This deadly cardiac condition requires rapid identification and immediate medical intervention.
Abstract: Patient survival of aortic dis section hinges on timely diagnosis and treatment. [Nurs Manage 2004:35(2):25-33]
Fifty-year-old Ted Burns presents to the emergency department complaining of excruciating chest pain that radiates to his back. he informs the triage nurse that the pain came on suddenly and that it feels like he's being "ripped in half." Burns is extremely anxious, diaphoretic, pale, tachycardie, and hypertensive.
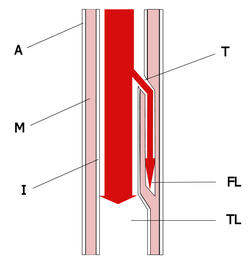
You'll need to act fast because Burns could be experiencing an acute aortic dissection-a tear in the lining (intima) of the aorta followed by bleeding and hematoma formation.1 Blood, driven by the force of arterial pressure, can cause separation of or delamination between the layers of the aorta, thus creating a new channel or false lumen in the aortic wall.
Unlike aortic aneurysms, aortic dissections usually occur suddenly and without evidence of previous vessel dilatation. The condition is life threatening: The likelihood of death within the first 48 hours is 1% per hour for those left untreated, with a three-month mortality as high as 90%.2 Aortic dissection requires prompt recognition for a successful outcome. There can be many presentations in aortic dissection that mimic other conditions, thus confusing the clinical picture. And unfortunately, 65% of all aortic dissections are initially misdiagnosed.
Perhaps the single most important factor leading to a successful outcome is a high index of suspicion on the part of the examining clinician. Increased awareness, blood pressure control, and basic imaging are essential for accurate and swift diagnosis.
Aortic dissection occurs in approximately two of every 10,000 people. The incidence may be greater, but it's difficult to pinpoint due to the high mortality rate and misdiagnosis associated with the condition. In fact, evidence of aortic dissection is found in 1% to 3% of all autopsies.3 Although it strikes both sexes, it's three times more common in men, with a higher rate of occurance among African-Americans and a lower rate among Asians. Approximately 75% of aortic dissections occur in people ages 40 to 70.4
Pathogenesis/anatomy
The exact cause of aortic dissection remains unknown, but predisposing factors include atherosclerosis and hypertension. Most dissections occur due to deterioration of the aortic wall secondary to chronic stress, usually attributed to longstanding hypertension.5
A history of hypertension is reported in the majority of dissection cases. Over time, hypertension causes an increased strain on the aorta; consequently, if the wall of the aorta is vulnerable, a tear or dissection can occur.
Aortic dissection is also associated with certain rare genetic connective tissue disorders, such as Marfan and Ehlers-Danlos syndromes. Faulty connective tissue causes the wall of the aorta to weaken and stretch, a process called aortic dilatation. This dilatation can progress to dissection. Frequently, a flaw in the aortic valve is also present. Aortic dissection is the primary cause of premature death in individuals with Marfan syndrome.6
Aortic insufficiency, also called regurgitation, occurs in more than half of aortic dissections. When present, the aortic valve won't close tightly, leading to a backward flow of blood from the aorta into the left ventricle and, ultimately, causing heart failure.
Aortic dissection is also linked to blunt trauma. A blow to the aorta can cause a tear with subsequent bleeding and dissection. Presentation to the emergency room with a conscious victim frequently elicits complaints of severe chest pain. A chest X-ray usually confirms a widened mediastinum and the need for further diagnostic imaging.
