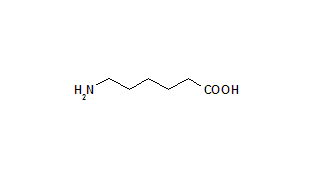
Operations were performed using cardiopulmonary bypass (CPB) and mild systemic hypothermia (34 [degrees] C to 35 [degrees] C). Myocardial protection was achieved using antegrade and retrograde cold (4 [degrees]) blood cardioplegia, supplemented by topical cooling with cold same solution. Aminocaproic acid (Amicar; American Reagent; Shirley, NY) was used routinely in this study. Departmental thresholds for homologous blood transfusion were defined as hematocrit of 20% during CPB and 25% postoperatively. Use of clotting factors was based on clinical assessment of bleeding and hematologic evaluation, specifically correcting factor deficits. Persistent bleeding in excess of 300 mL in the first hour or 500 mL in the first 2 h was considered an indication for transfusion of 5 to 10 U of platelets and 2 to 4 U of fresh frozen plasma. The departmental transfusion guidelines were rigid and did not change over the study period.
Data Collection
Hospital and clinical records were reviewed retrospectively. Data retrieved included the following: (1) demographic information -- age, gender, body surface area, indication for surgery, date of operation, surgeon, status of the procedure (elective vs urgent/emergent). We used the Society of Thoracic Surgeons criteria to define the status of the procedure.[18] Elective: an elective operation was one that was performed on a patient with cardiac function that had been stable in days or weeks prior to the operation. Urgent: an urgent operation was one in which surgery was required within 24 h in order to minimize the chance of further deterioration. Delay in operation was necessitated only by attempts to improve the patient's condition, availability of a spouse or a parent for informed consent, availability of blood products, or the availability of results of essential laboratory procedures or tests. Emergent: patients requiring emergency operations had ongoing, refractory unrelenting cardiac compromise, math or without hemodynamic instability, and were not responsive to any form of therapy except cardiac surgery. An emergency operation was one in which there was no delay in providing operative intervention.[18] (2) Preoperative left ventricular ejection fraction (LVEF) and functional status were determined by the New York Heart Association (NYHA) classification. (3) Comorbid risk factors included hypertension, diabetes mellitus, prior cerebrovascular disease, peripheral vascular disease, smoking, COPD, chronic renal failure (creatinine [is greater than] 2.5), dialysis, prior myocardial infarction, and preoperative use of anticoagulants. (4) Operative data included type of operation, concomitant procedures, type of CPB circuit, CPB and aortic cross-clamp times, use of inotropes and intra-aortic balloon pump, and intraoperative complications. (5) Postoperative complications included 30-day mortality, and significant morbidity was defined as reoperation for bleeding, mediastinal infection, pneumonia, respirator [is greater than] 3 days, transient ischemic attack and/or cerebrovascular event, myocardial infarction (new Q wave, and/or elevation of creatine phosphokinase MB [is greater than or equal to] 50 U), low cardiac output (a newly placed intra-aortic balloon pump or the use of inotropes for [is greater than] 24 h to maintain a cardiac index [is greater than] 2.0), valve thrombosis, and other major complications (vascular, GI, etc).[6] Bleeding and transfusion requirements were also noted.
Long-term Follow-up and Assessment of Quality of Life
Two questionnaires, one for patients and one for physicians caring for them, were developed to collect long-term results. Each questionnaire included a brief explanation of the project. The patient's questionnaire (Appendix 1) was based on the Duke University Medical Outcomes Study (MOS) system. To maximize the response rate, the questionnaire was kept as brief as possible, and consisted of three of the six items originally included in the MOS system. The focus was on functional capacity, the patient's perception of well-being, and the impact of surgery on overall health status. The physician questionnaire (Appendix 2) focused on long-term morbidity, mortality, and functional capacity as determined by NYHA classification. Patients, families, add/or physicians who failed to respond were directly contacted by phone to achieve as complete follow-up as possible.
