Nasal potential difference measurements are valuable endpoint assays in clinical studies of novel treatments for cystic fibrosis (CF). Similar measurements made on the lower airway via the bronchoscope have been successful in adults, but have not been reported in children, the group most likely to benefit from such therapies. Here we report the design and validation of a small, single-lumen catheter technique allowing baseline potential difference and chloride secretion to be assessed in the distal airways of children as young as 1 year of age. Tracheal baseline values were significantly higher in children with CF than those without, although this was not the case more distally. In airways between the third and seventh generation, perfusion with a zero chloride solution containing isoprenaline led to a significant change in potential difference in children without CF, whereas no change was seen in those with CF. This measure provided a reliable distinguishing test between the two disease groups. We confirm that invasive bronchoscopic techniques can be performed safely and reliably in small children. Potential difference measurements could form a useful functional endpoint assay for future studies of either the CFTR gene or protein-based therapies in future trials in the pediatric age group.
Keywords: cvstic fibrosis: ion transport: ootential difference
Cystic fibrosis (CF) results from abnormal function of the epithelial chloride ion channel, CF transmembrane conductance regulator (CFTR) (1), likely leading to low airway surface liquid volume and impairment of mucociliary clearance (2). Subsequent chronic infection results in an exaggerated and damaging inflammatory response (3). Despite increases in survival, the disease still carries significant morbidity, and death in early adulthood is common (4). This has led to the search for novel forms of treatment, either CFTR gene transfer (5) or improving endogenous CFTR protein function (6). Neither of these approaches is likely to reverse existing lung damage, so success is likely to be greatest in the earlier stages of disease (i.e., in young children). One of the difficulties with such therapeutic studies is in assessing efficacy; rates of decline in lung function or survival are not useful in early-phase studies, and surrogate endpoints are required.
CFTR-related ion transport can be measured electrically as the transepithelial potential difference (PD). Nasal measurements are well-established, characteristic features of CF epithelia, including higher (more negative) baseline readings; an exaggerated depolarization to sodium channel blocking drugs, such as amiloride; and a reduced or absent response to stimulation of chloride secretion (7, 8). Nasal PD measurements have proved useful as an aid to diagnosis (9,10) and in clinical studies of novel therapies (11-13). In gene therapy studies, these measurements can provide evidence of functional correction - in contrast to molecular assays for cDNA or mRNA, which do not. Many such studies were conducted initially in the nose because of ease of access and safety issues. However, it is likely that novel therapeutic agents will eventually need to prove effective in correcting the underlying defect in the target organ, namely the lower airways.
We recently reported bronchoscopic measurements of both baseline PD and responses to drug perfusion in the lower airway of adults (14). Similar to that observed in the nose, chloride secretion was significantly impaired in subjects with CF and was partially restored after a single dose of cationic liposome-CFTT? gene complex. To date, a similar technique has not been assessed in children. This age group poses specific problems, such as small airway size, length of time required for such procedures, and ethical issues. In designing this study, we were informed by previously unpublished bronchoscopic data obtained from adult subjects at our institution, which we present here for completeness and for the purposes of comparison. We describe the design and validation of a small, single-lumen catheter and a perfusion protocol, which allowed assessment of both baseline PD and chloride secretion in children as young as 1 year of age. Data included in this article have been previously published in abstract form (15).
METHODS
An expanded METHODS section is provided in the online supplement.
Assessment of the Single-Lumen Catheter using Nasal Measurements
The size limitations of the suction/biopsy channels of the pediatric flexible bronchoscopes (1.2-mm diameter in the 3.6-mm bronchoscope used in the majority of children younger than 6-7 years) led to the requirement for a smaller catheter than that used in our previous nasal (> 3 mm) and adult bronchoscopic studies (2.8 mm). Early attempts to develop a double-lumen catheter of a sufficiently small diameter were unsuccessful (see online supplement). We therefore assessed a polyethylene single-lumen catheter (1.0-mm outer diameter). The catheter was primed to the tip with a zero chloride solution containing isoproterenol (ZCI). Baseline recordings and responses to perfusion with this catheter were measured in the noses of adult volunteers (four without CF, five with CF). Subsequently, this technique was directly compared with the conventional, double-lumen nasal PD technique in a further six healthy volunteers, with measurements made in random order on separate days in the same nostril (for further details see the online supplement).