Aortic dissection is also associated with pregnancy. More than half of all dissections in women under the age of 40 occur during pregnancy, with the peak incidence during the third trimester. A dissection during pregnancy is caused by the increased production of hormones that work on smooth muscle and connective tissue for normal uterine growth. In addition to hormonal changes, a pregnant individual's blood volume increases by half during the third trimester, placing more strain on the aorta.7
Certain congenital cardiac anomalies, such as coarctation of the aorta or bicuspid aortic valve, can also predispose an individual to dissection. Coarctation of the aorta is characterized by a narrowing in the descending aorta, most commonly beyond the subclavian arteries. It occurs in one of every 10,000 people.8
Regarding the bicuspid aortic valve, it's important to understand that normally the aortic valve has three leaflets or cusps that control the flow of blood into the aorta. A bicuspid valve, present in 1% to 2% of the population, has only two leaflets or cusps and can hamper the way in which the valve opens and closes, leading to dilatation of the aortic root attributed to ineffective opening and closing (stenosis or insufficiency).9
Aortic dissection is also a rare but potential complication of both cardiac surgery and cardiac catheterization. Dissection of the thoracic aorta is also attributed to illicit drug use; cocaine inhalation can produce acute aortic damage, such as frank rupture or acute aortic dissection. The relationship between methamphetamine usage and aortic dissection is most likely due to the drug's hypertensive effect.10
Condition classifications
Dr. Michael DeBakey performed the first successful surgical repair of aortic dissection in 1955. DeBakey developed classifications for aortic dissection in 1964 that the health care community still uses. DeBakey's classification system is based on the fact that more than 95% of all dissections arise in either the ascending aorta (within centimeters of the aortic valve) or the descending thoracic aorta, usually beyond the origin of the left subclavian artery.11
The Stanford version, a simplified hybrid of DeBakey's classification system, is widely used and has become the standard for treatment strategy. Type A dissection receives surgical intervention; type B dissection receives medical therapy.12 (See "Where's the tear?")
Dissection is usually bi-directional, moving proximally toward the heart and distally into the descending aorta or toward the lower extremities.13 The dissection can progress quickly to the abdominal aorta, and the renal, iliac, or femoral arteries. Complete or partial occlusion of the arteries arising from the aortic arch or lumbar region may lead to myocardial infarction, stroke, or paralysis. Depending on the location of the dissection and the branches of arteries involved, vital organs may be compromised, adding to the devastation and diminishing an individual's survival prospect. Spontaneous rupture may result in sudden death.
Signs and symptoms
The path the dissection takes as it progresses along the aorta generally determines clinical manifestations.14 The most consistent symptom is the sudden onset of excruciating pain, often described as a "tearing" or "ripping" sensation. The pain usually isn't relieved with analgesics and its location may actually indicate the site of dissection. Aortic dissection is painless in only 10% of patients.
Dissection of the ascending aorta is usually associated with anterior chest pain, whereas dissection of the descending aorta is typically associated with back pain. As the dissection spreads, the pain migrates to the involved area.
In the early stages of dissection, the patient's blood pressure is usually elevated. he or she typically presents looking "shocky," but is hypertensive. Hypotension is usually an ominous sign and may represent cardiac tamponade.
Neurologic deficits occur in 20% of patients with aortic dissection, most presenting with syncope and altered mental status.15 Nearly 40% of patients have changes on their electrocardiogram suggesting ischemia. If a dissection of the aortic root occurs, it jeopardizes the coronary arteries. The patient may show signs and symptoms of acute myocardial infarction, which often confuses the clinical picture because the patient may be experiencing an acute infarction but the cause is secondary to the dissection. If you suspect aortic dis section, withhold all thrombolytics. Intra-aortic balloon pump insertion is contraindicated in the presence of aortic dissection.
When the dissection advances to the renal arteries, renal function becomes impaired. The patient may have elevated blood urea nitrogen and creatinine levels with decreased urinary output. If the dissection involves the femoral arteries, the patient will present with diminished or absent pulses and possible limb ischemia. Actual dissection or compression of the vessel due to hematoma formation may impact pulses in any extremity.16 Symptoms will appear as the dissection progresses; therefore, it's important to assess the patient thoroughly and frequently for any changes in his or her condition.
