Study objectives: To examine the effects of long-term intermittent dobutamine infusion, combined with oral amiodarone in patients with congestive heart failure (CHF) refractory to standard medical treatment.
Design: Prospective, randomized, double-blind, placebo-controlled clinical trial.
Setting: Inpatient and outpatient heart failure clinic in a university teaching hospital.
Patients and interventions: Thirty patients with end-stage CHF refractory to standard medical treatment who could be weaned from dobutamine therapy after a first 72-h infusion were randomized in a double-blind manner to receive IV infusions of placebo (group 1; 14 patients) vs dobutamine in a dose of 10 [micro]g/kg/min (group 2; 16 patients) for 8 h every 14 days. All patients received standard medical therapy and also were treated with oral amiodarone, 400 mg/d, which was started at least 2 weeks before randomization.
Measurements and results: Kaplan-Meier survival analysis showed a 60% reduction in the risk of death from any cause in the group treated with the combination of dobutamine and amiodarone, compared with the group treated with placebo and amiodarone (hazard ratio, 0.403; 95% confidence interval, 0.164 to 0.992; p = 0.048). The 1-year and 2-year survival rates were 69% and 44%, respectively, in the dobutamine-treated group, vs 28% and 21%, respectively, in the placebo-treated group (p < 0.05 for both comparisons). Median survival times were 574 and 144 days, respectively, for groups 2 and 1. At 6 months, the New York Heart Association functional class was significantly improved in the patients who survived from both groups.
Conclusions: Long-term intermittent dobutamine infusion combined with amiodarone added to the conventional drugs improved the survival of patients with advanced CHF that was refractory to conventional treatment. (CHEST 2004; 125:1198-1204)
Key words: heart failure: inotropic agents; survival
Abbreviations: CHF = congestive heart failure; CI = confidence interval; LVEF = left ventricular ejection fraction; LV = left ventricle, ventricular; NYHA = New York Heart Association; REMATCH = Randomized Evaluation of Mechanical Assistance for the Treatment of Congestive Heart Failure; [Vo.sub.2]= oxygen uptake
**********
Congestive heart failure (CHF) is usually associated with progressive deterioration of left ventricular (LV) function and a poor long-term prognosis. (1) Patients with severe CHF have a 1-year mortality rate that can exceed 50%e and have a high incidence of ventricular arrhythmias, and > 40% of them die suddenly. (3) The long-term oral administration of most positive inotropic agents is associated with increased mortality. (4-7) Digoxin remains the only oral positive inotropic agent without an adverse long-term effect on survival. (8) Positive inotropic agents administered IV improve the hemodynamics of patients with acute and chronic heart failure. However, data from randomized trials suggest that long-term treatment with positive inotropic agents decreases the survival of patients with heart failure, regardless of the agent used. (9) Despite their negative effect on survival, positive inotropic agents are commonly used in the management of severe chronic heart failure. In addition, there are data from nonrandomized studies suggesting that the use of positive inotropic agents in combination with [beta]-blockers (10) or amiodarone (11) might be useful in a subset of patients with end-stage heart failure.
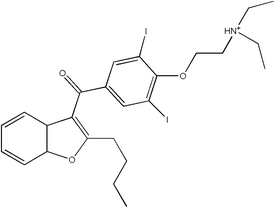
Amiodarone, a potent antiarrhythmic agent (12) with antiadrenergic properties (13,14) has a minimal negative inotropic effect (13) and may prolong the survival of patients with heart failure. (14) Dobutamine, a potent inotropic agent, improves the hemodynamic, and clinical conditions of patients with CHF who are refractory to standard medical treatment, (15-18) but does not increase their survival. (19) Studies of oral inotropic agents have suggested that the number of hospitalizations and deaths from heart failure may be increased. However, because a proarrhythmic effect of dobutamine (20) appears to play a pivotal role in the increased mortality of patients treated with long-term intermittent dobutamine infusion, we postulated that adding amiodarone to dobutamine treatment would prevent the deleterious effects on survival associated with dobutamine treatment.