Potential Difference Measurement in the Pediatric Lower Airways
Children were undergoing a general anesthetic (GA) for either a fiberoptic bronchoscopy (patients with CF and patients without) or insertion of an in-dwelling central venous catheter (patients with CF). All children received a combination of inhaled and intravenous anesthetic agents; topical anesthesia with lignocaine has been shown to affect PD recordings and was avoided. Nonsurgical subjects were self-ventilating through cither face or laryngeal masks, whereas surgical subjects were endotracheally intubated and ventilated. Bronchoscopies were performed by one of two operators (J.C.D., A.B.). In every case, the PD measurements were made at the end of the primary procedure, clinical stability permitting.
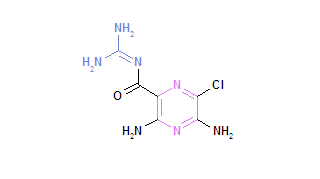
The PD catheter was attached via a three-way tap to a calomel halfcell electrode and was primed to the tip with ZCI (sodium gluconate [135 mM], calcium gluconate [2 mM], potassium gluconate [6 mM], magnesium gluconate [1 mM], HEPES [10 mM], glucose [10 mM], and isoprolcrenol [10 µM]). Values were recorded with reference to a second calomel electrode connected via a three-way tap to an intravenous line perfused with Ringer's solution. After a finger PD had confirmed the integrity of the electrical circuit (-30 mV or more), the bronchoscope was positioned in the trachea and the catheter advanced down the suction channel. The bronchoscope was maneuvered to optimize contact between the catheter tip and airway wall. Baseline measurements were attempted in the trachea, main bronchus, and lobar and segmentai bronchi, avoiding areas covered in mucus and sites of bleeding or previous lavage. Chloride secretion was assessed in either a third-generation airway (3.6-mm bronchoscope or larger) or the most distal possible wedge position (following acquisition of a 2.7-mm bronchoscope). A stable baseline was achieved for at least 30 seconds, after which the ZCI solution was perfused (0.3 ml/min^sup -1^). The response was recorded over the following 3 minutes.
The study was approved by the Ethics Committee of the Royal Brompton Hospital Trust, and all parents (and older children) gave informed consent.
Statistical Analysis
The Mann Whitney U-test was used to compare CF and non-CF groups. For the perfusion data, changes from baseline were compared after 3 minutes. Data are expressed as mean for convenience. The null hypothesis was rejected at p
RESULTS
Validation of the Single-Lumen Catheter: Adult Nasal PD Measurements
Stable baseline values could be obtained in the nose with the small, single-lumen catheter primed to the tip with ZCI solution (non-CF -14.3 [2.2] mV; CF -38.6 [5.1] mV; p
Clinical Details of Pediatric Cohort
Data were recorded on 22 children without CF age 5.6 (1.1) years and 15 children with CF age 9.1 (1.8) years (p = 0.1 for comparison of ages). The youngest child was 1 year of age and weighed 12.4 kg. Indications for bronchoscopy in the non-CF group were: recurrent chest infections (6), focal consolidation (2), stridor (3), bronchiectasis (3), chronic cough (4), severe asthma (3), and possible pulmonary tuberculosis (1). Of the CF cohort, nine children had a GA for insertion of a central line. In the remaining six, bronchoscopy was performed to obtain lower airway samples for microbiological culture. No adverse effects were seen in any child in whom recordings were made. Because of clinical instability after the primary procedure, three other patients (all without CF) were excluded after enrollment to the study before any PD measurements had been attempted. In a further three patients (two with CF, one without), measurements were attempted but could not be obtained because of technical problems with equipment.
Pediatric PD Values
Baseline. Baseline values in the trachea, main bronchi, lobar and segmentai bronchi, and the wedge position are shown in Figure 1. Tracheal values differed significantly (p
Drug perfusion responses. Responses to ZCI perfusion were recorded in a segmentai (third generation) bronchus in 23 patients (without CF, n = 15; with CF, n = 8; Figure 2 and E2 in the online supplement). The non-CF cohort demonstrated a hyperpolarization of 10.1 (2.0) mV after 3 minutes, whereas a small depolarization (1.3 [0.7] mV) was observed in the patients with CF (p
Adult Lower Airway PD Measurements
The baseline PD, measured with a double-lumen catheter, was significantly (p
DISCUSSION
The aims of this study were to (1) develop a method for measuring PD in the pediatric lower airway and (2) determine the ability of this technique to differentiate airways with and without CF. The latter would provide us with an indication of the potential of lower airway PD as an endpoint assay in clinical trials of novel gene or protein-based therapies. Our initial results from adult subjects had been encouraging in this respect, demonstrating that a double-lumen catheter technique could differentiate between the two disease groups, and was useful in a clinical trial of CFTR gene therapy (14). In this article, we have described the steps taken to adapt this double-lumen technique to the smaller pediatric lower airway and the development of a single-lumen catheter technique through which both PD can be measured and solutions can be perfused. Finally, we have confirmed that administration of a combined zero chloride and isoproterenol solution to the small airways reliably distinguishes between children with and without CF.
