Bone metastases from carcinomata are a medical and social issue. About one-half of all primary cancers tend to disseminate to the skeleton, which is the third most frequent site of metastatic spread after the lung and the liver.1 Epidemiological investigation has shown that of 1.2 million new cases of cancer each year in the USA, about 300 000 will eventually develop a bone metastasis.2,3 Tumours which have a predilection for dissemination to bone are those of the prostate (32%), breast (22%) and kidney (16%) followed by the lung and the thyroid The sites most usually involved are, in order of frequency, the spine, pelvis, ribs, skull and proximal long bones.3
The treatment of bone metastases is usually palliative and aims to achieve adequate control of pain, to prevent and resolve compression of the cord in lesions of the spine and to anticipate or stabilise pathological fractures in the appendicular skeleton. In selected cases the complete resection of an isolated bone metastasis may improve the survival of the patient.
The prognosis of patients with bone metastases is extremely variable depending on the site of the primary growth. During recent decades, the life expectancy of patients affected with metastatic carcinoma has improved considerably because of advances in chemotherapy, immunotherapy, hormonal treatment and radiotherapy. However, this improvement results in an increase in the population at risk of developing bone metastases or experiencing a pathological fracture. The reconstructive procedure requires greater reliability in order to avoid mechanical failure during prolonged survival of the patient.
At present, the treatment of bone metastases may not follow any codified protocol. The patient may be treated by different specialists such as an orthopaedic surgeon, an oncologist or a radiotherapist without any rational guideline as to the indications for surgical treatment. We have recently introduced a new protocol for the treatment of bone metastases of the appendicular skeleton which describes guidelines for indications for surgery, the type of operation to be undertaken and the methods of reconstruction available. The aim is to offer adequate individual treatment to the patient, avoiding undertreatment or overtreatment, to achieve control of pain and to manage impending and pathological fractures so that the longer survival is associated with a better quality of life.
Types of tumour
Prostate. Carcinoma of the prostate most often metastasises to the spine and pelvis. The lesions are usually osteoblastic (84%) or mixed (12%) and rarely osteolytic (4%).5 Because of their osteoblastic nature, pathological fractures are rarely seen and have a high potential for union after fixation.
The first line of treatment is hormonal therapy. Radiotherapy may be used additionally for symptomatic sites in association with or after hormone treatment. Chemotherapy is the third line of management and, finally, hemibody irradiation or systemic isotope therapy may be needed.
The response to treatment is shown radiologically by an increase in density without enlargement of the lesion. An increase in size of the metastasis, change from an osteoblastic to an osteolytic appearance and the onset of additional lesions indicate progression of the disease.
The five-year survival rate for metastatic prostate cancer is 33%.2
Breast. In metastatic breast cancer, the bone is the first site of involvement in 26% of cases but as many as 74% of patients will eventually show skeletal involvement.6 The lesions may be osteolytic, osteoblastic or mixed.
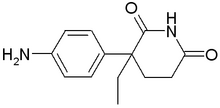
In premenopausal patients, ablative hormonal surgery by hypophysectomy, adrenalectomy or oophorectomy has shown comparable results to hormonal therapy with oestrogens, androgens, progestins, anti-oestrogens or corticosteroids. A rate of response of 50% was reported with the use of aminoglutethimide, an aromatase inhibitor, given with hydrocortisone. The same results were obtained with tamoxifen.6 On the basis of these findings, the first choice of treatment in both pre- and postmenopausal patients is usually tamoxifen. When hormonal therapy is not feasible because of the absence of oestrogen receptors, or in patients with severe extension and rapid growth of the disease, chemotherapy is indicated using either combinations of cyclophosphamide, methotrexate, fluorouracil, vincristine, prednisone (CMFVP, CMF, CFP) or adriamycin alone or in combination (FAC). A response to chemotherapy is observed in 45% to 75% of patients with a good relief of pain but with an unpredictable effect on the evolution of bone metastases.6
In 1984 Miller and Whitehill7 found that the mean survival with liver or lung metastases was 17 months, and after bone metastases 30 months. Currently, the five-year survival rate for metastatic breast cancer is 22%.2
Kidney. Metastatic lesions from carcinoma of the kidney are usually located, in order of frequency, in the lung, skeleton and brain. Bone lesions are most often osteolytic with an aggressive aspect. The cortex may disappear without periosteal reaction and soft-tissue expansion is common. In these lesions, the risk of pathological fracture is high (50%), both in the spine and in the long bones, with very little potential for spontaneous union.8
Chemotherapy is rarely successful, but treatment with interferon gives a chance of regression of 20% to 25%, especially for lesions in the lung. Although renal cancer has a low sensitivity to irradiation, a short course of palliative radiation is indicated for metastatic dissemination when there is limited life expectancy. More aggressive irradiation is recommended for indolent lesions with a better prognosis.8
Because of the intense vascularity of renal metastases, preoperative selective embolisation is recommended to reduce bleeding during the operation especially for lesions located in the spine, pelvis or shoulder girdle. After palliative fixation, repeated embolisations may be used to reduce local progression of the disease.