In a previous nonrandontized study, (11) we found that long-term intermittent dobutamine infusions combined with oral amiodarone and standard medical therapy improved the survival of patients with refractory CHF, when compared with patients receipting long-term intermittent dobutamine infusions and standard medical treatment but no amiodarone. We hypothesized that a synergistic effect of amiodarone and dobutamine improved survival in these patients. The purpose of this study was to test this hypothesis in a randomized, double-blind protocol.
MATERIALS AND METHODS
Patient Selection
This randomized, double-blind, placebo-controlled study included 30 patients with CHV that was refractory to standard therapy, including digoxin, enalapril, spironolactone, and diuretics, who could be weaned from an initial 70-h infusion of dobutamine.
All patients were treated with amiodarone, 400 mg/d, but those with an internal cardioverter defibrillator were treated with 800 mg/d, in addition to standard therapy. All patients previously had not responded to oral metoprolol. 6.25 mg bid, demonstrating clinical deterioration that was resistant to a diuretic dose increase. Treatment with amiodarone was staffed at least 2 weeks before randomization to biweekly 8-h IV infusions of placebo (group 1) vs biweekly 8-h IV infusions of dobutamine, 10 [micro]g/kg/min, in the same vehicle as group 1 (group ,9). Nine patients with decompensated CHF who could not be weaned from IV dobutamine therapy were not enrolled in the study. Randomization was stratified based on the presence vs absence of coronary artery disease using a randomized block (Table 1). The ethical review board of our institution approved this study, and all patients had granted their written reformed consent to participate.
Study Design
Thirty patients enrolled in the study based on an assumed prespecified difference of at least 262 days between the two treatment groups, a two-sided significance level of 0.05, and power of 80%. Patients were allocated to treatment at random, in a 1:1 ratio. One interim analysis was planned and performed.
Patients with decompensated chronic CHF, despite receiving optimal standard management, were hospitalized for the initiation of continuous IV dobutamine infusion of 10 [micro]g/kg/min for up to 72 h. All patients who could be weaned from the dobutamine infusion within 72 h were treated with oral amiodarone, 400 mg/d for at least 2 weeks, and subsequently were rehospitalized and randomized to group 1 vs group 2. The first infusion began 2 weeks after the initial stabilization and was continued every 2 weeks thereafter, even if there was clinical improvement. If a patient's clinical and/or hemodynamic condition worsened, weekly infusions of placebo or dobutamine were started. Subsequently, if the clinical condition remained unchanged after 2 weekly infusions or worsened, at any time during follow-up, the randomization code was broken, and the patient began receiving weekly infusions of dobutamine as destination therapy or until cardiac transplantation for the listed candidates.
All patients underwent a baseline clinical and laboratory evaluation, including echocardiography and radionuclide ventriculography to measure LV ejection fraction (LVEF). These tests were repeated at 3 and 6 months of follow-up, along with an exercise stress test.
The primary end point of the study was death from any cause. Secondary end points were changes in functional status, hemodynamic variables, INEF, LV dimensions, arrhythmias, and maximum oxygen uptake ([Vo.sub.2]). All patients were evaluated before infusion for their clinical situation and biochemical status.
Statistical Analysis
The Kaplan Meier method was used to estimate the 1-year and 2-year survival curves for each treatment group. The log-rank statistic was used to compare differences between groups in the primary end point (death from any cause). Cox proportional hazards regression analysis was used with dobutamine treatment as a variable to estimate relative risks, 95% confidence intervals (CIs) and corresponding p value. Analyses were performed according to the intention-to-treat principle, including the patients placed on weekly infusions of dobutamine because Of the deterioration of their clinical stains.
The Student t test was used for unpaired observations to evaluate differences between secondary end point variables in the two groups. In patients who had two repeat evaluations, the Student paired t test was used to identify changes with time in the same group of patients. When the underlying assumptions of the t test models were violated, the Mann-Whitney U test or the Wilcoxon test was used.