For lower airway PD measurements to be achievable in young children, we had several specific requirements of a technique: the catheter needed to be small enough to pass down the suction channel of the pediatric bronchoscopes; the system needed to allow for both baseline and perfusion recordings, without causing pooling of solutions in the small airways; and the protocol needed to be safe and short enough to be ethically acceptable. The 1-mm catheter was small enough for this purpose, but the potential for pooling of solutions led us to omit a perfusion step with the sodium channel blocking agent, amiloride, and to perform baseline measurements with the catheter primed to the tip with the ZCI solution. This also resulted in a shorter procedure, which we considered would increase acceptability. We confirmed in two cohorts of adult volunteers that priming to the tip with the ZCI solution did not in itself induce chloride secretion, because it neither affected the magnitude nor the stability of the nasal baseline measurements.
Baseline recordings in the pediatric trachea were significantly higher in subjects with CF than in those without. However, at no other sites were significant differences observed. This contrasts with data from our adult subjects with CF, in whom baselines were higher than those observed in the children, and disease-related differences were seen at all sites except the most distal wedge position. This difference between adults and children could be due to either technical or age-related factors. We have considered the following possibilities: (1) The single-lumen catheter system could be leading to lower PD readings than the double-lumen system. This was not apparent in the adult nasal studies, nor was this the case in the subjects without CF, because of children and adults having very similar values at each of these sites. We think therefore that this is unlikely. (2) Children have generally "leakier" airways than adults do. However, if this were the case, one might have expected similar age-related differences in the non-CF group. (3) Baseline PDs were affected by different levels of inflammation. This hypothesis requires further exploration in future studies.
Chloride secretion had already been assessed in the large proximal airways in the adult study (14). In this pediatric study, we were interested to see whether we could make similar measurements in the smaller airways. The distal airways seem to be the site where clinically apparent disease begins; they are one of the sites of relatively high CFTR expression (16), and, therefore, this may be the site at which effective CFTR function is required to correct the disease phenotype. At the start of the study, we were limited by the availability of the size 3.6-mm bronchoscope as the smallest instrument with a suction channel; chloride secretory responses were performed in a third-generation segmentai bronchus. However, during the course of the study, a prototype 2.7-mm flexible bronchoscope with a similar size channel became available, allowing measurements to be made more distally. In larger children, passage of the bronchoscope as far as a seventh-generation airway was possible; the catheter was then advanced until resistance was felt. This is the first lime that drug perfusion responses have been performed so distally in the airways, and we confirm that this approach could be used to differentiate CF from non-CF responses. However, we did encounter problems: whereas measurements in the third-generation airway clearly differentiated children with CF from those without, those in the wedge position were less clear, with a degree of overlap between groups. Of particular concern, only three of six children without CF demonstrated the expected hyperpolarization response to ZCI; in the other three, there was no change. This possibly reflects a degree of trauma at the site of measurement, which is not visible through the bronchoscope. Clearly, the technique needs further refinement before it could be reliably used at this distal site.
One limitation of this technique is the inability to include an amiloride perfusion step. In the majority of nasal protocols, amiloride is perfused before the low chloride solution and cAMP-agonist solutions. In this way, an electrical driving force in favor of chloride secretion is provided, and any changes in PD in response to ZCI cannot be attributed to movement of sodium ions. However, because the negative baseline PD is largely the result of the absorption of sodium ions, this measurement and the amiloride response are closely linked, essentially providing similar pieces of information. Finally, in the clinical CFTR gene therapy trials that have shown a functional effect (14, 17, 18), this has been in improved chloride secretion, not in reduction of sodium hyperabsorption, which may relate to these two functions requiring different levels of CFTR expression (19). For all of these reasons, we thought it most useful to devise a protocol consisting of a baseline recording (reflecting sodium ion transport) and a chloride secretion response (to a combined zero chloride and isoproterenol solution). We demonstrated in the nose of healthy volunteers that the magnitude of the response to ZCI was no different with our two protocols, one with and one without preperfusion with amiloride, which supported our decision to omit this step. Future lower airway protocols may assess any potential benefit of including this step, which would also allow direct comparison to be made between nasal and lower airway responses.
