Edema is the result of an imbalance in the filtration system between the capillary and interstitial spaces. The kidneys play a key role in regulating extracellular fluid volume by adjusting sodium and water excretion. Major causes of edema include venous obstruction, increased capillary permeability, and increased plasma volume secondary to sodium and water retention. A systematic approach is warranted to determine the underlying diagnosis. Treatment includes sodium restriction, diuretic use, and appropriate management of the underlying disorder. Leg elevation may be helpful in some patients. Loop diuretics often are used alone or in combination. In patients with New York Heart Association class III and IV congestive heart failure, spironolactone has been found to reduce morbidity and mortality rates. In patients with cirrhosis, ascites is treated with paracentesis and spironolactone. Dihydropyridine-induced edema can be treated with an angiotensin-converting enzyme inhibitor or angiotensin-receptor blocker. Lymphedema occurs when a protein-rich fluid accumulates in the interstitium. Compression garments and range-of-motion exercises may be helpful in patients with this condition.
**********
Edema is a frequently encountered problem in clinical practice, but effective treatment of this condition is a relatively recent development. (1) The etiology of edema always must be determined; the condition may indicate an underlying life-threatening disease such as congestive heart failure, or it may be caused by something as benign as sitting for too long. Edema may be localized and confined to one limb, or generalized and massive. It usually results from an imbalance of forces controlling fluid exchange, including an alteration in capillary hemodynamics favoring the retention of sodium and water by the kidneys and the movement of fluid from the vascular space into the interstitium. (2) The causes of edema are categorized in Table 1. (3)
Pathophysiology
Edema occurs when forces such as an elevation in capillary hydraulic pressure, an increase in capillary permeability or interstitial oncotic pressure, or a reduction in plasma oncotic pressure increase net filtration. (2) The kidneys have a central role in maintaining body fluid homeostasis: they control extracellular fluid volume by adjusting sodium and water excretion. Antidiuretic hormone, which is secreted in response to stimuli such as changes in blood volume, tonicity, and blood pressure, is the primary regulator of body water. Sodium and other anions form the major solutes in extracellular fluid and are maintained within a narrow range. Sodium chloride intake generally is equivalent to output over the course of a few days; when intake increases, there is a compensatory increase in sodium chloride excretion after a lag period. Thus, extracellular fluid volume can be maintained at a constant level despite wide fluctuations in intake. (4)
The concept of effective arterial blood volume (EABV) is central to an understanding of the sodium retention that occurs to maintain plasma volume. EABV is sensed by volume homeostatic mechanisms and ultimately modulates renal sodium reabsorption. EABV correlates with extracellular fluid volume. In healthy persons, sodium loading increases extracellular fluid volume and EABV, resulting in prompt natriuresis and restoration of normal volumes. In persons who are volume depleted, EABV and extracellular fluid volume are reduced. Renal sodium retention is activated via the renin-angiotensin-aldosterone axis, and normal blood volume is restored. When kidney function is impaired, the partitioning of fluid in various compartments is disturbed. In the ensuing edematous states, the reduction in EABV activates volume/pressure sensors, including low-pressure baroreceptors in the venous circulation, high-pressure baroreceptors in the great vessels, intrarenal receptors, and intrahepatic receptors.
In patients with primary sodium retention, the afferent stimuli are suppressed. As extracellular volume increases, edema develops and EABV decreases. This change stimulates efferent pathways, causing sodium retention, activation of the sympathetic nervous system, stimulation of the renin-angiotensin-aldosterone axis, and secretion of arginine vasopressin.
Whether it is caused by decreased cardiac output or other conditions, edema persists because of compensatory mechanisms geared toward maintaining plasma volume.
Treatment
PRINCIPLES OF THERAPY
Treatment of edema consists of reversing the underlying disorder (if possible), restricting dietary sodium to minimize fluid retention, and, usually, employing diuretic therapy. (3) This approach highlights the need to establish a diagnosis and to use nonpharmacologic approaches when appropriate, rather than resorting to the immediate use of diuretics.