After resection of a solitary metastasis, the expected five-- year survival rate is 35% and an aggressive approach is justified.8 In multiple lesions, only palliative surgery is indicated and the median survival is about 12 months. Nevertheless, 25% of patients have a life expectancy ranging from three to ten years, and therefore longer-lasting reconstructive procedures are recommended.
Thyroid. Carcinomas of the thyroid are well differentiated in 85% of cases (papillary, follicular), less differentiated in 10% (Hurtle cell, medullary) and undifferentiated in 5% (anaplastic). Patients develop pulmonary metastases in 9% of cases and bone lesions in 4%. Bone metastases are usually osteolytic and hypervascularised and a solitary lesion may be observed in 30%.9
Treatment with radioactive iodine showed a complete response in 70% and a partial response in 30% of pulmonary lesions, but only a partial response in 20% to 30% of bone lesions.9
Thus the treatment of choice for solitary and late bone lesions is wide surgical resection followed by radiotherapy. Preoperative embolisation is recommended before resection or palliative osteosynthesis because intense bleeding may be expected. In pathological fractures, the rate of union after irradiation alone is 35%, rising to 85% if rigid fixation is also used.9
The overall rate of survival at five years is 44% for metastatic thyroid cancer 2 with an expected survival of less than one year for anaplastic tumours. However, with Hurtle tumours survival may occur for up to 12 years and in other types for from three to six years.9 Therefore the selection of reconstructive techniques must take account of the long-- term prognosis.
Lung. The prognosis of patients affected with carcinoma of the lung has not shown a significant improvement in recent decades. The five-year rate of survival was 12% in 1976 and 14% in 1994. The 'non-small-cell' type of bronchogenic carcinoma has a five-year survival rate of 10% after surgery, of 3% to 9% after local irradiation and of 14% after local irradiation plus chemotherapy.10 The 'small-cell' type has a worse prognosis, and it is usually treated by chemotherapy with or without radiotherapy with a disease-- free survival at two years in only 17% of cases. 10 'Small-- cell' carcinoma and adenocarcinoma frequently metastasise to the skeleton, often involving the hand or foot. The lesion is usually osteolytic and only 25% are osteoblastic.l Metastatic lung cancer has a very bad prognosis with a five-year survival rate of 2%,2 and therefore simple osteosynthesis with palliative irradiation is usually indicated.
Impending fractures
Metastatic lesions affect the strength of bone reducing stress transmission and the ability to absorb energy. The evaluation of the risk of fracture in a metastasis of a long bone is still open to debate but useful general guidelines have been established.11-14
1) Osteolytic lesions are more at risk of fracture than osteoblastic or mixed lesions. Those with a permeative pattern of osteolysis have the same risk of fracture as the more classic types which show a discrete area of lysis. Permeative osteolysis may be underestimated on plain radiographs, but MRI usually reveals the real extent of the disease (Fig. 1).
2) Highly stressed anatomical sites are particularly at risk of pathological fracture. These include the neck of the femur when there is cortical involvement, the intertrochanteric and subtrochanteric region when more than 50% of the diameter of the bone is involved, the supracondylar area and the proximal third and the midshaft of the humerus. A more aggressive surgical approach is recommended at these sites.