Statistical Analysis
Statistical analysis was performed using the statistical software (SAS version 6. 11; SAS Institute; Cary, NC). Data are expressed as mean [+ or -] SD, and for selected variables also by the median and range. Two-tailed Student t test was used to analyze continuous variables. Categorical variables were analyzed Using [X.sup.2] with Yates' correction or Fisher's Exact Test when appropriate. A p value of [is less than] 0.05 was considered significant. Multivariate analysis using logistic regression was used to identify factors associated with early and late mortality. For the logistic regression analysis, the LOGISTIC procedure was utilized. A backward selection method was used to select the variables in the model, with a significance level for entry into the model of 0.1 and a significance level of 0.05 for staying in the model. Long-term survival was analyzed using the Kaplan-Meier method. The survival of the study group was compared to age-, race-, and gender-matched general US population, obtained from the Life Tables of the US National Center for Health Statistics,19 using the log rank test. All the calculations were performed using a procedure (SAS LIFETEST).
Results
Baseline Characteristics of the Study Group
The baseline clinical and operative profiles of the study group are summarized in Table 1. There were 99 men and 48 women with a mean age of 79.3[+ or -] 3.8 years (range, 75 to 89 years). Mean LVEF was 53.9[+ or -] 16.1% with 27% having LVEF of [is less than] 45%. Mean preoperative NYHA functional class was 3.3 [+ or -] 0.7 with 87% being in class III/IV. A significant number of patients had multiple comorbidities such as hypertension, coronary artery disease, smoking, diabetes, prior stroke, and others.
Aortic valve replacement (AVR) was performed in 105 patients mostly for senile calcific aortic stenosis; mitral valve repair (n=9) or replacement (n=21) (MVR) was performed in 30 patients, one third of whom had ischemic mitral regurgitation; and double valve replacement (DVR) procedures were performed in 12 patients. Concomitant coronary artery bypass grafting (CABG) was performed in 69 patients (47%). More than 50% of the operations (73/147) were nonelective, and 9% were reoperations. Bioprostheses were implanted in most patients (121/147 [82%]). There was no significant difference between mechanical valves and bioprostheses with regards to the size of the prosthesis implanted: AVR prosthesis size -- mechanical: 20.6 [+ or -] 2 mm vs bioprosthesis: 21.6 [+ or -] 3 mm (p=0.36); MVR prosthesis size -- mechanical: 30.0 [+ or -] 4 mm vs bioprosthesis: 28.8 [+ or -] 3 (p=0.46). Conventional CPB circuits were used in 91 patients and heparin-bonded circuits were used in 56.
[TABULAR DATA NOT REPRODUCIBLE IN ASCII]
Early Mortality and Morbidity
Early clinical outcomes are summarized in Table 2. Thirty-day operative mortality was 7.5% (11/147). The causes of hospital deaths included the following: CVA, two patients; ischemic bowel, two patients; coagulopathy, two patients; aortic dissection, postinfarction ventricular septal defect, perioperative myocardial infarction (MI), multiorgan failure, and atrioventricular rupture each in one patient. Patients with bioprostheses had a mortality of 5.8% (7/121), and patients with mechanical valves had a mortality of 23.5% (4/17), p=0.04. The causes of deaths in patients with mechanical valves included CVA in two patients, atrioventricular rupture, and multiorgan failure. The causes of death in these patients could not be directly attributed to the use of mechanical valves.
[TABULAR DATA NOT REPRODUCIBLE IN ASCII]
Overall morbidity was quite high (61%), mainly due to high rates of respiratory complications, postoperative atrial fibrillation, and reoperation for bleeding. Excluding uncomplicated episodes of atrial fibrillation overall, morbidity was still significant -- 35% (52/147). Postoperative CVA occurred in 4.8% (7/147). Three patients clearly had an intraoperative neurologic event. However, four patients were neurologically intact immediately after the operation, and the neurologic deficit developed 3 to 5 days after surgery. In all four patients, the development of CVA was strongly related to new-onset atrial fibrillation of [is greater than or equal to] 24-h duration. Of note are the very low rates of perioperative MI and mediastinal infection.