Not all patients with edema will require drug treatment; in some patients, sufficient sodium restriction (i.e., less than the amount excreted by the kidneys) and elevation of the lower extremities above the level of the left atrium are effective. However, diuretics are required in most patients in addition to nonpharmacologic treatments, especially continued restriction of salt. The choice of diuretic, route of administration, and dosing regimen will vary based on the underlying disease, its severity, and the urgency of the problem. Knowledge of the pharmacokinetics and pharmacodynamics of the various agents is essential.
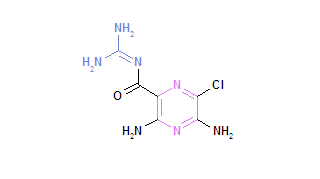
Diuretics exert their effects at different sites in the kidneys (Table 2). (4) Loop diuretics such as furosemide (Lasix), bumetanide (Bumex), and torsemide (Demadex) block the sodium-potassium chloride transporter in the ascending loop of Henle, (5) whereas thiazide diuretics block the electroneutral sodium chloride transporter in the distal convoluted tubule. Amiloride (Midamor) and triamterene (Dyrenium) block apical sodium channels in the cortical collecting tubule. These drugs are highly bound to albumin. (4) All diuretics except spironolactone (Aldactone) reach luminal sites of action through the tubular fluid.
After oral administration of furosemide, absorption averages about 50 percent, but may range from 10 to 80 percent. Absorption of bumetanide and torsemide is more complete, ranging from 80 to 100 percent. (6) Thiazide diuretics, such as chlorothiazide (Diuril) and hydrochlorothiazide (Esidrix), may be excreted unchanged in the urine. Other agents, such as bendroflumethiazide (Naturetin) and indapamide (Lozol), are metabolized by the liver. Plasma half-life will determine the frequency of administration. Thiazide diuretics with a long half-life can be administered once or twice daily.
Loop diuretics with shorter half-lives, which range from approximately one hour for bumetanide to three to four hours for torsemide, must be given more frequently than thiazide diuretics. (6) The effect of loop diuretics dissipates rapidly, after which the kidneys immediately begin to reabsorb sodium and nullify the diuretic effect. This process is called post-diuretic sodium chloride retention. If sodium chloride intake is high and the half-life of the diuretic is short (as with a loop diuretic), post-diuretic sodium chloride retention compensates entirely for the sodium loss.7 Therefore, sodium restriction is important when a patient is taking loop diuretics.
TREATMENT FAILURE
Diuretic resistance is a failure to create a negative sodium balance despite the use of high dosages of diuretics (e.g., furosemide at a dosage of 240 mg per day). Resistance should be suspected in patients with persistent edema who are receiving appropriate diuretic treatment and restricting physical activity and sodium intake (i.e., less than 2 g per day). (8)
An understanding of the pharmacokinetics of the various diuretic agents is essential in addressing diuretic resistance. Furosemide administered orally has an erratic absorption pattern; bumetanide may be a better choice because it is absorbed more completely. Adding a diuretic that acts at a different site may help overcome the adaptation of distal convoluted cells to chronic diuretic use. Using short-acting diuretics more frequently or using longer-acting diuretics limits the sodium reabsorption that can occur when the diuretic effect wears off. The patient must be followed carefully for adverse effects such as hypokalemia and hypovolemia. Occasionally it may be necessary to use a continuous intravenous infusion of a loop diuretic. This strategy should be reserved for patients with true refractory resistance who are being treated in an intensive care unit.9
Other potential causes of treatment failure are listed in Table 3. (8) The problem may not be true drug resistance, but a matter of nonadherence to therapy; this becomes a concern in treating older adults who are taking multiple medications and are at risk for urinary incontinence. These patients may limit diuretic use to maintain continence. Diuretic resistance can be aggravated by the concomitant use of nonsteroidal anti-inflammatory drugs (NSAIDs), which may negate the diuretic effect.10 Discontinuing NSAID therapy may correct the resistance.