3) A site of endosteal or periosteal resorption with cortical thinning extending for more than 50% to 75% of the original cortical thickness is at risk of fracture (Fig. 2).
A fracture may be also predicted when interruption of the cortex in either a longitudinal or coronal plane exceeds 50% of the diameter of the bone as measured at the same level (Fig. 3). This feature may be difficult to evaluate on plain radiography and CT is the best imaging technique to assess extension of cortical breakdown. A cortical defect in the femur which extends for 2.5 cm or more is at high risk of fracture. In our series, a fracture was observed in 55% of patients with lesions of this size in the femur which had been treated by irradiation without prophylactic fixation.
4) The possibility of pathological fracture must be considered in any lesion of any radiographical type or size in a major long bone which shows persistent pain on weight-- bearing or local progression after irradiation or chemotherapy.
A scoring system to define the risk of pathological fracture which considers the site, pain, the radiological appearance and the size of the lesion was introduced by Mirels 13 (Table I). A low risk of fracture was predicted for patients with a mean average score of 7 (4 to 9) and a high risk for a mean score of 10 (7 to 12).
Sites of metastases
Pelvis and acetabulum. The pelvis is the most frequent site of metastatic carcinoma after the spine. Lesions of the wing of the ilium, the sacroiliac joint or the anterior arch of the pelvis are not at risk of mechanical failure and may usually be treated successfully by irradiation. At these sites operation is required only for solitary and late lesions and when patients have a favourable prognosis. In these cases, removal of the tumour by wide resection or extensive curettage may improve survival.
Periacetabular lesions are usually painful under weight-- bearing and are at risk of mechanical failure with consequent progressive protrusio acetabuli. Surgical treatment is therefore indicated in order to achieve relief of pain, restoration of function and to allow early weight-bearing. The treatment of choice is a cemented total hip arthroplasty using appropriate techniques of reconstruction according to the amount of bone loss.15 Postoperative radiotherapy is always recommended. Therefore the prosthetic components must be cemented and bone grafting avoided since bone ingrowth into a cementless implant and incorporation of graft is severely impaired by radiotherapy.
When the medial wall of the acetabulum is involved, special cups with a screwed lateral flange may be used to prevent medial migration and a metal mesh placed on the medial wall before cementation. Different types of reinforcement ring may be used when both the medial and lateral wall of the acetabulum are destroyed (Fig. 4). 15
An alternative technique was introduced by Harrington utilising cement to fill the defect which is reinforced by Steinmann pins placed into the pubic and ischial rami and from the acetabular dome to the sacroiliac joint. This system allows better distribution of stress from the acetabular component to the spine providing durability of the implant for a longer term.
For massive bone loss, or after wide resection for a solitary lesion, prosthetic replacement with modular or custom-made prostheses is a useful option. The saddle prosthesis is modular and easy to assemble but may be unstable and lead to long-term wear of the wing of the ilium, or breakage with consequent migration. Custommade pelvic prostheses are designed from preoperative three-dimensional CT scans but may be found not to match at operation. Simple screw fixation to the residual pelvis is at risk of failure when postoperative radiotherapy is performed. Concerns have been raised as to the cost-effectiveness of the use of these devices in patients with metastases.
Hip and proximal femur. The proximal femur is the most frequent site of mechanical failure in patients with metastases and surgical treatment is recommended for all impending or pathological fractures at this site, except in bedridden patients with a life expectancy of less than two months.
Preoperative MRI of the entire femur and pelvis is indicated in order to detect any acetabular involvement, to define the extension of the tumour into the femoral shaft and to identify other metastatic foci in the distal medullary canal.
When the acetabulum is not involved, the use of bipolar cups is recommended because of their intrinsic stability. For metastatic lesions limited to the head and neck of the femur, a conventional prosthetic replacement is recommended. Long-stem implants are preferred in order to reinforce the shaft and to prevent failure in case of progression of the disease. In some cases, when the calcar area is destroyed, special prostheses may be required to replace it.