Most patients (138/147, 94%) required significant amount of homologous blood transfusions, an average of 22.3 [+ or -] 26 donors (median, 15 U; range, 0 to 134 U). Blood product utilization was high for each of the components: RBCs: 5.5 [+ or -6] U (median, 4 U; range, 0 to 34 U); fresh frozen plasma: 3.4 [+ or -] 4 U (median, 2 U; range, 0 to 22 U); platelets: 9.9 [+ or -] 11 U (median, 6 U; range, 0 to 59 U). Even after exclusion of the 15 patients (10%) who underwent reoperation for bleeding, 93% (123/132) required transfusion of an average of 16.3 [+ or -] 17 donors (median, 11 U; range, 0 to 78 U). The relatively high transfusion and complication rates resulted in an average of 37.8 [+ or -] 63 h (median, 20 h; range, 6 to 432 h) of ventilatory support, 3.9 [+ or -] 6.5 days (median, 2 days; range, 1 to 49 days) of ICU stay, and total hospital length of stay of 10.3 [+ or -] 7.3 days (median, 8 days; range, 5 to 52 days). These figures are significantly higher than our results following similar operations performed in younger patients (data not shown). Factors associated with increased early mortality in a univariate analysis (Table 3, top) included nonelective operations, increased cardiopulmonary and aortic cross-clamp times, use of intra-aortic balloon pump, increased postoperative mediastinal chest tube output, reoperation for bleeding, increased homologous transfusions, and postoperative CVA. However, in a multiple logistic regression analysis, only postoperative CVA and increased homologous transfusions were identified as independent predictors of increased mortality, and the use of bioprosthetic valve was associated math decreased mortality (Table 3, bottom). There was a trend toward increased mortality for mitral valve procedures compared to aortic valve, but the difference did not reach significance (MVR, 5/30 [16.6%] vs AVR 5/105 [4.8%], vs DVR 1/12 [9.1%], p=0.09). Performing CABG in addition to valve replacement did not significantly affect early mortality (valve procedure alone 4/74 [5.1%] vs valve procedure with CABG 7/69 [10.1%], p=0.15).
[TABULAR DATA NOT REPRODUCIBLE IN ASCII]
Long-term Mortality
Follow-up was complete for 98% (133/136) of hospital survivors and ranged from 2 to 55 months (mean, 30 [+ or -] 13 months). Fifteen patients (10.2%) died during the follow-up period. The most common cause of long-term mortality was congestive heart failure, 7 of 15 (46.6%). Actuarial survival at 55 months was 71 [+ or -] 6%, equivalent to a general age-, race-, and gender-matched population reported in the Life Tables of the US National Center for Health Statistics (Fig 1).[19] Factors associated math late mortality in a univariate analysis (Table 4, top) included advanced age, male gender, preoperative history of CVA, postoperative respiratory failure requiring ventilatory support [is greater than] 3 days and tracheostomy, postoperative CVA, and postoperative atrial fibrillation. In a multiple logistic regression analysis, advanced age, male gender, preoperative and postoperative CVA, and the need for tracheostomy remained significant independent predictors of long-term mortality (Table 4, bottom).
[TABULAR DATA NOT REPRODUCIBLE IN ASCII]
Quality of Life
Quality of life results are summarized in Figures 2-4. At the time of follow-up, 112 (96%) lived at home, 78% (91/116) defined their health status between good and excellent (Fig 2), and 81% (93/114) stated that the operation improved their health status (Fig 3). Ninety-seven percent (112/116) were able to bathe and dress independently, 92% (104/113) could walk at least one block, and 88.5% (100/113) could climb at least one flight of stairs. Moderate to vigorous activities could be performed by 59.2% (67/113) (Fig 4, A [top]). Most patients who could not perform vigorous activities were limited by concomitant disorders such as CVA, degenerative joint disease, and impaired visual acuity, rather than by their cardiovascular performance. Overall, at the time of follow-up, 81% (95/117) were in NYHA class I/II -- a significant change compared to preoperative status (Fig 4, B [bottom]).