Invasive studies such as these require special consideration in children, not only related to the practicalities discussed above, but also with regard to safety and ethics (20). For these reasons, the procedure was kept as short as possible, usually being completed within 10-15 minutes. Any further perfusion steps, in addition to potentially compromising the recordings obtained, would have had the disadvantage of increasing the time required. All of these children were undergoing a GA for clinical reasons; it was not felt by either our anesthetic consultants or the Hospital Trust Ethics Committee that increasing the GA by 10-15 minutes was unsafe, although clearly this had to be discussed with the parents during the consent procedure. It is likely that most Ethics Committees would consider it acceptable to incorporate such research measurements into a clinically indicated bronchoscopy. However, unlike the children having these measurements performed at the end of such a procedure, the children with CF having an indwelling line inserted had the whole bronchoscopic procedure performed for the purpose of this research study. We felt this was justified, because it is common practice in our Institution for children with CF to have a period of intensive physiotherapy for airway clearance before recovery from GA; the bronchoscopy facilitated airway toilet as well as providing an opportunity for direct visualization of the airway and an assessment of severity of plugging. Further, many children with CF do not routinely expectorate sputum; this procedure allowed an opportunity to obtain lower airway secretions for culture purposes, with the potential for optimization of treatment.
In summary, we have described for the first time the feasibility of lower airway PD measurements in children as young as 1 year of age. Although there was significant overlap between CF and non-CF in the baseline measurements at all sites except the trachea, the chloride secretion responses differentiated successfully between children with and without CF. Such measurements could form a useful functional endpoint assay for studies of either CFTR gene or protein-based therapies in trials in the pediatric age group.
Conflict of Interest Statement: J.C.D. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; M.D. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; D.M. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; S.S. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; S.C. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; A.J. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; R.F. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; L.C. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; A.B. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; M.S. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; J.P. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; D.M.G. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; E.W.F.W.A. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript.
Acknowledgment: The authors thank the patients and their families for volunteering for the study and theater, surgical, and anesthetic staff for assistance.
References
1. Welsh MJ, Smith AE. Molecular mechanisms of CFTR chloride channel dysfunction in cystic fibrosis. Cell 1993;73:1251-I254.
2. Matsui H, Grubb BR, Tarran R, Randell SH, Gatzy JT, Davis CW, Boucher RC. Evidence for periciliary liquid layer depletion, not abnormal ion composition, in the pathogenesis of cystic fibrosis airways disease. Cell 1998;95:1005-1015.
3. Armstrong DS, Grimwood K, Carzino R, Carlin JB, Olinsky A, Phelan PD. Lower respiratory infection and inflammation in infants with newly diagnosed cystic fibrosis. BMJ 1995;310:1571-1572.
4. CF Foundation. Patient Registry 1994 Annual Data Report, CF Foundation. Bethesda, MD: CF Foundation; 1995.
5. Davies JC, Geddes DM, Alton EW. Gene therapy for cystic fibrosis. J Gene Med 2001;3:409-417.
6. Lim M, Zeitlin PL. Therapeutic strategies to correct malfunction of CFTR. Paediatr Respir Rev 2001;2:159-164.
7. Knowles M, Gatzy J, Boucher R. Increased bioelectric potential difference across respiratory epithelia in cystic fibrosis. N Engl J Med 1981; 305:1489-1495.
8. Middlelon PG, Geddes DM, Alton EWFW. Protocols for in vivo measurement of the ion transport defects in cystic fibrosis nasal epithelium. Eur Respir J 1994;7:2050-2056.
9. Wilson DC, Ellis L, Ziclenski J, Corey M, Ip WF, Tsui LC, Tullis E, Knowles MR, Durie PR. Uncertainty in the diagnosis of cystic fibrosis: possible role of in vivo nasal potential difference measurements. J Pediatr 1998;132:596-599.
10. Delmarco A, Pradal U, Cabrini G, Bonizzato A, Mastella G. Nasal potential difference in cystic fibrosis patients presenting borderline sweat test. Eur Respir J 1997;10:1145-1149.