For lesions which also involve the trochanteric and metaphyseal area, simple osteosynthesis using a screw-- plate or intramedullary nails may give results which are inadequate in terms of long-term durability, especially when the medial cortex of the femur is not restored. When the fixation is reinforced with cement to restore the medial bone loss the results are improved, but the high mechanical stresses at this level, and the risk of necrosis of the femoral head because of postoperative irradiation, will eventually lead to failure of the implant. This intralesional procedure involving a wide exposure, curettage, filling with cement and osteosynthesis has no significant advantages in terms of operating time, blood loss, rate of complications and recovery time compared with a 'more aggressive' wide resection and reconstruction with a prosthesis. Moreover, intralesional curettage, which is the technique of choice in benign lesions, is oncologically inadequate to control a highly malignant tumour, such as a metastasis, and local recurrence may be expected if the patient survives for a long term and has no other effective adjuvant treatment such as cryosurgery or radiotherapy.
For these reasons, resection of the proximal femur and reconstruction with a cemented modular megaprosthesis is our preferred method of treatment (Fig. 5).
The 'ideal implant' should be modular so that it can be assembled according to the intraoperative requirements, long-stemmed in order to reinforce the medullary canal as much as possible and cemented since the cement acts as an adjuvant, sterilising any residual tumour foci in the medullary canal. Pre- or postoperative radiotherapy does not affect cemented implants but ingrowth of bone in uncemented prostheses is jeopardised by irradiation. Usually, no intramedullary plug for restriction of cement is used, allowing the cement to fill the distal metaphysis and to reinforce the entire medullary canal. This avoids stress-- raising at the tip of the stem or along the medullary canal. Accurate cleaning of the bone marrow and drilling of the supracondylar cortex for venting are recommended to prevent possible embolism due to high-pressure injection of the cement.
In order to allow immediate weight-bearing, which is a major objective in these patients, every effort must be made to improve stability of the hip and to avoid subsequent dislocation. This is a frequent complication in the early postoperative period because of the lack of muscle control after detachment of major muscles, such as the glutei, quadriceps and iliopsoas, and inadequate reattachment to the prosthesis. The following recommendations are given to improve stability in a megaprosthesis of the hip.
1) Intrinsically stable joints should be used if possible and a bipolar cup is usually the prosthesis of choice. When acetabular replacement is required because of involvement by tumour, associated osteoarthritis or postradiation deterioration of the articular cartilage, the use of either a snap-fit socket or a large prosthetic femoral head (size 28 to 32 mm) is strongly recommended.
2) It is important to try to save as much of the joint capsule as possible in order to close it around the neck of the prosthesis. A Marlex mesh tube may be used as reinforcement or as a substitute for the joint capsule, and it should be wrapped around the prosthesis with its proximal end sutured along the acetabular rim.
3) Reinsertion of detached muscles must be very accurate.
A longitudinal tension band suturing gluteus medius to quadriceps is first established and this then provides the anchorage for the reattachment of iliopsoas, gluteus maximus and the external rotators. Artificial devices such as polyethylene plates, artificial ligaments and metal grips for the direct fixation of muscles to the prosthesis, may temporarily improve the fixation but they are rarely effective alone. To achieve better muscle control, in selected cases we suggest a wider use of allograft with composite prostheses which have sites for the reinsertion of tendons.
4) An external orthosis (articulating pelvic hip brace) may be used for one month in order to protect muscle reattachments from excessive stresses during early weightbearing.
Knee and ankle. The knee and ankle undergo loading forces which are mainly compressive. The tensile and torsional forces are lower than in the proximal femur, thus decreasing the risk of mechanical failure. A metastatic lesion involving less than half of the epiphyseal or metaphyseal area may be treated successfully by open curettage and plate fixation, filling the defect with PMMA cement. When the lesion involves more than one-half of the epiphyseal or metaphyseal area, an intra-articular resection is indicated. Reconstruction of the distal femur and/or proximal tibia may be performed using modular cemented megaprostheses (Fig. 6). A hinge joint with a posterior axis is recommended to afford passive stability in hyperextension, even after major excisions of the quadriceps. 16 After proximal resection of the tibia, several techniques have been described to improve reattachment of the patellar tendon including reinforcement by artificial ligaments or fascia lata grafts, transposition of the proximal head of gastrocnemius, multiple osteotomies of the fibula with anterior reposition of its head, and turning down a patellar-- quadriceps osteotendineous graft. However, we routinely use a flap of the medial gastrocnemius in these patients. This technique allows biological reattachment of the patellar tendon and achieves better soft-tissue coverage, minimising the risk of wound dehiscence and infection.