Another potential cause of treatment failure is diuretic tolerance. Short-term tolerance should be considered when there is a decrease in response after the first dose of a diuretic has been taken. Short-term tolerance is thought to be caused by depletion of intravascular volume, with a compensatory response to protect against further fluid loss. Long-term tolerance can occur in patients who are treated with loop diuretics over a long period. The problem is related to a mechanism whereby the distal nephron segments undergo hypertrophy and reabsorb more sodium after prolonged exposure to solutes, thus decreasing overall diuresis. (11) Increasing the dosage of loop diuretics in patients with long-term diuretic tolerance is unlikely to improve diuresis, whereas adding a thiazide diuretic, which acts at a different site, results in a synergistic and brisk diuretic response. The addition of acetazolamide (Diamox), which acts on the proximal tubule, also can be effective when there is decreasing response to other diuretics. (12)
CONGESTIVE HEART FAILURE
In patients with moderate to severe congestive heart failure, activation of the renin-angiotensin system results in vasoconstriction in the afferent and efferent renal arterioles. Neurohumoral responses include the release of aldosterone from the adrenal glands; increased sympathetic activity, which causes increased sodium reabsorption in the proximal tubules; and secretion of antidiuretic hormone, which causes increased water reabsorption in the collecting ducts and results in hyponatremia. (13)
The goals of treatment include symptom relief, improved quality of life, retardation of disease progression, and decreased mortality. (14) Despite their widespread use, diuretics have not been shown to improve survival in patients with congestive heart failure; the exception is spironolactone, which in one study (15) decreased morbidity and mortality rates in patients with New York Heart Association class III and IV heart failure. Diuretics have been used in combination with other agents in all of the other major survival heart failure trials (16) and provide superior symptom relief. Before inducing an increase in urinary output, loop diuretics administered intravenously reduce pulmonary capillary wedge pressure and increase venous capacitance within a few minutes of administration. (17) Loop diuretics are effective as solo agents in the treatment of moderate to severe heart failure. Most patients with heart failure have some degree of renal impairment secondary to intrinsic disease, prerenal azotemia, or an age-related decline in renal function. To overcome competition from endogenic organic ions at tubular binding sites, loop diuretics typically must be administered at higher dosages in patients with heart failure.
CIRRHOSIS
Most of the principles of diuretic use and sodium restriction apply in the treatment of ascites and edema associated with cirrhosis. Ascites is a common complication of cirrhosis and is associated with a worse prognosis. (18) Its severity typically is graded on a scale of 1 to 3: grade 1, or mild ascites, is detectable only by ultrasound examination; grade 2 ascites is manifested by moderate symmetrical distension of the abdomen; and grade 3, or gross ascites, is characterized by marked abdominal distension. Ascitic fluid should be sampled to determine the cause. Restriction of sodium and water is recommended almost universally.
Grades 2 and 3 ascites occurring in patients with cirrhosis typically require the addition of spironolactone to combat hyperaldosteronism (18); a typical dosage of 100 to 200 mg given once per day with food generally is effective. Response should be monitored by daily weight measurement. Weight loss should be limited to 0.5 kg (1 lb, 2 oz) per day in patients without peripheral edema and to 1.0 kg (2 lb, 3 oz) per day in patients with edema. If no response occurs to treatment with 100 mg of spironolactone per day, a low-dose loop diuretic can be added. Precipitation of hepatorenal syndrome can occur with overly aggressive diuretic therapy. Side effects of spironolactone include hyperkalemia, metabolic acidosis, and gynecomastia; these effects typically respond to a lowering of the dosage or discontinuation of the drug.
Paracentesis is the treatment of choice in patients with grade 3 ascites and should be complemented by sodium restriction and diuretic therapy. (18) Large-volume paracentesis in a single procedure is recommended even if the volume of f luid removed exceeds 5 L. (19) Paracentesis should be followed by f luid replacement and expansion to prevent renal complications. (20) Volume expansion should include a synthetic plasma substitute or albumin, especially if more than 5 L of fluid is removed. (21) In patients with refractory ascites, the use of a transjugular intrahepatic portosystemic shunt (TIPS) may be considered. In a randomized study, (22) TIPS was superior to large-volume paracentesis in relieving ascites and prolonging survival (58 versus 32 percent of patients were alive at two years). Many patients with ascites and cirrhosis eventually become candidates for hepatic transplantation. In another randomized study (23) comparing TIPS with paracentesis and albumin, replacement resulted in greater survival rates at two years without transplantation (59 versus 29 percent).