[TABULAR DATA NOT REPRODUCIBLE IN ASCII]
DISCUSSION
Evaluation of the short- and long-term results of surgery in the elderly is difficult, since there is no true control group. A randomized trial comparing surgery to medical treatment would be ideal, but it is unlikely to be performed based on the existing data of the natural history of hemodynamically significant valvular heart disease treated medically.[20-22] Comparison to age-, race-, and gender-matched population of patients with the same cardiac abnormalities who were eligible for surge and refused is another theoretical option, but it would be difficult to perform. Comparison to younger patients carries significant limitations as older patients have different cardiac diseases, significantly more comorbidities, and usually are referred later for surgery.[20-22] The most common aortic valve abnormality in the elderly is senile calcific aortic stenosis, whereas young patients are frequently operated on for aortic regurgitation or a mixed lesion. Rheumatic and degenerative mitral valve disease are the most frequent indications for surgery in the young, whereas ischemic mitral regurgitation is much more common in the older age group.[20-22] Also, concomitant coronary artery disease with the need for myocardial revascularization is more common in the elderly.[21,22] These trends are reflected in our study group, where 90% of aortic valve replacements were performed in patients with calcific aortic stenosis, one third of mitral valve procedures were performed in patients with ischemic mitral regurgitation, and concomitant CABG was indicated in 47% of patients. The late referral is reflected by the advanced preoperative NYHA functional class (87% in class III/IV), and the fact that [is greater than] 50% of the operations were nonelective. Considering this very high-risk profile, the observed 7.5% operative mortality seems to be acceptable, and compares favorably with the reported mortality rates in the most recent Society of Thoracic Surgeons national database[23] and previous studies evaluating valve surgery in the elderly, with reported mortality rates of 9 to 37%.[4-17] Most likely, the lower mortality is a result of continued improvement in anesthesia, surgical techniques, and perioperative care, but also of patient selection. All the patients operated on during the study period were included in our analysis with no exclusion. However, data were not available on patients who had significant valvular disease but have not been referred for surgery by their primary care physicians and/or cardiologist, or have been rejected by the surgeon. The issue of selection bias is one of the major limitations of a retrospective study.
Elderly patients had prolonged ventilatory support and longer ICU and total hospital lengths of stay. These figures reflect not only the high risk of this specific group, but also our practice during the study period. Since than, early extubation and a "fast track" protocol have been aggressively implemented in all of our patients, resulting in a significant reduction of ventilatory support time and lengths of ICU and hospital stays. Similar to previous reports,[6,10,11] mortality following mitral valve surgery was higher compared to aortic valve surgery. This did not reach significance in our study, most likely due to a small sample size. Also, concomitant CABG was not associated with increased mortality, an issue that is still debatable in the literature.[4,11-17,23-25] The only independent predictors of early mortality in this series were increased homologous blood transfusions and postoperative CVA. The rate of reoperation for bleeding was relatively high.[23] However, even after exclusion of this subset of patients, blood transfusions were required in [is greater than] 90% of patients. Thus, the high transfusion rates in this age group may be related to other factors such as higher incidence of preoperative anemia, high percentage of women with small body surface area, and higher incidence of postoperative coagulopathy. In the latter part of the study, we switched to heparin-bonded CPB circuits with lower systemic anticoagulation protocol with a dramatic reduction of the rate of bleeding and blood product utilization.[26] Postoperative CVA occurred in 4.8% of our patients, which is somewhat lower than that previously reported in this age population.[4-17] In our study, postoperative CVA was related to new-onset atrial fibrillation in two thirds of the patients. Undoubtedly, efforts aimed at decreasing the incidence of postoperative atrial fibrillation are of prime importance. We have shown previously that strategies such as the use of heparin-bonded circuits effectively reduced the rate of atrial fibrillation in patients undergoing CABG.[27] Similar approaches should be studied in this patient population. In this study, the use of bioprostheses was associated with lower early mortality, although the reason is not entirely clear. The superior short- and long-term results with bioprosthetic valves in this age population have been documented previously.[28,29] Analyzing the effect of the type of prosthesis on long-term result was impossible in our study due to small number of patients with mechanical valves.
A major finding in this study was that patients who left the hospital had excellent long-term survival, similar to that of an age-, gender-, and race-matched US general population. Of note is that postoperative CVA was the only variable identified as a significant predictor of both early and late mortality. Although occurring in only 4.8%, when it does occur, it is a bad prognostic indicator.
Since the long-term survival of these patients is excellent, the issue of quality of life becomes an increasingly important aspect of the evaluation of the risk-benefit ratio and cost-effectiveness. Previous studies evaluating long-term results of valve surgery in the elderly have used survival and NYHA classification as the major end points and have reported improving results.[4-17,24,25] However, other measures such as placement of the patient, health self-perception, and other important components of overall quality of life assessment have not been investigated previously in this specific patient population.