No suitable prosthetic device is yet available after resection of the distal tibia. The only reconstructive option is arthrodesis of the ankle using autografts or allografts reinforced by a tibial intramedullary rod locked proximally into the tibia and distally into the talus and calcaneum. Radiotherapy is not indicated because of its interference with the incorporation of the bone graft and fusion of the arthrodesis.
Shoulder girdle. Metastatic lesions of the scapula and clavicle may be treated conservatively by radiotherapy in most cases. Surgical treatment is indicated for solitary lesions from tumours with a favourable prognosis. Wide resection may be performed and no reconstruction is required.
The proximal humerus is at risk for pathological fractures because of the extreme bending and rotational forces from the muscle insertions. The metaphysis is largely cancellous and a stable fixation is often difficult to achieve especially in older osteoporotic patients. Therefore, the recommended treatment for metastases in the proximal humerus is a shoulder arthroplasty. The epiphyseal lesions may be treated by a conventional cemented long-stemmed prosthesis, preserving the insertion of the rotator cuff on the greater tuberosity. If the lesion extends to the metaphysis, a modular prosthesis must be used. Accurate reattachment of the rotator cuff, deltoid and pectoralis major to the prosthesis by non-absorbable sutures is recommended to improve stability and residual function. Recent prostheses have several holes in the metal body through which strips of artificial ligaments or fascia lata may be passed to afford better reattachment of muscle. The stability of the shoulder may also be improved by using suspension bands to the acromion, and by wrapping an artificial mesh around the prosthetic head to be sutured to the remaining rotator cuff or to the edges of the glenoid cavity.
Shafts of major long bones. Pathological fractures of major long bones are common and have dramatic physical and psychological consequences for the patient.1? The indications for prophylactic fixation depend on the site and size of the defect. The diaphyses of the femur, the humerus and the tibia are at most risk. As discussed above, it has been conventionally accepted that lesions with an absolute (>2.5 cm) and relative (>50%) size of the defect require treatment. Other factors to be taken into account are the general status of the patient, the life expectancy and the predicted response to adjuvant therapy. When a fracture does occur surgical treatment is always necessary with conservative care indicated only in patients in a terminal state.
For patients in a poor general condition with a bad prognosis and in those who have a good predictive response to radiotherapy, a simple osteosynthesis without open curettage may be considered. Intramedullary rods are usually preferred because of the limited surgical exposure and intraoperative bleeding. Surgical access is distant from the lesion and immediate postoperative irradiation may be administered. The rod is closer to the mechanical axis than a plate and locking screws can be placed in normal bone at a distance from the lesion. The use of the latest design of nail, locked proximally and distally, is recommended. These devices provide immediate stability, allow early weight-bearing and avoid telescoping in the presence of massive intercalary resorption. Other devices such as Steinmann pins and Rush, Ender or conventional Kuntscher nails are not strong enough and do not prevent telescoping and rotational instability.
A more aggressive approach is indicated in patients with a good prognosis or in those who have a poor predictive response to adjuvant treatment. The defect is widely curetted, filled with PMMA and fixed by a plate or intramedullary nail in order to achieve a reinforced osteosynthesis (Fig. 7). When a rod is used, PMMA may be injected under pressure by a cement gun into the medullary canal before insertion of the implant in order to reinforce the fixation and to prevent failure due to progression of the disease. 8 The operative working time of the PMMA may be prolonged by cooling the liquid monomer. A tourniquet inflated around the limb at the level of the osteolytic area during injection may help to prevent extrusion of cement into the soft tissues. Venting by drill holes in the anterolateral cortex of the femur may decrease the risk of embolic phenomena during injection of the cement. The latter may also sterilise residual microfoci of the tumour either by the direct heat of polymerisation or the toxic effect of release of monomer. Antibiotics or chemotherapeutic drugs may be added to the cement in order to reduce the risk of infection and to improve local control of the tumour. After curettage, local adjuvants such as phenol or liquid nitrogen may be used to enhance local control.