NEPHROTIC SYNDROME
Nephrotic syndrome is a less common cause of edema and is characterized by marked proteinuria, hypoalbuminemia, hyperlipidemia, and edema. Debate continues over whether the edema is a result of decreased oncotic pressure or overfilling with sodium that results in water retention; most researchers now subscribe to the overfilling theory. (24) Treatment includes sodium restriction and a combination of loop diuretics, antialdosterone drugs, (25) and other medications to treat the underlying disease process.
CHRONIC VENOUS INSUFFICIENCY
Venous insufficiency is a common cause of edema of the lower extremities. New-onset edema--especially if it is unilateral--necessitates the exclusion of deep venous thrombosis (DVT). Complications of long-standing lower-extremity edema include stasis dermatitis, ulceration, and cellulitis. Diuretics have limited benefit. Elevation of the affected limb above the level of the heart and the use of support stockings can alleviate venous hypertension and reduce edema, (26) and support stockings have been found to significantly reduce the incidence of edema and DVT on long-distance flights (i.e., longer than seven hours). (27)
MEDICATION-INDUCED EDEMA
Many medications have been implicated in pedal edema, especially vasodilators, estrogens, NSAIDs, and calcium channel blockers. Dihydropyridine drugs are more likely than other calcium channel blockers to cause pedal edema. The edema appears to be dose-dependent and increases over time. (28) Because medication-induced edema is caused by capillary hypertension, diuretics are not an effective treatment. However, angiotensin-converting enzyme inhibitors and angiotensin-receptor blockers seem to be effective. (29,30)
LYMPHEDEMA
Lymphedema is the general term for a group of pathologic conditions characterized by excessive regional interstitial accumulation of protein-rich f luid. (31) Lymphedema may be primary or secondary; globally, secondary lymphedema caused by filariasis is much more common, affecting 90 million persons worldwide. (31) Lymphedema following axillary node dissection is the most common type in the United States, (32) affecting up to 80 percent of patients after surgery.31 With the advent of breast-conserving surgery and sentinel lymph-node biopsy, it is hoped that the condition will occur less frequently.
Distinguishing lymphedema from other forms of edema may be challenging, especially early in its course. Stemmer's sign, the inability to tent the edematous skin on the dorsal surface of the toes, suggests lymphedema. Additional findings include swelling of the dorsum of the foot with a "squared-off " appearance of the digits. A computed tomography (CT) or magnetic resonance imaging (MRI) scan may be necessary to confirm the diagnosis. A characteristic honeycomb pattern in the subcutaneous compartment distinguishes lymphedema from other edemas; MRI is considered superior to CT in diagnosing patients with this finding. (33)
Treatment may be initiated if the circumference of the arm increases by 2 cm from the preoperative measurement. Long-term use of compression garments coupled with meticulous skin care and avoidance of blood-pressure measurements and other constrictions on the affected site are likely helpful. (34) The use of range-of-motion exercises; skin care; compression wrapping; and comprehensive decongestive physiotherapy, a two-phase process of specialized manual lymph massage and drainage, may be effective. Diuretics may be of benefit early in the course of the disease but rarely are effective on a long-term basis. Surgical treatment is of little benefit, although it may play a debulking role in patients with advanced elephantiasis. (35)
REFERENCES
(1.) Eknoyan G. A history of edema and its management. Kidney Int Suppl 1997;59:S118-26.
(2.) Rose BD. Pathophysiology and etiology of edema. In: Rose BD, ed. UpToDate. Wellesley, Mass.: UpToDate, 2004.
(3.) Rose BD. Approach to the adult with edema. In: Rose BD, ed. Up-To-Date. Wellesley, Mass.: UpToDate, 2004.
(4.) Ellison DH. Diuretic drugs and the treatment of edema: from clinic to bench and back again. Am J Kidney Dis 1994;23:623-43.