Assessment of quality, of life is a complex process because it relies heavily on subjective data, it requires evaluation of many variables, and it is very difficult to quantify.[3] Comprehensive health surveys such as the McMaster Health Index Questionnaire,[30] the Sickness Impact Profile,[31] and others are lengthy instruments that make them clinically impractical. Single-item measures such as the National Health and Nutrition Examination Survey[32] are short and result in an improved response rate but are usually less precise, less reliable, and less valid. The Duke University MOS system,[33] which was developed as a compromise between these extremes, subsequently has become a very effective tool in evaluating quality of life in a variety of clinical trials.[34-36] In this study, we used a modified version of the MOS system because of the specific characteristics of the study group, being aware of the lower compliance rate for these type of studies in the elderly.[33] The focus was on functional capacity, the patient's perception of well-being, and the impact of surgery on overall health status. Bodily pain was not assessed as most patients were far out from surgery. Work status was believed to be not applicable as the patients were all retired. The psychosocial status was not included as it is a more complex issue, and we believed that it should be assessed separately. Using this short version, we were able to achieve a very high response rate and obtain a reliable evaluation of long-term quality of life of this patient population. The overall results were very encouraging. Most patients stated that the operation had a significant positive impact on their overall health status, and estimated their health status at the time of follow-up to be between good to excellent. Also, the vast majority of patients lived at home, either alone or with family, and were functionally independent. Most patients were able to function at a relatively high level. Those who did not were limited by other comorbidities and not by their cardiovascular performance.
In conclusion, valve surgery in the elderly is associated with acceptable early morbidity and mortality. Hospital survivors are expected to have a fife expectancy that is equal to that of age-, race-, and gender-matched population. Long-term quality of life in the elderly after valve surgery is excellent. These facts strongly support the performance of valve surgery in patients older than 75 years.
References
[1] US Bureau of the Census. Statistical abstract of the United States: 1994, 109th ed. Washington, DC: US Bureau of the Census, 1994
[2] US Bureau of the Census. Major improvement in life expectancy: 1989. Statistical bulletin, July-September 1990. Washington, DC: US Bureau of the Census, 1990
[3] Stewart AL, Ware JE. Measuring functioning and well being -- the Medical Outcomes Study approach. 1st ed. Durham, NC: Duke University, 1992; 1-449
[4] Tsai TP, Matloff JM, Chaux A, et al. Combined valve and coronary artery bypass procedures in septuagenarians and octogenarians: results in 120 patients. Ann Thorac Surg 1986; 42:681-84
[5] Bessone LN, Pupello, DF, Hiro SP, et al. Surgical management of aortic valve disease in the elderly: a longitudinal analysis. Ann Thorac Surg 1988; 46:264-69
[6] Fremes SE, Goldman BS, Ivanov J, et al. Valvular surgery in the elderly. Circulation 1989; 80(suppl I):I-77-I-90
[7] Fiore AC, Naunheim KS, Barner HB, et al. Valve replacement in octogenarians. Ann Thorac Surg 1989; 48:104-08
[8] Merrill WH, Stewart JR, Frist WH, et al. Cardiac surgery in patients age 80 years or older. Ann Surg 1990; 211:772-75
[9] Pifarre R. Open heart operations in the elderly: changing risk parameters. Ann Thorac Surg 1993; 56(suppl):S-71-S-73
[10] Davis EA, Gardner TJ, Gillinov AM, et al. Valvular disease in the elderly: influence on surgical results. Ann Thorac Surg 1993; 55:333-38
[11] Tsai TP, Chaux A, Matloff JM, et al. Ten-year experience of cardiac surge in patients aged 80 years and over. Ann Thorac Surg 1994; 58:445-51
[12] Adkins MS, Amalfitano D, Harnum NA, et al. Efficacy of combined coronary revascularization and valve procedures in octogenarians. Chest 1995; 108:927-31