11. Caplen NJ, Alton EW, Middleton PG, Dorin JR, Stevenson BJ, Gao X, Durham SR, Jeffery PK, Hodson ME, Coutelle C, et al. Liposome-mediated CFTR gene transfer to the nasal epithelium of patients with cystic fibrosis. Nat Med 1995;1:39-46.
12. Wilschanski M, Famini C, Blau H, Rivlin J, Augarten A, Avital A, Kerem B, Kerem E. A pilot study of the effect of gentamicin on nasal potential difference measurements in cystic fibrosis patients carrying slop mutations. Am J Respir Cm Care Med 2000;161:860-865.
13. Rubenstein RC, Zeitlin PL. A pilot clinical trial of oral sodium 4-phenylbutyrate (Buphenyl) in deltaF508-homozygous cystic fibrosis patients: partial restoration of nasal epithelial CFTR function. Am J Respir Crit Care Med 1998;157:484-490.
14. Alton EW, Stern M, Farley R, Jaffe A, Chadwick SL, Phillips J, Davies J, Smith SN, Browning J, Davies MG, et al. Cationic lipid-mecdiated CFTR gene transfer to the lungs and nose of patients with cystic fibrosis: a double-blind placebo-controlled trial. Lancet 1999;353:947-954.
15. Davies JC, Davies MG, Smith S, Jaffe A, Bush A, Scallon M, Geddes DM, Alton EW. Confirmation of abnormal chloride ion secretion in the lower airway of children with cystic fibrosis. Pediatr Pulmonol 2000;S20:293.
16. Engelhardt JF, Zepeda M, Cohn JA, Yankaskas JR, Wilson JM. Expression of the cystic fibrosis gene in adult human lung. J Clin Invest 1994; 93:737-749.
17. Porteous DJ, Dorin JR, McLachlan G, Davidson-Smith H, Davidson H, Stevenson BJ, Carothers AD, Wallace WA, Moralee S, Hoenes C, et al. Evidence for safety and efficacy of DOTAP cationic liposome mediated CFTR gene transfer to nasal epithelium of patients with cystic fibrosis. Gene Ther 1997;4:210-218.
18. Hyde SC, Southern KW, Gileadi U, Fitzjohn EM, Mofford KA, Waddell BE, Gooi HC, Goddard CA, Hannavy K, Smyth SE, et al. Repeat administration of DNA/liposomes to the nasal epithelium of patients with cystic fibrosis. Gene Ther 2000;7:1156-1165.
19. Johnson LG, Boyles SE, Wilson J, Boucher RC. Normalization of raised sodium absorption and raised calcium-mediated chloride secretion by adenovirus-mediated expression of cystic fibrosis transmembrane conductance regulator in primary human cystic fibrosis airway epithelial cells. J Clin Invest 1995;95:1377-1382.
20. Davies J, Payne D. Research applications of bronchoscopy. Paediatr Respir Rev 2003;4:230-236.
Jane C. Davies, Michael Davies, Donna McShane, Stephen Smith, Sharon Chadwick, Adam Jaffe, Raymond Parley, Louise Collins, Andrew Bush, Michael Scallon, John Pepper, Duncan M. Gecldes, and Eric W. F. W. Alton
Department of Gene Therapy, National Heart and Lung Institute, Imperial College London; Departments of Paediatric Respiratory Medicine, Thoracic Medicine, Anaesthesia, and Cardiothoracic Surgery, Royal Brompton Hospital, London, United Kingdom; and the UK Cystic Fibrosis Gene Therapy Consortium
(Received in original form August 25, 2004; accepted in final form December 30, 2004)
Supported by the Cystic Fibrosis Research Trust and by a Wellcome Trust Senior Clinical Fellowship (E.W.F.W.A.).
Correspondence and requests for reprints should be addressed to Jane Davies, M.B.Ch.B., M.D., Department of Gene Therapy, National Heart and Lung Institute, Imperial College London, Emmanuel Kaye Building, Manresa Road, London SW3 6LR, UK. E-mail: j.c.davies@imperial.ac.uk
This article has an online supplement, which is accessible from this issue's table of contents at www.atsjournals.org
Am J Respir Crit Care Med Vol 171. pp 1015-1019, 2005
Originally Published in Press as DOI: 10.1164/rccm.200408-1116OC on January 7, 2005
Internet address: www.atsjournals.org
Copyright American Thoracic Society May 1, 2005
Provided by ProQuest Information and Learning Company. All rights Reserved