[[alpha].sub.2]-Antiplasmin deficiency is a serious coagulation disorder that results in unrestrained fibrinolytic activity. Clinically, it is manifested by instability of the fibrin hemostatic plug and prolonged or delayed bleeding, which is more serious in patients who are homozygous for this trait. A patient scheduled for aortic valve replacement and coronary bypass presented with a history of repeated episodes of postoperative bleeding. Hemostatic laboratory evaluation revealed that the patient had the heterozygous form of [[alpha].sub.2]-antiplasmin deficiency with a serum concentration of 52 percent (normal, >65 percent of the activity of pooled plasma). He underwent preoperative plasmapheresis with administration of 3,000 ml of fresh frozen plasma, which resulted in an increase in the preoperative level of [[alpha].sub.2]-antiplasmin to 78 percent. Although postoperative blood loss was greater than normal, it was easily managed. Preoperative identification of this rare coagulation abnormality permitted appropriate treatment and probably prevented a postoperative death from hemorrhage.
We recently treated a patient with unstable angina, severe aortic stenosis and coronary artery disease in whom preoperative evaluation led to the discovery of a striking history of previous bleeding episodes. Operation was postponed, and further laboratory studies revealed heterozygous [[alpha].sub.2]-antiplasmin deficiency. Managemetn of this patient and a brief review of the syndrome of [[alpha].sub.2]-antiplasmin deficiency are described. To our knowledge, this is the first reported case of a patient with this syndrome who has successfully undergone open-heart surgery. The patient is also notable for the degree of bleeding complications he had experienced throughout his life despite the fact that he has only the heterozygous form of the disease.
CASE REPORT
A 75-year-old white man presented with a long history of aortic insufficiency and the recent development of disabling dyspnea on exertion and angina. Cardiac catheterization revealed severe aortic insufficiency and tight stenosis of the left anterior descending coronary artery.
During preoperative evaluation, a history of repeated episodes of postoperative bleeding over a 20-year period was obtained from the patient. These episodes included postoperative hemorrhage after both transurethral prostatectomy and Nissen foundoplication, a large subcutaneous hematoma after repair of a ventral hernia, and a massive palmar hematoma after suture of a hand laceration.
The patient could recall no bleeding disorders in his parents or siblings, and he had no children. Hemostatic laboratory evaluation revealed a prothrombin time of 13.1 s, a partial thromboplastin time of 29 s, a normal bleeding time of eight minutes, and a platelet count of 98,000/cu mm. Bone marrow examination showed a slight increase in megakaryocytes consistent with mild idiopathic thrombocytopenic purpura, which was thought to be an unlikely cause of delayed postoperative hemorrhage. The thrombin time and reptilase time were normal, and no abnormal platelet antibodies were found. Because some of the patient's bleeding complications had occurred after an interval of apparently effective hemostasis, the possibility of clot instability was raised. The level of fibrin-stabilizing factor (factor XIII) was determined to be normal; however, the level of [[alpha].sub.2]-antiplasmin obtained was 52 percent of the activity of normal pooled plasma as determined by the method of Teger-Nilsson et al[1] (normal >65 percent).
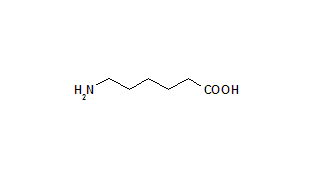
Because of the urgent need for cardiac surgery to control unstable angina, a plan was formulated in an attempt to prevent uncontrollable postoperative bleeding. Although the antifibrinolytic agents [apallon]-aminocaproic acid (Amicar) or tranexamic acid (Cyklokapron) could be used in the postoperative period, we considered it prudent to attempt to correct the patient's diminished level of [alpha.sub.2]-antiplasmin before operation.
The day before surgery, the patient underwent plasmapheresis, during which 3,080 ml of blood was removed and 3,000 ml of fresh frozen plasma, autologous red cells, and anticoagulant citrate dextrose solution was reinfused.
The next day, the patient underwent replacement of the aortic valve with a 23-mm Carpentier-Edwards bioprosthesis (Baxter Healthcare Corporation, Edwards CVS Division, Santa Ana, CA), and a vein graft was performed from the aorta to the left anterior descending coronary artery. The level of [alpha.sub.2]-antiplasmin drawn on the day of operation was 78 percent of control. Hemodynamically, the patient was stable after operation, but he did experience more than the usual amount of bleeding. Within the first 16 h after surgery, the patient had lost 2,270 ml of blood. For reasons that will be discussed later, the use of desmopressin acetate was avoided, and fresh frozen plasma, packed red cells, platelets and autologous blood were used for replacement of blood volume. During the next 24 h, output from the patient's chest tube was 495 ml, which dropped to 340 ml/24 h by the third postoperative day. Subsequently, the patient had minimal drainage from the mediastinal chest tubes, and they were removed. One year has passed since surgery, and the patient is doing well.