RESULTS
Patient Groups
Group 1 included 14 patients (mean [[+ or -] SD] age, 61 [+ or -] 8.2 years) who received biweekly placebo infusions, and group 2 included 16 patients (mean age, 64 [+ or -] 9.9 years) who received biweekly dobutamine infusions. In both groups, randomization and IV infusions were started 2 weeks after they had stabilized from an episode of cardiac decompensation that was refractory to standard treatment. All patients received long-term amiodarone therapy, 400 mg/d, orally in addition to standard medical therapy. All patients had a radionuclide LVEF of < 35%. There were no differences between the two groups with respect to clinical or hemodynamic status, biochemical measurements, or drag regimens (Table 1).
Four of 14 patients (28%) in group 1 crossed over to dobutamine therapy after 3, 12, 16, and 51 weeks of placebo treatment. Clinical deterioration also was observed in 4 of 16 patients (25%) in group 2 after 16, 20, 36, and 52 weeks of treatment, mad thereafter they were treated with weekly dobutamine infusions.
The Kaplan-Meier estimates of survival for 1 year were 69% in group 2 vs 28% in group 1 (p = 0.0187). Two-year survival rate estimates were 44% vs 21%, respectively, in group 2 vs group 1 (p = 0.0412) [Fig 1]. The combination of dobutamine and amiodarone in addition to standard treatment (group 2) was associated with a 7] % reduction in the risk of death from any cause (hazard ratio, 0.294; 95% CI, 0.1 to 0.869; p = 0.027) at 1 year and a 60% risk reduction at 2 years (hazard ratio, 0.403; 95% CI, 0.164 to 0.992; p = 0.048). The median survival time was 574 days for dobutamine-treated patients (group 2) and 144 days for group 1 patients. At the final analysis (mean of the two groups median duration of follow-up, 359 days; range, 7 to 728 days), 9 deaths had occurred in group 2, and 11 deaths had occurred in group 1. There were seven survivors in group 2 (44%) vs three survivors in group 1 (21%). Table 2 lists the causes of death. End-stage heart failure was the cause of death in 64% of patients in group 1, and in 67% of patients in group 2 (p = 0.890).
[FIGURE 1 OMITED]
Hemodynamic Measurements at 3 Months
There were no significant changes in LVEF or pulmonary capillary wedge pressure (PCWP) at 3 months of follow-up in either group (Table 3). However, at 6 months, PCWP had significantly decreased from 32 [+ or -] 5.4 mm Hg to 26 [+ or -] 7 mm Hg in group 2 (p = 0.012).
Functional Evaluation at 3 and 6 Months
At the 3-month follow-up, the functional status of group 1 patients improved significantly from a mean New York Heart Association (NYHA) class 4.0 to 3.2 [+ or -] 0.9 (p = 0.048; nine patients). In group 2, the mean NYHA functional class decreased from 4.0 to 2.8 [+ or -] 0.7 (p = 0.001; 13 patients). The maximum mean [Vo.sub.2] in patients able to undergo cardiopulmonary exercise testing was 12.9 [+ or -] 3.5 mL/kg/min in group 1 (five patients) and 12.8 [+ or -] 3.1 mL/kg/min in group 2 (nine patients) [Table 3].
At 6 months, the mean NYHA functional class was 2.2 [+ or -] 0.9 in group 1 (p = 0.035 vs baseline; four patients), and the mean peak [Vo.sub.2] was 13.2 [+ or -] 1.9 mL/kg/min (three patients). In group 2, the mean NYHA class was 2.3 + 0.5 (p = 0.001 vs baseline; 10 patients), and the mean peak [Vo.sub.2] was 12.6 [+ or -] 2.4 mL/kg/min (six patients).