Diagnosis and evaluation
In 2001, the European Society of Cardiology developed diagnosis, management, and treatment guidelines for aortic dissection. The guidelines stress initial management for those with suspected aortic dissection, including:
* detailed history and physical whenever possible
* electrocardiogram
* laboratory testing: complete blood count, basic metabolic profile, rnyoglobin, D-dimer, creatine kinase, troponin, lactate dehydrogenase
* heart rate and blood pressure monitoring
* pain relief (morphine sulfate)
* reduction of systolic blood pressure using beta-blockers (intravenous propranolol, metoprolol, esmolol, or labetalol)
* transfer to intensive care unit
* additional vasodilator (intravenous sodium nitroprusside) to titrate blood pressure to 100 to 120 mm Hg in patients with severe hypertension.17
In 2002, the American College of Radiology developed appropriateness criteria for acute chest pain and suspected aortic dissection. These guidelines include:
* chest X-ray: The first step in detection, it reveals a widened aorta in 90% of patients with symptoms.
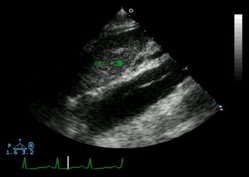
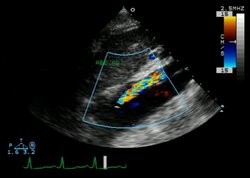
* echocardiogram or transesophageal echocardiogram (TEE): This provides high accuracy for quick decision making. It's also good to use if the patient is too unstable for transport. The operator must be proficient.
* computed tomography (CT): This scan, with a sensitivity greater than 90% and specificity greater than 85%, is used most often to detect suspected dissections.
* magnetic resonance imaging (MRI): This test provides the highest accuracy and sensitivity as well as specificity (nearly 100%) for detection of all forms of dissection. Due to time and transport considerations, it's impractical for acute situations.
* aortography: This proves valuable to diagnose classic aortic dis section but isn't practical in all cases.18
If the patient is unstable on presentation, the health care team should immediately intubate, with stabilization as the objective. Control the patient's blood pressure, because hypertension will add to bleeding and cause the patient's condition to deteriorate quickly.
Use TEE for diagnosis if the patient is too unstable to transport for a CT scan or an MRI. An echocardiogram or TEE will also provide invaluable information regarding the patient's aortic valve-specifically, the degree of aortic insufficiency, which occurs in more than half of patients with type A or proximal dis section.19 You may note the presence of a distinctive murmur, often with a musical quality, with or without evidence of congestive heart failure.20 Notify the cardiovascular surgeon immediately and alert other members of the surgical team.
Type and cross-match the patient for multiple blood products, including packed cells, fresh frozen plasma, platelets, and cryoprecipitate. If your facility can't provide the required level of care (cardiopulmonary bypass), immediately transport the patient to a qualified facility.
Differential diagnosis
A variety of conditions may mimic aortic dissection. When a patient presents with one or more risk factors, rule out aortic dissection before entertaining other diagnoses. Conditions included in the differential diagnosis are:
* myocardial infarction
* stroke
* pericarditis
* cardiac tamponade
* myocarditis
* pulmonary embolism
* aortic insufficiency
* mediastinal tumors.
Treatment
The goal of treatment is to prevent complications. Treatment is based on halting the progression of the dis secting hematoma, since fatal complications arise not from the intimai tear but rather the destructive path taken by the dissection.21 You'll need to intricately balance control of hypertension, prevention of hypotension, and maintenance of adequate perfusion to vital organs.
Surgical intervention is indicated in type A dissections, unless the patient has sustained severe neurological impairment or suspected bowel necrosis has occurred. The purpose of surgery is to reestablish blood flow in the true channel or lumen. This may be accomplished by removing the intimai tear and replacing the dissection with a synthetic graft, thus reinforcing the damaged aorta.