DISCUSSION
The formation and dissolution of fibrin clot is a dynamic process that should result in a temporary hemostatic plug until healing of the primary vessel can occur. Activation of plasminogen and dissolution of this fibrin clot can be initiated by a number of intrinsic and extrinsic mechanisms.[2] To modulate and restrain this fibrinolytic activity, normal blood contains a number of inhibitory agents, the most important of which is [alpha.sub.2]-antiplasmin.[2-5] This glycoprotein modulates fibrinolysis, resulting in a more stable clot.[6-8]
The clinical syndrome of [[alpha].sub.2]-antiplasmin defiency was first reported by Aoki et al[9] in 1979. This syndrome has been reported in two Japanese families,[9,10] a Dutch family[11] and an elderly Dutch man,[12] an American family,[13] and a Norwegian family.[14] Abnormal and functionally deficient [[alpha].sub.2]-antiplasmin resulting from molecular substitution of alanine also has been described[15] in two sisters in the Netherlands.
The typical form of [[alpha].sub.2]-antiplasmin deficiency is transmitted as a non-sex-linked autosomal recessive trait. Although the family pedigree in two of these reports[9,13] revealed consanguinity, the absence of consanguinity in the other reported cases suggests that the genetic trait may be distributed more widely.
Patients with [[alpha].sub.2]-antisplamin deficiency who are homozygous have only 1 to 10 percent normal activity as measured by a variety of functional and immunochemical assays.[9-11,13,16] These patients have a severe clinical bleeding abnormality, including neonatal umbilical hemorrhage, prolonged bleeding after lacerations or contusions, gingival bleeding, hemoarthroses, subarachnoid and epidural hemorrhage, muscle hematomas, hemothorax, hematuria and heavy menstrual bleeding.
Patients with [[alpha].sub.2]-antiplasmin deficiency who are heterozygous have approximately 50 percent of the normal level of [[alpha].sub.2]-antiplasmin in the plasma.[9-11,13] Although the heterozygous patients in the Japanese family first described[9] were asymptomatic, approximately 40 percent of heterozygous patients in two other series[11,13] have experienced mild hemorrhagic complications. Our patient, although heterozygous, had experienced multiple significant bleeding complications in the past. The clinical expression of the disease in heterozygous patients may relate to the degree of challenge presented to the clotting and fibrinolytic systems.
Results of routine preoperative coagulation studies are normal, and these studies are of no value in screening for this rare syndrome. A careful history of previous bleeding problems must be elicited and pursued. Suspected abnormalities of clot stability and fibrinolysis should be investigated by determination of clot lysis time, level of factor XIII and level of [[alpha].sub.2]-antiplasmin.[9,13,16,17]
No patient with [[alpha].sub.2]-antiplasmin deficiency has previously been reported to have undergone open-heart surgery. The implications of this condition in such patients are potentially life-threatening. Secondary fibrinolysis is a common result of extracorporeal circulation, and the addition of hereditary [[alpha].sub.2]-antiplasmin deficiency might result in disastrous or fatal hemorrhage from the extensive raw surfaces and vascular suture lines.
Both tranexamic acid and [apallon]-aminocaproic acid have been used to treat patients with this syndrome who had bleeding or who were undergoing noncardiac operations. However, the ability of these agents to control the additive hyperfibrinolytic challenges of [[alpha].sub.2]-antiplasmin and the postextracorporeal circulation state is unknown. Furthermore, intravascular thrombosis of the saphenous vein graft or prosthetic aortic valve is an unlikely but worrisome potential compliation of antifibrinolytic agents.