DISCUSSION
Long-term intermittent dobutamine infusions combined with oral amiodarone resulted in a significant increase in the survival of patients with severe CHF that is refractory to standard medical treatment, including amiodarone. Patients in the control group received optimal medical care with digoxin, furosemide, spironolactone, enalapril, amiodarone, and intermittent placebo infusions, from the same heart failure specialists who managed the patients in group 2. All patients were admitted to the same ICU and received the same level of medical care, including infusions of dobutamine or placebo in a double-blind manner. Treatment with amiodarone hid the effect of dobutamine on heart rate, such that physicians and patients remained unaware of the treatment assignment. The 1-year mortality rate of 72% and the median survival time of 144 days in the control group were similar to the 75% 1-year mortality rate and the 150-day median survival time reported in the Randomized Evaluation of Mechanical Assistance for the Treatment of Congestive Heart Failure (REMATCH) study. (21) These similarities corroborate the severity of the heart failure of the patients included in this study.
Strikingly, the 31% 1-year mortality rate and the median survival time of 574 days in our patients who were treated with intermittent dobutamine infusions and oral amiodarone were similar to, if not better than, the 48% 1-year mortality rate and the 408-day median survival time reported in the LV assist device group of the REMATCH trial. (21) These similarities emphasize the significant reduction of the mortality rate by the dobutamine infusions combined with oral amiodarone therapy. Our patients had a somewhat higher LVEF than that reported for patients in the REMATCH trial. Tiffs difference may be attributed to an amiodarone effect as was shown in the Congestive Heart Failure: Survival Trial of Antiarrhythmic Therapy study. (22) Furthermore, 50% of our patients had moderate-to-severe mitral regurgitation, which may have contributed to a higher LVEF measurement in our study.
The patients included in the present study had severe cardiac disease. The mortality rate in the control group was higher than that reported by other randomized trials of treatment for heart failure. (4-8,14,11,23) Patients in both groups who were able to undergo exercise testing at 3 and 6 months of follow-up had a mean peak [Vo.sub.2] of only 12.8 [+ or -] 3.1 mL/kg/min, which is highly predictive of early mortality. (24) The remaining patients who were unable to exercise may have been in even worse condition than those who underwent exercise testing.
There are no precise guidelines for the management of patients with chronic LV systolic dysfunction who present with decompensated heart failure despite optimal therapy with angiotensin-converting enzyme inhibitors, spironolactone, digoxin, and diuretics. These patients can present with symptoms of volume overload or low cardiac output in the absence of volume overload. Intermittent dobutamine infusion is commonly used in these patients for the relief of symptoms and to improve quality of life, despite the expected increased mortality. The quality of life of the survivors in the dobutamine-treated group 2 seemed to be better during the first 3 months of treatment, based on the tendency for a better functional status (mean NYHA classification: group 2, 2.8 [+ or -] 0.7 [13 patients]; group 1, 3.2 [+ or -] 0.9 [nine patients]) and on the number of patients who were able to undergo cardiopulmonary exercise testing (group 2, 9 of 13 survivors [70%]; group 1, 5 of 9 survivors [55%]). At 6 months of follow-up, only 4 patients were alive in group 1, and their quality of life seemed to be comparable to that of the 10 survivors in group 2. (25) In this study, treatment with intermittent dobutamine infusions in patients with severe heart failure who were receiving optimal medical treatment plus therapy with oral amiodarone was associated with a 57% relative reduction in death rate during the 1-year follow-up period and a 41% absolute reduction in mortality at 1 year. These findings imply that, for every 1,000 patients with end-stage heart failure, intermittent dobutamine infusions combined with oral amiodarone therapy could prevent an estimated 410 deaths annually. This treatment effect is commensurate with that of the implantation of an LV assist device, which has been estimated to prevent 270 deaths for every 1,000 patients who undergo its implantation. (21)