Anderson et al19 noted a higher mechanical strength with the use of two orthogonal plates and cement, and an increase in the load for torsional failure by a factor of 2.6 and in bending failure by 4.2 with respect to intramedullary fixation. Nevertheless, this procedure is rarely indicated since it requires an extensive surgical exposure with excessive blood loss, increasing the risk of local and general complications.
In selected cases of solitary diaphyseal lesions with a good prognosis, wide intercalary resection is indicated. The reconstruction may be performed using intercalary prostheses with cemented stems and modular components joined by a morse taper.
Curettage and local adjuvants in bone metastases. When removal of tumour tissue by open curettage is indicated, the wall of the cavity may be cleaned using curettes, gouges and high-speed burrs. Local adjuvants may be used to improve sterilisation of the margins. Highly concentrated phenol (80%) is effective in sterilising the surface of the cavity wall. Soaking of the surface three times is followed by lavage with alcohol and saline solution. Electrocauterisation of the bony walls, especially if performed with argon, has a haemostatic effect and a sterilising property of 1 mm. Methylmethacrylate has an adjuvant thermal and toxic effect during polymerisation. The thermal effect is greater in cancellous bone (2 to 3 mm) than in cortical bone (0.5 mm). Deep freezing and thawing of the cavity may be performed with liquid nitrogen or by filling the cavity with a sterile gel and inserting a probe connected to a device monitoring temperature and the rate of freezing. After carrying out the freezing-thawing procedure three times, a ring of necrosis of 1 to 2 cm is obtained. Cryotherapy represents the most effective local adjuvant, but there are concerns as to weakening of the bone and possible damage to soft tissues. 20
Guidelines for surgical treatment
The treatment of bone metastases requires a multidisciplinary approach with clear delineation of the roles of the orthopaedic surgeon, oncologist and radiotherapist. We have introduced a prospective protocol containing guidelines on the indications for surgery and on the type of procedure which should be undertaken. Factors taken into account include the expected survival, the type and stage of the tumour, visceral spread, the status according to Karnofsky and Burchenal,21 the time since detection of the primary tumour, the risk of pathological fracture and the predictive sensitivity to chemotherapy, hormonal therapy and irradiation.
Management protocol. Patients are placed in one of four classes (Table II) as follows.
Class 1. Those with a single metastatic lesion of a primary tumour with a good prognosis and an interval of more than three years from detection of the primary lesion to the development of bone metastasis. Primary tumours with a favourable prognosis include well-differentiated thyroid, prostate, breast when sensitive to hormonal treatment or chemotherapy, clear-cell renal and colorectal carcinoma. Myeloma and hymphoma are included since their biological behaviour and the mechanical implications are similar to those of metastatic disease.
Class 2. Patients with a pathological fracture in a major long bone.
Class 3. Patients with radiological and/or clinical signs of impending fracture in a major long bone or the periacetabular area.
Class 4. Patients with: a) osteoblastic lesions at all sites; b) osteolytic or mixed lesions in non-weight-bearing bones such as the fibula, ribs, sternum or clavicle; c) osteolytic lesions in major bones with no impending fracture; and d) lesions in the wing of the ilium, anterior pelvis or scapula (excluding patients included in class 1).
All patients included in classes 1, 2 and 3 should have a priority referral to an orthopaedic oncologist for surgical treatment. After surgery they should be referred back to an oncologist and/or a radiotherapist for adjuvant treatment if indicated. Patients in class 4 should be treated conservatively by chemotherapy, hormonal therapy and/or irradiation according to the diagnosis. The response to treatment and the control of pain should be carefully evaluated at follow-up. In the case of pathological fracture, persistence of pain for two months after completion of treatment or radiological signs of local progression, the patients should be referred to an orthopaedic surgeon for surgical treatment since they are now in either class 2 or class 3 (Fig. 8).
