* The historical perspective of pharmacogenetics is presented to a large extent from a personal view, since I happened to get into this field of science at the time of its beginning, and since pharmacogenetics has remained the backbone of my scientific career. Pharmacogenetics initially emphasized observations of interpersonal variability, but the attention on interethnic differences soon followed. Technical advances led to the identification of many responsible gene alterations in both individuals and in populations. Included is a relatively extensive discussion in which the effects and the different consequences of monogenic (mendelian) and multigenic (multifactorial) variation are compared.
(Arch Pathol Lab Med. 2001;125:77-80)
In the early 1950s in Toronto, Ontario, I found a genetic variant of the enzyme then called pseudocholinesterase, now called butyryl-cholinesterase.1 This finding was clinically important because this enzyme was responsible for the normally short action of the muscle relaxant succinylcholine, then very frequently used during general anesthesia. It was this finding that established my interest in pharmacogenetics, soon fortified by an article by Motulsky.2
I was, therefore, much aware of the story of primaquine sensitivity. Primaquine was an antimalarial drug given during the World War II to American soldiers who served in malaria-infested areas. Some soldiers who took this drug developed a hemolytic disease; the remarkable fact was that virtually only black soldiers developed this disease. After the war, this hemolytic disease was thoroughly investigated in Chicago, Ill.3 It was found that the occurrence was based on a fault of the red blood cells; only red blood cells with this fault were destroyed by primaquine. Later, it was discovered that the fault was based on genetic variation of the enzyme glucose-6-phosphate dehydrogenase. The explanation for the interethnic difference was provided by Motulsky.4 The enzyme variant protected the carrier from infection with malaria and therefore occurred mainly in populations that came from countries in which malaria was prominent. This was the first clear-cut case of a drug-related genetic variant with a major difference in interethnic occurrence.
Another pharmacogenetic discovery in the early 1950s was that of a faulty metabolism of the antituberculosis drug isoniazid.5 Soon it was known that the frequency of this metabolic fault differed much between the world's populations.6 Today, the reason for this interethnic variability is still unknown; an influence of geographical latitude and climate is suspected, perhaps via geographical differences in the amounts and kinds of food.
The practical importance and widespread occurrence of such interethnic differences dawned on me after some research experiences in our laboratory. My colleagues and I started to investigate the metabolism of amobarbital, a sleeping pill of the barbiturate class widely used at that time.7 It turned out that one of our female students did not have in her urine the one breakdown product, a metabolite, that we and all the other investigated students had. We got permission to investigate the family members of the student, and it turned out that her brother and mother also did not produce this metabolite; we had discovered a new pharmacogenetic deficiency.8
We sought to learn whether this deficiency was a rare or common occurrence. We asked a colleague to get us more volunteers for this study from a class of medical students. One hundred forty students volunteered and all were tested. We were surprised to see that 7 of these students had more of this questioned amobarbital metabolite in their urine than what we considered normal. We wondered whether we had made some mistake in our measurements, and we asked the colleague whether we could retest these students. We gave him the student numbers that we had for their identification; a short time later, he came back, visibly shaken. All the numbers that we had given him were from the Chinese students in this class. Could it be that there was an ethnic difference in the metabolism of amobarbital? Our retest gave the same result as before; the measurements had not been mistaken.9 We had found a new interethnic difference of drug metabolism.
At about the same time, an inborn defect of the metabolism of a drug called debrisoquine was found in England' and of the drug sparteine in Germany." Our laboratory,12 like a Swedish laboratory,13 compared these 2 defects in some people. It turned out that both observations pointed to the deficiency of the same human liver enzyme, now called CYP2D6. Having established the methods for this investigation, we decided to use the method also to compare students of European and Chinese descent for the metabolism of these drugs. Again, there was clear evidence of a metabolic difference in drug metabolism between these 2 ethnic populations. I became excited with this observation and published an article on interethnic differences of drug metabolism,14 the first article of its kind, combining our data with those of older investigations. During the past few years, Swedish investigators published the genetic data that account for the metabolic difference of CYP2D6 between Chinese and white people.