Dobutamine exerts a sustained therapeutic effect, lasting up to 10 weeks after a single 72-h continuous infusion in patients with CHF. (26) The management of CHF with long-term, weekly, 48-h dobutamine infusions produces significant and sustained hemodynamic and clinical improvements,16-19 although it does not prolong survival. (19) The increased death rate in patients treated with long-term, intermittent dobutamine infusions is most likely due to a proarrhythmic effect. (20,27)
In patients with severe CHF, treatment with amiodarone was associated with an early decrease in sudden death rate, and a late decrease in mortality due to progressive heart failure. (12) It is noteworthy that no study has shown a negative effect of amiodarone on survival. A meta-analysis of 13 randomized studies with amiodarone in patients with systolic LV dysfunction showed a 13% reduction of the risk of death. (28) This decrease in mortality by amiodarone has been attributed to its antiarrhythmic (12,29) and antiadrenergic properties. (30)
In this study, an 8-h dobutamine infusion was chosen, as it has been found to promote sustained improvements in LV function with minimal tachyphylaxis, (31) and is of sufficient duration to correct fluid retention, electrolyte abnormalities, and azotemia in patients with severe CHF. Although the sustained clinical and hemodynamic improvements that we noted may have been mulfifactorial, we believe that they are most likely attributable to dobutamine. Suggested beneficial dobutamine effects include a conditioning effect, (32) cellular changes in myocardial energetics and peripheral muscle, (33) an improvement in myocardial mitochondrial structure, an increase in the myocardial adenosine triphosphate/creatinine ratio, an increase in subendocardial blood flow, (34) and normalization of ventricular vascular coupling. (35)
The lower mortality rate that we observed is probably attributable to a synergistic effect of dobutamine and amiodarone. Whereas the intermittent dobutamine infusion administered to patients in group 2 is known to increase mortality, (9) we expected the salutary effect of amiodarone to be similar in both groups. The reduction in mortality rate associated with intermittent dobutamine infusions goes against the effect expected from the administration of this type of pharmaceutical. The possible explanations for this effect may be that (1) dobutamine improved or at least stabilized the patients hemodynamic and clinical status, and prevented deaths due to the progression of heart failure, and (2), while amiodarone has no affinity to [beta]-adrenergic receptors and does not a/feet basal or isoproterenol-induced intracellular cyclic adenosine monophosphate levels, it down-regulates the density of cardiac [beta]-adrenergic receptors acting as a triiodothyronine antagonist. (36,37) In addition, amiodarone suppressed spontaneous life-threatening arrhythmias, (12,29) as well as arrhythmias induced by dobutamine, (19) such that, by preventing the additional dobutamine-induced arrhythmic deaths, the net effect was a decrease in mortality related to hemodynamic and clinical improvement or stabilization. This hypothesis is supported by the similar proportions of sudden death relative to all deaths in both groups. Furthermore, these results are concordant with those of studies of combined enoximone and metoprolol administration in addition to standard medications, (10) and with the results of our previous nonrandomized study using intermittent dobutamine infusions combined with oral amiodarone. (11)
Study Limitations
The most important limitation of our study was the small number of patients in each subgroup. However, these favorable and impressive results have encouraged us to plan a larger randomized study. To recruit a larger number of patients, we intend to include NYHA class IV patients, as well as patients with less severe heart failure than those included in this study.
CONCLUSION
Our results suggest that long-term, intermittent dobutamine infusions combined with amiodarone therapy, in addition to standard therapy, improve the survival of patients with severe CHF. Furthermore, this study suggests that the combination of inotropic agents with antiadrenergic and powerful antiarrhythmic agents should be evaluated with respect to its effect on survival in CHF patients, as well as its effect on the natural history of heart failure.