Types of operation
In Table III the different types of osteosynthesis and reconstructive device are described. Their use is discussed in relation to the class of the patient and the site of the bone metastasis.
Class 1. In these patients, the metastasis is treated as a primary tumour and the operation aims to achieve a long-- term cure, both oncologically and mechanically. An articular or intercalary resection is performed with wide surgical margins and the defect is reconstructed by a cemented megaprosthesis or an intercalary spacer. Single metastatic lesions located in expendable bones, such as the fibula, ribs and clavicle, may be resected without any functional impairment. Lesions of the scapula in class-1 patients should be treated by scapulectomy with consequent loss of the abductor function. Wide resection of the wing of the ilium and the anterior pelvic arch may be performed without any functional impairment. In these cases, no reconstruction is usually required except for reinforcement by synthetic mesh to avoid visceral herniation. Wide resection of periacetabular lesions requires demanding prosthetic reconstruction, as previously described.
Classes 2 and 3
Metaphysis of long bones. The recommended treatment for these sites in class-2 and class-3 patients is shown in Figure 9 in which area I (the epiphysis) and area 2 (the metaphysis) are considered separately.
At the proximal end of the humerus and femur the risk of pathological fracture is considerable because of the high rotational and weight-bearing forces. For this reason aggressive treatment by resection and prosthetic replacement is recommended to allow an early functional recovery and to avoid later failure due to progression of the disease. If wide oncological margins are achieved at resection, postoperative radiotherapy can be avoided, but it is still recommended after marginal or intralesional procedures or in patients presenting with a pathological fracture. It should be delivered with full doses (3000 to 5000 cGy) and not the levels used for palliative control of pain. A long-stemmed cemented conventional prosthesis may be used in epiphyseal involvement, while metaphyseal resection requires reconstruction by a cemented megaprosthesis.
The risk of mechanical failure is lower in the elbow, knee and ankle. When less than one-half of the bone is involved, curettage with cement filling and plate osteosynthesis is recommended. When curettage is performed, local adjuvant treatment using cryotherapy, phenol etc., is strongly recommended and postoperative radiotherapy should be used. Extension of the tumour to more than one-half of the metaphyseal area may be managed by intra-articular resection and prosthetic replacement of the distal humerus, distal femur or the proximal tibia or by arthrodesis of the ankle. Diaphysis of long bones. A scoring system has been introduced for assessment of diaphyseal metastasis in patients in classes 2 and 3 (Table IV) which takes into account the expected survival (Table V), the site of the lesion, its dimensions and the response to adjuvant treatment (Table VI). The score ranges from 3 to 15 points for each patient. Simple osteosynthesis (Al) is recommended for those with a low score (
Periacetabular area. In the periacetabular area, conservative treatment is indicated for osteoblastic or mixed lesions with a good predictive response to irradiation. Weightbearing should be proscribed during treatment by radiotherapy. Surgical treatment is indicated in class-1 patients, in those in class 2 with a protrusio acetabuli and in those in class 3 with osteolytic lesions and a poor predictive response to adjuvant management. Preoperative angiography and selective embolisation are recommended in highly vascular lesions such as clear-cell or thyroid carcinomata. When the subchondral bone of the acetabulum is not involved, a simple curettage of the lesions may be performed with cement filling, thus preserving the hip. This procedure may be carried out percutaneously. Metal pins or bars inserted into intact bone may be used as augmentation to reinforce the acetabular dome. Destruction of the subchondral bone and protrusio acetabulae require total hip replacement with special reinforcement devices such as pins, bars, rings and cemented self-retaining sockets or a saddle prosthesis.
References
1. Hage WD, Aboulafia AJ, Aboulafia DM. Incidence, location and diagnostic evaluation of metastatic bone disease. Orthop Clin North Am 2000;31:515-28.