THE CHANGE FROM PHENOTYPING TO GENOTYPING
One tends to forget how dramatic has been the change from the time genetics depended on family studies until more recently when molecular genetics allowed the investigation of DNA sequences. This change of the science of genetics has also much affected pharmacogenetics. Particularly, differences in drug response between ethnic populations were in the past often called cross-cultural, especially by psychiatrists, who could not get themselves to believe in a genetic cause of the observed differences.
Until recent times, we could not imagine the magnitude of the gene variations that confronted us. Humans have approximately 3 billion base pairs of nucleic acids, and about every 1 in 1000 or more are variant's in the form of single nucleotide polymorphisms. There are more than 100 cancer-producing oncogenes and a few dozen cancer-- suppressing genes, and their functions may be controlled by genes determining DNA repair, cell division, metabolism, immune responses, embryonic development, and cell migration.16 Many of these controlling genes show variation. It is not surprising that many genes that control drug responses are variable; the existence of pharmacogenetics is not surprising.
The decades-old biochemical methods for the study of genes are currently being replaced by methods serving the new science of genomics.17 The structure of a genome is much more than a simple accumulation of genes, and it promises many new insights. It is not surprising that pharmacogenetics is gradually extended to include some new expectations, thereby becoming pharmacogenomics.18,19
THE SCIENCE OF HUMAN POPULATIONS
Old investigations referred to human populations as white, black, or yellow entities. Later, distinctions were often made on the basis of geography, language, and anthropology; the descriptive term ethnography was meant to indicate science but did not prevent bias. The situation changed with the introduction of genetic investigations, summarized and much enhanced by Cavalli-Sforza et al.20 They reported extensive studies of 42 populations and large enough numbers of subjects to get frequencies of 120 genetic polymorphisms. They summarized the data in terms of 9 clusters, which included New Guineans, Pacific Islanders, Southeast and Northeast Asians, Amerindians, Europeans, other Caucasoids, and Africans; they assigned comparative genetic distance data to these populations. The biggest difference was between Africans and all other populations, allowing an estimated time division of about 150 000 years that human populations emigrated from Africa. For comparison, the division between Northeast Asians and Europeans occurred approximately 40 000 years ago.
Thus, there are many genetic variants that occur with different frequencies in these populations. Therefore, the observation of pharmacogenetic differences between human populations is to be expected and is not a surprising phenomenon.21
MONOGENIC VERSUS MULTIFACTORIAL VARIATION
It has been known for a long time that there are 2 kinds of genetic variation that may be distinguished by the terms monogenic (mendelian) or multigenic (alternatively and perhaps better called multifactorial). So far, most studies of pharmacogenetics have dealt with monogenic, structural variations of drug-metabolizing enzymes. A number of examples were provided in the introduction; let me broaden this outlook.
MONOGENIC VARIATION AND TRADITIONAL PHARMACOGENETICS
There are many variable cytochrome P-450s, a major group of enzymes metabolizing drugs and endogenous chemicals. For instance, CYP2A6 is responsible for the main metabolism of nicotine,2 and CYP2C19 is responsible for mephenytoin metabolism.23 The cytochrome CYP2D6 deserves some special considerations. For instance, in Spain there are more persons than elsewhere in Europe with very high CYP2D6 activity, resulting from gene duplication and admixture with North African populations in whom this duplication is frequent. Furthermore, the CYP2D6 gene is known to harbor more than 48 mutations,24 which, through duplications, account for 50 variant forms of the enzyme. Only one of these, the G>C variant at location 4268 occurs in all populations; many others occur only in Europe, Asia, China, or Africa.25 The explanation must be that the G>C variant found in all populations is the oldest, representing a mutation that has occurred before humans divided into different groups. All other variants must have occurred later, after the separation and division of humanity into different ethnic populations. Different times of mutation will probably explain many interethnic differences between drug-metabolizing enzymes.