REFERENCES
(1) Mosterd A, Cost B, Hoes AW, et al. The prognosis of heart failure in the general population: the Rotterdam Study. Eur Heart J 2001; 22:1318-1327
(2) Califf RM, Adams KF, McKenna WJ, et al. A randomized controlled trial of epoprostenol therapy for severe congestive heart failure: the Flolan International Randomized Survival Trial (FIRST). Am Heart J 1997; 134:44-54
(3) Massie BM, Shah NB. Evolving trends in the epidemiologic factors of heart failure: rationale for preventive strategies and comprehensive disease management, Am Heart J 1997; 133: 703-712
(4) Xamoterol in Severe Heart Failure Study Group. Xamoterol in severe heart failure. Lancet 1990; 336:1-6
(5) Packer M, Carver JR, Rodeheffer RJ, et al. Effect of oral milrinone on mortality in severe chronic heart failure. N Engl J Med 1991; 325:1468-1475
(6) Narahara KA. Oral enoximone therapy in chronic heart failure: a placebo-controlled randomized trial; The Western Enoximone Study Group. Am Heart J 1991; 121:1471-1479
(7) Feldman AM, Bristow MR, Parmley WW, et al. Effects of vesnarinone on morbidity and mortality in patients with heart failure. N Engl J Med 1993; 329:149-155
(8) The Digitalis Investigation Group. The effect of digoxin on mortality and morbidity in patients with heart failure. N Engl J Med 1997; 336:525-533
(9) Felker GM, O'Connor CM. Inotropic therapy for heart failure: an evidence-based approach. Am Heart J 2001; 142:393-401
(10) Shakar SF, Abraham WT, Gilbert EM, et al. Combined oral positive inotropic and beta-blocker therapy for treatment of refractory class 1V heart failure. J Am Coll Cardiol 1998; 31:1336-1340
(11) Nanas JN, Kontoyannis DA, Alexopoulos GP, et al. Long term intermittent dobutamine infusion combined with oral amiodarone improves the survival of patients with severe congestive heart failure. Chest 2001; 119:1173-1178
(12) Greene HL. The CASCADE Study: randomized antiarrhythmic drug therapy in survivors of cardiac arrest in Seattle: the CASCADE Investigators. Am J Cardiol 1993: 72:70F-74F
(13) Singh BN. Amiodarone: historical development and pharmacologic profile. Am Heart J 1983; 106:788-797
(14) Doval HC, Nul DR, Grancelli HO, et al. Randomised trial of low dose amiodarone in severe congestive heart failure: Grupo de Estudio de la Sobrevida en la Insuficiencia Cardiaca en Argentina (GESICA). Lancet 1994; 344:493-498
(15) Collins JA. Skidmore MA, Melvin DB, ct al. Home intravenous dobutamine therapy ill patients awaiting heart transplantation. J Heart Transplant 1990:9:205-208
(16) Gibelin P. Sbirrazzuoli V. Drici M, et al. Effects of short-term administration of dobutamine on left ventricular performance, exercise capacity, norepinephrine levels, and lymphocyte adrenergic receptor density in congestive heart failure. Cardiovasc Drugs Ther 1990; 4:1105-1112
(17) Miller LW. Outpatient dobutamine for refractory congestive heart failure: advantages, techniques, and results. J Heart Lung Transplant 1991; 10:482-487
(18) Krell MJ, Kline EM. Bates ER. et al. Intermittent, ambulatory dobutamine infusions ill patients with severe congestive heart failure. Am Heart J 1986; 112:787-791
(19) Dies F, Krell MJ, Whitlow 19, et al. Intermittent dobutamine in ambulatory outpatients with chronic cardiac failure [abstract]. Circulation 1986; 74:II-38
(20) Tisdale JE, Patel R, Webb CB, et al. Electrophysiologic and proarrhythmic effects of intravenous inotropic agents. Prog Cardiovase Dis 1995:38:167-180
(21) Rose EA. Gelijns AC. Muskowitz AJ, et al, Long term use of a left ventricular assist device for end-stage heart failure: the Randomized Evaluation of Mechanical Assistance for the Treatment of Congestive Heart Failure (REMATCH) study group, N Engl J Med 2001; 345:1435-1443