2. Cancer facts and figures. Atlanta: American Cancer Society, 1999: 1-36.
3. Silverberg E. Cancer statistics 1986. CA Cancer J Clin 1986; 36:9-25.
4. Clain A. Secondary malignant disease of bone. Br J Cancer 1965; 19:15-29.
5. Richardson RL, Swee RG, Sim FH, Schray MF, Wold LE. Prostate cancer. In: Sim FE, ed. Diagnosis and management of metastatic bone disease: a multidisciplinary approach. New York: Raven Press, 1988:273-81.
6. Ingle JN, Sim FH, Schray MF, Wold LE, Beabout JW. Breast cancer. In: Sim FH, ed. Diagnosis and management of metastatic bone disease: a multidisciplinary approach. New York: Raven Press, 1988:251-63.
7. Miller F, Whitehall R. Carcinoma of the breast metastatic to the skeleton. Clin Orthop 1984;184:121-7.
8. Hahn RG, Sim FH, Scott SM, et al. Renal cell cancer. In: Sim FH, ed. Diagnosis and management of metastatic bone disease: a multidisciplinary approach. New York: Raven Press, 1988:283-90.
9. Hay ID, Rock MG, Sim FH, et al. Thyroid cancer. In: Sim FH, ed. Diagnosis and management of metastatic bone disease: a multidisciplinary approach. New York: Raven Press, 1988:305-17.
10. Frytak S, McLeod RA, Gunderson LL, Pritchard DJ, Unni KK. Lung cancer. In: Sim FE, ed. Diagnosis and management of metastatic bone disease: a multidisciplinary approach. New York: Raven Press, 1988:305-17.
11. Bechtol CO. Bone as a structure. In: Bechtol CO, Ferguson AB, Laing PG, eds. Metals and engineering in bone and joint surgery. Baltimore: Lippincott, Williams & Wilkins, 1959:127-42.
12. McBroome RY, Hayes WC, Poon P. Strength reduction of endosteal defects in diaphyseal bone. Trans Orthop Res Soc 1986; 11:65.
13. Mirels H. Metastatic disease in long bones: a proposed scoring system for diagnosis of impending pathologic fractures. Clin Orthop 1989;249:256-64.
14. Pugh J, Sherry HS, Futterman B, Frankel VH. Biomechanics of pathologic fractures. Clin Orthop 1982;169:109-14.
15. Harrington KD. Orthopaedic management of extremity and pelvic lesions. Clin Orthop 1995;312:136-47.
16. Capanna R, Ruggieri P, Biagini R, et al. The effects of quadriceps excision on functional results after distal femoral resection and prosthetic replacement of bone tumors. Clin Orthop 1991;267:186-96.
17. Yazawa Y, Frassica FJ, Chao EYS, et al. Metastatic bone disease: a study of the surgical treatment of 166 pathological humeral and femoral fractures. Clin Orthop 1990;251:213-9.
18. Sim FH, Daugherty TW, Ivins JC. The adjunctive use of methylmethacrylate in fixation of pathological fractures. J Bone Joint Surg [Am] 1974;56-A:40-8.
19. Anderson JT, Erickson JM, Thompson RC Jr, Chao EY. Pathologic femoral shaft fractures comparing fixation techniques using cement. Clin Orthop 1978;13:273-8.
20. Gitelis S, McDonald DJ. Adjuvant agents and filling materials. In: Simon MA, ed. Surgery for bone and soft tissue tumours. Springfield: Lippincott-Raven, 1998:133-57.
21. Karnofsky DA, Burchenal JH. The clinical evaluation of chemotherapeutic agents. In: McLeod E, ed. Evaluation of chemotherapeutic agents. New York: Columbia University Press, 1949.
R. Capanna, MD, Chairman
D. A. Campanacci, MD, Consultant Orthopaedic Oncologist
Department of Orthopaedic Oncology, Orthopaedic Traumatology Centre, Largo Palagi 1, 50139 Florence, Italy.
Corresoondence should be sent to Dr R. Caranna.
Copyright British Editorial Society of Bone & Joint Surgery May 2001
Provided by ProQuest Information and Learning Company. All rights Reserved