I will herein discuss only briefly drug receptors and transporters. There are various kinds of receptors, for instance, nuclear receptors such as the aromatic hydrocarbon receptor or the G protein-coupled receptors with 7 transmembrane loops.26 There are more than 1000 of this latter kind, accounting for more than 1% of the human genome. In view of these large numbers, our ignorance of receptor variation is striking; reasons for this ignorance are at least in part the need for special analytical or technical methods. To investigate the genetics of a receptor in the brain, for example, one first needs to know the DNA sequence of its gene; one can then look for DNA variants of this gene in white blood cells or other accessible materials. To find out whether a given change of the gene is clinically significant, it usually requires the use of statistical or epidemiological methods. As a result of these difficulties, our knowledge of most receptor variations is limited, particularly in relation to drug responses. However, for example, it has been claimed that some variations of the dopamine D4 27 or the serotonin 5-HT2C receptor 28 are responsible for the nonresponse to clozapine of some schizophrenic patients.
Transporters have been investigated even less than receptors. There are important data on the variability of the transporter P-glycoprotein. This transporter protects cell membranes. A variant has been responsible for the therapeutic failure of anticancer drugs.29
MULTIFACTORIAL VARIATION AND A PHARMACOGENETIC CONCERN
Most differences between people are represented by differences between many genes, and these differences may be enhanced by innumerable environmental factors. In pharmacology, the ever-present differences in drug response have been recognized by introduction of the concept the effective dose for 50% of any population of humans or animals.311 It means a dose large enough to be effective in half the population, too low for the other half. It was this concept that converted pharmacology from an observational discipline into a science.
Let us consider the metabolism of a drug. As described herein, the metabolism may fail because the enzyme is not formed, structurally altered, or not functional because of the presence of a (perhaps unknown) inhibitor. It may be poorly formed because of a missing hormonal inducer. It may be degraded too fast. The drug may not be able to reach the intracellular enzyme. Thus, even a single event such as drug metabolism may represent a complexity.
In addition, the response to a given dose of a drug may depend on drug absorption, drug distribution in body fat, drug binding to proteins, drug transport, blood flow, target reaction, or elimination via kidney, bile, or gut. We can be certain that each of these factors is controlled by one or more genes. Multifactorial variation of the drug's fate, or of the response to it, is important. Because of these complexities, we usually do not care for the reasons of a difference in drug response between individuals.
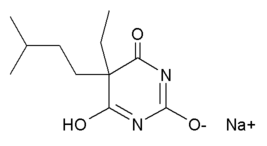
This lack of interest may be unwarranted if a drug response that appears to be multifactorial is different not only between individuals but also between populations. For example, the apparently multifactorial glucuronidation of codeine differs systematically between Swedish and Chinese subjects.31 It may lead to an erroneous conclusion if, in such cases, one simply compares the means (or averages) plus their SDs in these populations. One problem is illustrated in the Figure.32
Each curve indicates the person-to-person variation of the clearance of some drug; in people with slow clearance the drug may produce an adverse effect, particularly after repeated drug administration. The 2 curves indicate the clearance variations in 2 populations; the means are 1 SD apart. There is much overlap between the individual values of the 2 curves, and the difference between the means may register as statistically not significant. The arrow indicates the clearance rate, below which the drug causes toxic effects; thus, 2% of population A and 16% of population B must be assumed to experience toxic effects, an eightfold difference. This toxicity ratio would become larger the more the arrow is moved to the left edge; this edge effect is not reflected by the difference between the means of the curves.
In any case, the interpretation of a multifactorial difference between pharmacological data requires caution, and a simple statistical comparison of the 2 means may provide inadequate biological information.
CAN INTERETHNIC FREQUENCY DIFFERENCES OF ENZYME VARIANTS BE QUALIFIED?
Pharmacogenetic differences between populations are of 2 possible kinds. First, it is an almost universal observation that the frequency of a mutant is found to differ between populations. Second, there are often different mutants in different populations, as I have shown with the example of CYP2D6 variations.
I counted 40 drug-metabolizing enzymes known to show pharmacogenetic variation within one or more white populations. Of these, 30 are known to have at least one interethnic difference of variant frequency. In many or most cases for which no interethnic difference is entered, such difference has not yet been searched for; the glucuronosyl transferases are clear-cut examples, because their genetic variants are relatively new observations. The compared populations were usually European and Asian, sometimes African. In any case, it can be said with assurance that in at least three fourths of all cases, interindividual differences of drug-metabolizing enzymes are paralleled by interethnic differences.