(22) Massie BM, Fisher SG, Deedwania PC, et al. Effect of amiodarone on clinical status and left ventricular function in patients with congestive heart failure. Circulation 1996; 93: 2128-2134
(23) Packer M, Coats AJS, Fowler MB, et al. Effect of carvedilol on survival in severe chronic heart. failure. N Engl J Med 2001; 344:1651-1658
(24) Mancini DM, Eisen H, Kussmaul W, et al. Value of peak exercise oxygen consumption for optimal timing of cardiac transplantation in ambulatory patients with heart failure. Circulation 1991; 83:778-786
(25) Young JB, Moon EK. Outpatient parenteral inotropic therapy for advanced heart failure. J Heart Lung Transplant 2000; 19:S49-S57
(26) Liang CS, Sherman LG, Doherty JU, et al. Sustained improvement of cardiac function in patients with congestive heart failure after short-term infusion of dobutamine. Circulation 1984; 69:113-119
(27) John RM, Taggart PI, Sutton PM, et al. Direct effect of dobutamine on action potential duration in ischemic compared with normal areas in the human ventricle. J Am Coll Cardiol 1992; 20:896-903
(28) Amiodarone Trials Meta-Analysis Invetigators. Effect of prophylactic amiodarone on mortality after acute myiocardial infarction and in congestive heart failure: meta analysis of individual data from 6500 patients in randomized trials. Lancet 1997; 350:1417-1424
(29) Kudenchuk PJ, Cobb LA, Copass MK, et al. Amiodarone for resuscitation after out-of-hospital cardiac arrest due to ventricular fibrillation. N Engl J Med 1999:341:871-878
(30) Haikerwal D, Dart AM, Little PJ. et al. Identification of a novel, inhibitory action of amiodarone on vesicular monamine transport. J Pharmacol Exp Ther 1999; 288:834-837
(31) Unverferth DV, Magorien RD, Lewis RP, et al. Long term benefit of dobutamine ill patients with congestive cardiomyopathy. Am Heart J 1980; 1000:622-630
(32) Adamopoulos S, Piepuli M, Qiang F, et al. Effects of pulsed [beta]-stimulant theraphy on [beta]-adrenoceptors and chronotropic responsiveness in chronic heart failure. Lancet 1995; 345: 344-349
(33) Leier CV, Binkle PF, Parenteral inotropic support for advanced congestive heart failure. Prog Cardiovasc Dis 1998; 41:207-224
(34) Unverferth DV, Magorien RD, Altshuld B. et al. The hemodynamic and metabolic advantages gained by a three-day infusion of dobutamine in patients with congestive cardiomyopathy. Am Heart J 1983; 106:29-34
(35) Binkley PF, Van Fossen DB, Nunziata E, et al. Influence of positive inotropic therapy on pulsatile hydraulic, loa0d and ventricular-vascular coupling in congestive heart failure. J Am Coll Cardiol 1990; 15:1127-1135
(36) Drvota V, Haggblad J, Blanger I, et al. The effect of amiodarone on the b-adrenergic receptor is due to a downregulation of receptor protein and not to a receptor-ligand interaction. Biochem Biophys Res Commun 1999; 225:515-520
(37) Hartong R, Wiersing WW, Plomp TA. Amiodarone reduces the effect of [T.sub.3] on beta adrenergic receptor in rat heart. Horn Metab Res 1990; 22:85-89
* From the University of Athens School of Medicine, Department of Clinical Therapeutics, "Alexandra" Hospital Athens, Greece. Manuscript received May 16, 2003; revision accepted September 25, 2003.
Reproduction of this article is prohibited without written permission from the, American College of Chest Physicians (e-mail: permissions@chestnet.org).
Correspondence to: John N. Nanas, MD, Makedonias 24, 104 33 Athens, Greece; e-mail: jnanas@ath.forthnet.gr
COPYRIGHT 2004 American College of Chest Physicians
COPYRIGHT 2004 Gale Group