Sponsored by: EORTC International Antimicrobial Therapy Group
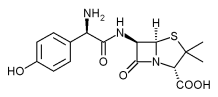
RATIONALE: Antibiotics such as amoxicillin, ciprofloxacin, and moxifloxacin may be effective in preventing or controlling fever and neutropenia in patients with cancer. It is not yet known whether moxifloxacin alone is more effective than amoxicillin combined with ciprofloxacin in treating neutropenia and fever.
PURPOSE: Randomized clinical trial to compare the effectiveness of moxifloxacin with that of ciprofloxacin combined with amoxicillin in treating neutropenia and fever in patients who have cancer.
Study Type: Interventional
Study Design: Treatment
OBJECTIVES:
* Compare the rates of successful response to moxifloxacin vs. ciprofloxacin in combination with amoxicillin-clavulanate potassium in low-risk febrile neutropenia patients with cancer.
* Compare the time to discharge, time to discontinuation of any antimicrobial therapy, and time to defervescence of patients treated with these regimens.
* Compare 28-day survival of patients treated with these regimens.
* Determine the proportion of these patients who are eligible for oral therapy and a therapeutic management including intention of early discharge.
* Determine the medical and nonmedical reasons for continued in-hospital observation and care or for readmission of these patients.
* Determine the accuracy of the physician's estimate of further neutropenia duration and evaluate its predictive value in these patients.
* Validate the Multinational Association for Supportive Care in Cancer low-risk prediction rule to predict the absence of serious medical complications in the setting of oral therapy in in- and outpatients.
OUTLINE: This is a double-blind, randomized, multicenter study. Patients are stratified according to institution, underlying disease (hematologic malignancy vs. other), pretreatment with no more than a single dose (yes vs. no), and outpatient status at fever onset (yes vs. no). Patients are randomized into 1 of 2 treatment arms.
* Arm I: Patients receive oral moxifloxacin once daily. Patients also receive oral ciprofloxacin placebo and oral amoxicillinclavulanate potassium placebo twice daily.
* Arm II: Patients receive oral ciprofloxacin and oral amoxicillin-clavulanate potassium twice daily. Patients also receive oral moxifloxacin placebo once daily. Patients with fever classified as not related to infection (i.e., doubtful) stop antibiotic therapy on day 3. All other patients receive antibiotics until complete resolution of infection or until failure is determined or anticipated, for up to 28 days.
* Patients are followed at 7-10 days.
Ages eligible for study: 18 years and above, both genders
Inclusion Criteria:
* Diagnosis of cancer with developing febrile neutropenia
* Neutropenia defined as an absolute granulocyte count of less than 1,000/[mm.sup.3], expected to fall to less than 500/[mm.sup.3] within 24 hours, secondary to administration of chemotherapy and/or radiotherapy within the past 30 days
* Fever defined as an oral temperature greater than 38.5[degrees]C once, or 38[degrees]C or greater on 2 or more occasions at least 1 hour apart during a 12-hour period, and suspected to be due to infection
* Expected low risk of serious medical complications as predicted by a Multinational Association for Supportive Care in Cancer risk-index score of greater than 20
* No obvious signs of exit-site or tunnel intravascular catheter infection
* No known or suspected CNS infection
* No known or highly suspected bacterial, viral, or fungal infection
Patient Characteristics:
Life expectancy
* No high probability of death within 48 hours before study enrollment (i.e., patients who are moribund or comatose for any reason with little hope of recovery OR patients in danger of or in hepatic stupor or coma)
Hematopoietic
* No signs or symptoms of uncontrolled bleeding
Hepatic
* Bilirubin no greater than 3 times upper limit of normal (ULN)
* Alkaline phosphatase no greater than 3 times ULN
* AST and ALT no greater than 5 times ULN
* No severe hepatic dysfunction
Renal
* Creatinine no greater than 3.4 mg/dL
* Creatinine clearance at least 25 mL/min
* No renal failure requiring hemodialysis or peritoneal dialysis
Cardiovascular
* No prior symptomatic arrhythmias
* No clinically relevant bradycardia
* No QTc interval prolongation
* No uncorrected hypokalemia
* No signs or symptoms of hypotension (systolic less than 90 mm Hg)
Pulmonary
* No signs or symptoms of respiratory insufficiency
Other
* Not pregnant or nursing
* Fertile patients must use effective contraception
* Able to swallow oral medication
* No contraindication for oral drug intake
* No condition likely to severely impair drug absorption
* No prior immediate or accelerated reaction to penicillin, cephalosporin, or fluoroquinolone antibiotics
* No known allergy or hypersensitivity to any antibiotics in this study or other quinolones
* No signs or symptoms of severe dehydration
* No signs or symptoms of shock
* No other signs or symptoms at presentation that would necessitate IV supportive therapy
* More than 4 days since prior antibacterial agents except for the following:
* A single (oral or parenteral therapeutic) dose after initial diagnostic work-up and within the last 8 hours
* Low-dose cotrimoxazole (i.e., no more than 480 mg daily or 960 mg 3 times per week) prophylaxis of Pneumocystis carinii pneumonia
* More than 30 days since prior investigational drugs
* No prior randomization in this study
* No other concurrent antimicrobial agents
* No class IA or class III antiarrhythmic drugs or other concurrent drugs that prolong the QTc interval
Location and Contact Information
Klinikum der Albert-Ludwigs-Universitaet Freiburg, Freiburg, D-79106, Germany; Winfried Kern, MD Study Chair Tel: 49-761-270-1818
Germany
A total of 530 patients (265 patients per treatment arm) will be accrued for this study within approximately 2 years.
Study ID Numbers CDR0000304631; EORTC-46001
NLM Identifier NCT00062231
COPYRIGHT 2003 Journal of Drugs in Dermatology
COPYRIGHT 2003 Gale Group