(5.) Wittner M, Di Stefano A, Wangemann P, Greger R. How do loop diuretics act? Drugs 1991;41(suppl 3):1-13.
(6.) Brater DC. Diuretic therapy. N Engl J Med 1998;339:387-95.
(7.) Wilcox CS, Mitch WE, Kelly RA, Skorecki K, Meyer TW, Friedman PA, et al. Response of the kidney to furosemide. I. Effects of salt intake and renal compensation. J Lab Clin Med 1983;102:450-8.
(8.) Dormans TP, Gerlag PG, Russel FG, Smits P. Combination diuretic therapy in severe congestive heart failure. Drugs 1998;55:165-72.
(9.) Dormans TP, van Meyel JJ, Gerlag PG, Tan Y, Russel FG, Smits P. Diuretic efficacy of high dose furosemide in severe heart failure: bolus injection versus continuous infusion. J Am Coll Cardiol 1996;28:376-82.
(10.) Furst DE. Clinically important interactions of nonsteroidal anti-inflammatory drugs with other medications. J Rheumatol Suppl 1988;17:58-62.
(11.) Kaissling B, Bachmann S, Kriz W. Structural adaptation of the distal convoluted tubule to prolonged furosemide treatment. Am J Physiol 1985;248(3 pt 2):F374-81.
(12.) Knauf H, Mutschler E. Sequential nephron blockade breaks resistance to diuretics in edematous states. J Cardiovasc Pharmacol 1997;29:367-72.
(13.) De Bruyne LK. Mechanisms and management of diuretic resistance in congestive heart failure. Postgrad Med J 2003;79:268-71.
(14.) Consensus recommendations for the management of chronic heart failure. On behalf of the membership of the advisory council to improve outcomes nationwide in heart failure. Am J Cardiol 1999;83(2A):1A-38A.
(15.) Pitt B, Zannad F, Remme WJ, Cody R, Castaigne A, Perez A, et al. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. Randomized Aldactone Evaluation Study Investigators. N Engl J Med 1999;341:709-17.
(16.) Packer M. Treatment of chronic heart failure. Lancet 1992;340:92-5.
(17.) Silke B. Haemodynamic impact of diuretic therapy in chronic heart failure. Cardiology 1994;84(suppl 2):115-23.
(18.) Moore KP, Wong F, Gines P, Bernardi M, Ochs A, Salerno F, et al. The management of ascites in cirrhosis: report on the consensus conference of the International Ascites Club. Hepatology 2003;38:258-66.
(19.) Tito L, Gines P, Arroyo V, Planas R, Panes J, Rimola A, et al. Total paracentesis associated with intravenous albumin management of patients with cirrhosis and ascites. Gastroenterology 1990;98:146-51.
(20.) Anand BS. Drug treatment of the complications of cirrhosis in the older adult. Drugs Aging 2001;18:575-85.
(21.) Gines P, Tito L, Arroyo V, Planas R, Panes J, Viver J, et al. Randomized comparative study of therapeutic paracentesis with and without intravenous albumin in cirrhosis. Gastroenterology 1988;94:1493-502.
(22.) Rossle M, Ochs A, Gulberg V, Siegerstetter V, Holl J, Deibert P, et al. A comparison of paracentesis and transjugular intrahepatic portosystemic shunting in patients with ascites. N Engl J Med 2000;342:1701-7.
(23.) Salerno F, Merli M, Riggio O, Cazzaniga M, Valeriano V, Pozzi M, et al. Randomized controlled study of TIPS versus paracentesis plus albumin in cirrhosis with severe ascites. Hepatology 2004;40:629-35.
(24.) Palmer BF, Alpern RJ. Pathogenesis of edema formation in the nephrotic syndrome. Kidney Int Suppl 1997;59:S21-7.
(25.) De Santo NG, Pollastro RM, Saviano C, Pascale C, Di Stasio V, Chiricone D, et al. Nephrotic edema. Semin Nephrol 2001;21:262-8.