We decided to attempt to correct this [[alpha].sub.2]-antiplasmin deficiency preoperatively using fresh frozen plasma, and we used concomitant plasmapheresis to prevent intravascular volume overload. Plasma exchange raised the level of [[alpha].sub.2]-antiplasmin in our patient to 78 percent on the day of operation, which is within the normal range. Fresh frozen plasma was used for volume replacement in the days immediately after operation to counteract the expected decline in concentration of transfused [[alpha].sub.2]-antiplasmin over the next one to three days.[10,18]
Despite pretreatment, our patient experienced more postoperative bleeding than usual, emphasizing the serious pathophysiology of even the heterozygous form under certain circumstances. Had life-threatening bleeding occurred despite our use of fresh frozen plasma, we would have administered [apallon]-aminocaproic acid or tranexamic acid. Given the extensive use of blood products ultimately required in our patient, it is possible that the risk of intravascular thrombosis from the use of such agents would have been less than that of transfusion-related disease. The risk-benefit ratio for these two treatments, which are complementary and certainly not mutually exclusive, must be determined for each patient. Desmopressin acetate, which has been advocated to enhance platelet activity in patients with excessive postoperative bleeding,[19] must be avoided in patients with [[alpha].sub.2]-antiplasmin deficiency because it may induce endothelial secretion of plasminogen activator.[20-22]
REFERENCES
[1] Teger-Nilsson AC, Friberger P, Gyzander E. Determination of a new rapid plasmin inhibitor in human blood by means of a plasmin specific tripeptide substrate. Scand J Clin Lab Invest 1977; 37:403-09
[2] Aoki N, Harpel PC. Inhibitors of the fibrinolytic enzyme system. Semin Thromb Hemost 1984; 10:24-41
[3] Aoki N, Kaulla KN von. Inactivation of human serum plasminogen antiactivator by synthetic fibrinolysis inducers. Thromb Diath Haemorrh 1969; 22:251-62
[4] Moroi M, Aoki N. Isolation and characterization of alpha 2-plasmin inhibitor from human plasma: a novel proteinase inhibitor which inhibits activator-induced clot lysis. J Biol Chem 1976; 251:5956-65
[5] Collen D. Identification and some properties of a new fast-reacting plasmin inhibitor in human plasma. Eur J Biochem 1976; 69:209-16
[6] Harpel PC. Blood proteolytic enzyme inhibitors: their role in modulating blood coagulation and fibrinolytic enzyme pathways. In: Colman RW, Hirsch J, Marder VJ, Salzman EW, eds. Hemostasis and thrombosis: basic principles and clinical practice. 2nd ed. Philadelphia: JB Lippincott, 1988:219-34
[7] Mimuro J, Kimura S, Aoki N. Release of alpha 2-plasmin inhibitor from plasma fibrin clots by activated coagulation factor XIII: its effect on fibrinolysis. J Clin Invest 1986; 77:1006-13
[8] Sakata Y, Aoki N. Significance of cross-linking of alpha 2-plasmin inhibitor to fibrin in inhibition of fibrinolysis and in hemostasis. J Clin Invest 1982; 69:536-42
[9] Aoki N, Saito H, Kamiya T, Koie K, Sakata Y, Kobakura M. Congenital deficiency of alpha 2-plasmin inhibitor associated with severe hemorrhagic tendency. J Clin Invest 1979; 63:877-84
[10] Yoshioka A, Kamitsuji T, Takase T, Iida Y, Tsukada S, Mikami S, et al. Congenital deficiency of alpha 2-plasmin inhibitor in three sisters. Haemostasis 1982; 11:176-84
[11] Kluft C, Vellenga E, Brommer EJ, Wijngaards G. A familial hemorrhagic diathesis in a Dutch family: an inherited deficiency of alpha 2-antiplasmin. Blood 1982; 59:1169-80
[12] Knot EA, ten Cate JW, Lamping RJ, Gie LK. Alpha 2-antiplasmin: functional characterization and metabolism in a heterozygote deficient patient. Thromb Haemost 1986; 55:375-78
[13] Miles LA, Plow EF, Donnelly KJ, Hougie C, Griffin JH. A bleeding disorder due to deficiency of alpha 2-antiplasmin. Blood 1982; 59:1246-51
[14] Stormorken H, Gogstad GO, Brosstad F. Hereditary alpha 2-antiplasmin deficiency. Thromb Res 1983; 31:647-51
[15] Holmes WE, Lijnen HR, Nelles L, Kluft C, Nieuwenhuis HK, Rijken DC, et al. Alpha 2-antiplasmin Enschede: alanine insertion and abolition of plasmin inhibitory activity. Science 1987; 238:209-11
[16] Aoki N. Genetic abnormalities of the fibrinolytic system. Semin Thromb Hemost 1984; 10:42-50
[17] Rapaport SI. Preoperative hemostatic evaluation: which tests, if any? Blood 1983; 61:229-31
[18] Tamaki T, Sakata Y, Aoki N. Survival of transfused alpha 2-plasmin inhibitor in a patient with its congenital deficiency. Thromb Res 1981; 22:281-86
[19] Salzman EW, Weinstein MJ, Weintraub RM, Ware JA, Thurer RL, Robertson L, et al. Treatment with desmopressin acetate to reduce blood loss after cardiac surgery: a double-blind randomized trial. N Engl J Med 1986; 314:1402-06
[20] Mannucci PM, Rota L. Plasminogen activator response after DDAVP: a clino-pharmacological study. Thromb Res 1980; 20:69-76
[21] Juhan-Vague I, Conte-Devolx B, Aillaud MF, Mendez C, Oliver C, Collen D. Effects of DDAVP and venous occlusion on the release of tissue-type plasminogen activator and von Willebrand factor in patients with panhypopituitarism. Thromb Res 1984; 33:653-59
[22] Desnoyers PC. Indirect fibrinolytic agents. In: Markwardt F, ed. Fibrinolytics and antifibrinolytics. New York: Springer-Verlag, 1978:273-314
COPYRIGHT 1990 American College of Chest Physicians
COPYRIGHT 2004 Gale Group