CONCLUDING THOUGHTS
Pharmacogenetics represents only one of many genetic responses to environmental hazards.33 Human variation in pharmacogenetics is similar to human variation in response to foods. For instance, the normal salt intake in Western countries causes members of populations who come from salt-poor areas to develop cardiovascular disease. Populations adjusted to frequent periods of starvation tend to show a high incidence of type 2 diabetes mellitus. Very interesting are the different genetic mechanism to fight infections; acquired immunodeficiency syndrome resistance has been explained in whites but not yet in Africans, where the resistance must be of a different kind.34 At least some of the genetic mechanisms that allow people to thrive in hot or cold climates are known.
Pharmacogenetic variation can be looked at as a feature that can protect populations by providing them with genetic diversity; pharmacogenetic variation is usually immaterial for any affected individual unless a drug or toxicant is present. For instance, resistance of an individual insect to the killing effect of an insecticide may cause this individual to survive an exposure, allowing it to reproduce and in the long run to create the resistant strain; in the absence of the poison, the existence of the resistant individual simply represents population diversity. Bacterial resistance to antibiotics represents the same mecha-- nism. We cannot see this dramatic effect of pharmacogenetics in people, because environmental hazards usually do not have a fatal impact on the general population and the human generation time is too long.
I hope that the look at pharmacogenetic variation in this broad perspective is useful. It should help us to understand the genetic differences that affect both human individuals and human populations.
References
1. Kalow W. Familial incidence of low pseudocholinesterase level. Lancet. 1956;2:576-577.
2. Motulsky A. Drug reactions, enzymes, and biochemical genetics. JAMA. 1957;165:835-837.
3. Dern RJ, Beutler E, Alving AS. The hemolytic effect of primaquine. J Lab Clin Med. 1954;44:171-176.
4. Motulsky AG. Metabolic polymorphisms and the role of infectious diseases in human evolution. Hum Biol. 1960;32:28.
5. Bonicke R, Lisboa BP. Ober die Erbbeddingtheit der intraindividuellen Konstanz der Isoniazidausscheidung beim Menschen. Naturwissenschaften. 1957;44: 314.
6. Sunahara S, Urano M, Ogawa M. Genetical and geographical studies on isoniazid inactivation. Science. 1961;134:1530-1531.
7. Tang BK, Inaba T, Kalow W. Amobarbital metabolism in man: determination of N-hydroxyamobarbital and 3'-hydroxylation of amobarbital in urine by gas chromatography chemical ionization mass spectrometry. Biomed Mass Spectrometry. 1977;4:73-76.
8. Kalow W, Kadar D, Inaba T, Tang BK. A case of deficiency of N-hydroxylation of amobarbital. Clin Pharmacol Ther. 1977;21:530-535.
9. Kalow W, Tang BK, Kadar D, Endrenyi L, Chan F-Y. A method to study drug metabolism in populations: racial differences in amobarbital metabolism. Clin Pharmacol Ther. 1979;6:766-776.
10. Mahgoub A, Idle JR, Dring LG, Lancaster R, Smith RL. Polymorphic hydroxylation of debrisoquine in man. Lancet. 1977;2:584-586.
11. Eichelbaum M, Spannbrucker N, Steinke B, Dengler HJ. Defective N-oxidation of sparteine in man: a new pharmacogenetic defect. Eur] Clin Pharmacol. 1979;16:183-187.
12. Kalow W, Otton SV, Kadar D, Endrenyi L, Inaba T. Ethnic difference in drug metabolism: debrisoquine 4-hydroxylation in Caucasians and Orientals. Can Physiol Pharmacol. 1980;58:1142-1144.
13. Bertilsson L, Dengler HG, Eichelbaum M, Schulz H-U. Pharmaco-genetic
covariation of defective N-oxidation of sparteine and 4-hydroxylation of debrisoquine. EurJ Clin Pharmacol. 1980;17:153-155.