(26.) Douglas WS, Simpson NB. Guidelines for the management of chronic venous leg ulceration. Report of a multidisciplinary workshop. British Association of Dermatologists and the Research Unit of the Royal College of Physicians. Br J Dermatol 1995;132:446-52.
(27.) Cesarone MR, Belcaro G, Errichi BM, Nicolaides AN, Geroulakos G, Ippolito E, et al. The LONFLIT4-Concorde Deep Venous Thrombosis and Edema Study: prevention with travel stockings. Angiology 2003;54: 143-54.
(28.) Messerli FH, Grossman E. Pedal edema-not all dihydropyridine calcium antagonists are created equal. Am J Hypertens 2002;15:1019-20.
(29.) Messerli FH, Oparil S, Feng Z. Comparison of efficacy and side effects of combination therapy of angiotensin-converting enzyme inhibitor (benazepril) with calcium antagonist (either nifedipine or amlodipine) versus high-dose calcium antagonist monotherapy for systemic hypertension. Am J Cardiol 2000;86:1182-7.
(30.) Pool J, Kaihlanen P, Lewis G, Ginsberg D, Oparil S, Glazer R, et al. Once-daily treatment of patients with hypertension: a placebo-controlled study of amlodipine and benazepril alone. J Hum Hypertens 2001;15: 495-8.
(31.) Rockson SG. Lymphedema. Am J Med 2001;110:288-95.
(32.) Segerstrom K, Bjerle P, Graffman S, Nystrom A. Factors that influence the incidence of brachial oedema after treatment of breast cancer. Scand J Plast Reconstr Surg Hand Surg 1992;26:223-7.
(33.) Topham EJ, Mortimer PS. Chronic lower limb oedema. Clin Med 2002;2:28-31.
(34.) Harris SR, Hugi MR, Olivotto IA, Levine M. Clinical practice guidelines for the care and treatment of breast cancer: 11. Lymphedema. CMAJ 2001;164:191-9.
(35.) Macdonald JM, Sims N, Mayrovitz HN. Lymphedema, lipedema, and the open wound: the role of compression therapy. Surg Clin North Am 2003;83:639-58.
JAMES G. O'BRIEN, M.D., is the Margaret D. Smock Endowed Chair in Geriatrics and professor and chair of the Department of Family and Geriatric Medicine at the University of Louisville (Ky.) School of Medicine. He also is director of the department's geriatrics division. Dr. O'Brien received his medical degree from University College Faculty of Medicine, Dublin, Ireland, and completed a family practice residency at Saginaw (Mich.) Cooperative Hospitals. He also completed a fellowship in geriatrics at Duke University School of Medicine, Durham, N.C.
SHOBHA A. CHENNUBHOTLA, M.D., is assistant professor of family and geriatric medicine at the University of Louisville School of Medicine. Dr. Chennubhotla received her medical degree from Gandhi Medical College, Osmania University, Hyderabad, India, and completed a family medicine residency and geriatric fellowship at the University of Louisville School of Medicine.
RAMANA V. CHENNUBHOTLA, M.D., is a staff member at the Veterans Affairs Medical Center in Louisville, Ky. Dr. Chennubhotla received his medical degree from Gandhi Medical College, Osmania University, and completed an internal medicine residency at State University of New York at Buffalo School of Medicine and Biomedical Sciences and a family practice residency at St. Francis Hospital, Evanston, Ill.
Address correspondence to James G. O'Brien, M.D., Department of Family and Geriatric Medicine, University of Louisville School of Medicine, MedCenter One, 501 E. Broadway, Suite 240, Louisville, KY 40202 (e-mail: jgobri01@gwise.louisville.edu). Reprints are not available from the authors.
The authors indicate that they do not have any conflicts of interest. Sources of funding: none reported.
Members of various family medicine departments develop articles for "Practical Therapeutics." This article is one in a series coordinated by the Department of Family and Geriatric Medicine at the University of Louisville School of Medicine, Louisville, Ky. Guest editor of the series is James G. O'Brien, M.D.
COPYRIGHT 2005 American Academy of Family Physicians
COPYRIGHT 2005 Gale Group