[13] Kumar P, Zehr KJ, Chang A, et al. Quality of life in octogenarians after open heart surgery. Chest 1995; 108: 919-26
[14] He GW, Grunkemeier GL, Starr A. Aortic valve replacement in elderly patients: influence of concomitant coronary grafting on late survival. Ann Thorac Surg 1996; 61:1746-51
[15] Chocron S, Etievent JP, Clement F, et al. Is surgery, for aortic stenosis justified in patients over 75 years of age? J Cardiovasc Surg 1996; 37:255-59
[16] Wixon CL, Lust RM, Meadows LW, et al. Mitral valve surgery in the elderly [abstract]. Chest 1996; 110(suppl):62S
[17] Geholt A, Mullany CJ, Ilstrup D, et al. Aortic valve replacement in patients aged 80 years and older: early and long-term results. J Thorac Cardiovasc Surg 1996; 111:1026-36
[18] The Society of Thoracic Surgeons National Cardiac Surgery Database. Manual for data managers -- definitions of terms. Minneapolis: Summit Medical Systems, 1995
[19] Vital Statistics of the United States, 1992. Life-tables (volume II, section 6). Hyattsville, Md: US Dept of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Center for Health Statistics, 1996
[20] Braunwald E. valvular heart disease. In: Braunwald E, ed. Heart disease: a textbook of cardiovascular medicine. Philadelphia: WB Saunders, 1997; 1007-76
[21] Kirklin JW, Barratt-Boyes BG. Mitral valve disease with or without tricuspid valve disease. In: Kirklin JW, Barratt-Boyes BG, eds. Cardiac surgery. New York: Churchill Livingstone, 1993; 425-89
[22] Kirklin JW, Barratt-Boyes BG. Aortic valve disease. In: Kirklin JW, Barratt-Boyes BG, eds. Cardiac surgery. New York: Churchill Livingstone, 1993; 491-571
[23] Society of Thoracic Surgeons. Data analysis of the STS national cardiac surgery database: the sixth year. Chicago: Society of Thoracic Surgeons, 1997; 94-167
[24] Flameng WJ, Herijgers P, Scecsi J, et al. Determinants of early and late results of combined valve operations and coronary artery bypass grafting. Ann Thorac Surg 1996; 61:621-28
[25] Verheul HA, van den Brink RB, Bouma BJ, et al. Analysis of risk factors for excess mortality after aortic valve replacement. J Am Coll Cardiol 1995; 26:1280-86
[26] Shapira OM, Alda GS, Zelingher J, et al. Enhanced blood conservation and improved clinical outcome after valve surgery using heparin-bonded cardiopulmonary, bypass circuits. J Cardiac Surg 1996; 11:307-17
[27] Aldea GS, Doursounian M, O'Gara P, et al. Heparin-bonded circuits with a reduced anticoagulation protocol in primary CABG: a prospective randomized study. Ann Thorac Surg 1996; 62:410-18
[28] Borkon AM, Soule LM, Baughman KL, et al. Aortic valve replacement in the elderly patient. Ann Thorac Surg 1988; 46:270-77
[29] Jamieson WRE, Burr LH, Munro Al, et al. Cardiac valve replacement in the elderly: clinical performance of biological prostheses. Ann Thorac Surg 1989; 48:173-85
[30] Chambers LW, MacDonald LA, Tugwell P, et al. The McMaster Health Index Questionnaire as a measure of quality of life for patients with rheumatoid disease. J Rheumatol 1982; 9:780-84
[31] Bergner M, Bobbitt RA, Carter WB, et al. The Sickness Impact Profile: development and final revision of a health status measure. Med Care 1981; 19:787-805
[32] Wan T17. Livieratos B. Interpreting a general index of subjective well-being. Milbank Mem Fund Q Health Soc 1978; 56:531-56
[33] Stewart AL, Hays RD, Ware JE. The MOS short-form health survey: reliability and validity in patient population. Med Care 1988; 26:724-35
[34] Lavie CJ, Milani RV. Effects of cardiac rehabilitation and exercise training programs in patients [is greater than or equal to] 75 years of age. Am J Cardiol 1996: 78:675-77
[35] Bubien RS, Knotts-Dolson SM, Plumb VJ. Effect of radio-frequency catheter ablation on health-related quality of life and activities of daily living in patients with recurrent arrhythmias. Circulation 1996; 94:1585-91
[36] Hlatky MA. Rogers WJ, Johnstone I, et al. Medical care costs and quality of life after randomization to coronary angioplasty or coronary bypass surgery. N Engl J Med 1997; 336:92-99
COPYRIGHT 1997 American College of Chest Physicians
COPYRIGHT 2004 Gale Group