14. Kalow W. Ethnic differences in drug metabolism. Clin Pharmacokinet. 1982;7:373-400.
15. Pennisi E. Using the wildly popular genome markers called SNPs to track genes may be less straightforward than researchers expected: a closer look at SNPs suggests difficulties. Science. 1998;281:1787-1789.
16. Garber K. More SNPs on the way: genome research. Science. 1998;281: 1788.
17. Collins FS. Genetics: an explosion of knowledge is transforming clinical practice. Geriatrics. 1999;54:41-47.
18. Baily DS, Bondar A, Furness LM. Pharmacogenomics: it's not just pharmacogenetics. Curr Opin Biotechnol. 1998;9:595-601.
19. Marshall A. Laying the foundations for personalized medicine. Nat Biotechnol. 2000;15:954-957.
20. Cavalli-Sforza LL, Menozzi P, Piazza A. The History and Geography of Human Genes. Princeton, NJ: Princeton University Press; 1994.
21. Kalow W. Pharmacoanthropology and the genetics of drug metabolism. In: Kalow W, ed. International Encyclopedia of Pharmacology and Therapeutics: Pharmacogenetics of Drug Metabolism. Oxford, NY: Pergamon Press Inc; 1992: 865-877.
22. Pianezza ML, Sellers EM, Tyndale RF. Nicotine metabolism defect reduces smoking. Nature. 1998;393:750.
23. Daniel HI, Edeki TI. Genetic polymorphism of S-mephenytoin 4-hydroxylation. Psychopharmacol Bull. 1996;32:219-130.
24. Marez D, Legrand M, Sabbagh N, et al. Polymorphism of the cytochrome P450 CYP2D6 gene in a European population: characterization of 48 mutations and 53 alleles, their frequencies and evolution. Pharmacogenetics. 1996;7:193202.
25. Daly AK, Brockmoller J, Broly F, et al. Nomenclature for human CYP2D6 alleles. Pharmacogenetics. 1996;6:193-201.
26. Kenakin T. The classification of seven transmembrane receptors in recombinant expression systems. Pharmacol Rev. 1996;48:413-451.
27. Van Tol HHM. Structural and functional characteristics of the dopamine D4 receptor. Adv Pharmacol. 1998;42:1054-3589.
28. Masellis M, Basile V, Meltzer HY, et al. Serotonin subtype 2 receptor genes and clinical response to clozapine in schizophrenia patients. Neuropsychopharmacology. 1998;19:123-132.
29. Izquierdo MA, Shoemaker RH, Flens MJ, et al. Overlapping phenotypes of multidrug resistance among panels of human cancer-cell lines. Int] Cancer. 1996;65:230-237.
30. Trevan JW. The error of determination of toxicity. Proc R Soc London B. 1927;101:483-515.
31. Yue Q-Y, Sawe J. Interindividual and interethnic differences in codeine metabolism. In: Kalow W, ed. Pharmacogenetics of Drug Metabolism. New York, NY: Pergamon Press Inc; 1992:721-727.
32. Kalow W, Bertilsson L. Interethnic factors affecting drug response. Adv Drug Res. 1994;25:1-59.
33. Kalow W. Pharmacogenetics in biological perspective. Pharmacol Rev. 1997;49:369-379.
34. Samson M, Libert F, Doranz BJ, et al. Resistance to HIV-1 infection in Caucasian individuals bearing mutant alleles of the CCR-5 chemokine receptor gene. Nature. 1996;382:722-723.
Werner Kalow, MD
Accepted for publication August 16, 2000.
From the Department of Pharmacology, University of Toronto,Toronto, Ontario.
Presented at the Ninth Annual William Beaumont Hospital DNA Technology Symposium, DNA Technology in the Clinical Laboratory, Royal Oak, Mich, April 13-15, 2000.
Reprints: Werner Kalow, MD, Department of Pharmacology, Medical Sciences Bldg, University of Toronto, Toronto, Ontario M5S 1A8, Canada (e-mail: w.kalow@utoronto.ca).
Copyright College of American Pathologists Jan 2001
Provided by ProQuest Information and Learning Company. All rights Reserved