If the patient's dissection involves the coronary arteries, he or she may require coronary artery bypass grafting. The aortic valve may need replacement, depending on the extent of the dissection. If this is the case, the surgeon will replace the damaged ascending aorta and the aortic valve with a composite graft (Bentall procedure). The surgeon will then reimplant the coronary arteries into the graft that replaces the aorta.22
Due to the aorta's frailty, this surgery is demanding and technically difficult to perform. There's a great deal of bleeding associated with the surgery, and often the tissue won't hold the sutures. Spinal cord ischemia with subsequent paraplegia is possible due to inadvertent disruption of the blood supply from the anterior spinal or intercostal arteries during surgery.23 Because surgical mortality can be as high as a quarter of the patients and the risk for complications is great, you'll want to thoroughly educate patients and their family prior to surgery. The patient may not be able to absorb or process all of the information, but make every effort to help his or her family understand the sitaution. Also, although time is critical, allow the family to spend a few moments alone with their loved one.24
All chronic dissections-those extending beyond 14 days-require medical therapy, which is also advised in type B dissections or those confined to the descending aorta. Medical therapy is also the treatment of choice in stable isolated arch dissection. Surgical intervention is indicated for:
* significant aortic insufficiency
* poor blood pressure control
* failing medical therapy
* inadequate pain relief
* progression of the dissection with multi-organ involvement.25
New treatment modalities
Endovascular therapy for the treatment of peripheral arterial disease proves an exciting and advancing field. Treatment for abdominal aortic aneurysm is now possible with a less invasive procedure. A special graft is inserted through the femoral artery and passed into the aneurysm under X-ray guidance.
Once properly positioned, the graft is released inside the aorta, where metal stents attached to the graft expand against the inside vessel wall above and below the aneurysm. This effectively excludes the diseased segment of the artery from blood circulation, preventing rupture.26 Although in its infancy, endovascular therapy for the treatment of descending thoracic aortic aneurysms appears promising.
Prevention
Because lowering blood pressure helps reduce stress on the aorta, individuals who experience an aortic dis section, including those treated surgically, must take medication to control blood pressure for the rest of their lives. Prescribed pharmacologie agents include a beta-blocker or calcium channel blocker and another antihypertensive, such as an angiotensin-converting enzyme inhibitor.27 Initial treatment of choice for hypertension in most cases is a thiazide-type diuretic.28
If the patient's valve was replaced with a mechanical prosthesis, he or she will require anticoagulation for life. he or she may also receive statins to reduce cholesterol plaquing and control atherosclerosis. Educate the patient about risks and the importance of close monitoring.
As previously mentioned, aortic dissection is the most frequent cause of premature death in individuals with Marfan syndrome. Low-risk elective surgery of the abnormal aortic root has the potential to prevent this complication. Successful aortic root replacement early in an individual's life may yield promising results. Although a multitude of factors influence the decision to opt for aortic root replacement, perhaps the single most pressing concern is a critical aortic root diameter of 5 cm or greater.29
After initial treatment, the patient will require serial imaging for close follow-up. The preferred method is MRI, followed by CT, and then TEE. Experts recommend outpatient visits at one, three, six, and 12 months post-operative, and biannually for two years thereafter.30
Living with the risk
Late complications remain a concern and require close monitoring. The risk of another dissection, development of aneurysms in the weakened aorta, and an increase in aortic insufficiency are all potential hazards that accompany this lethal diagnosis. For many patients, the psychological effects of this condition are devastating. The fear of another dissection is often described as a "time bomb waiting to explode." Others, with the help of counseling, learn to adjust to their condition and try to live each day to the fullest.
CE Test
Aortic dissection: the tear that kills
Instructions:
* Read the article beginning on page 26.
* Take the test, recording your answers in the test answers section (Section B) of the CE enrollment form. Each question has only one correct answer.
* Complete registration information (Section A) and course evaluation (Section C).
* Mail completed test with registration fee to: Lippincott Williams & Wilkins, CE Dept., 16th Floor, 345 Hudson St., New York, NY 10014.
* Within 3 to 4 weeks after your CE enrollment form is received, you will be notified of your test results.
* If you pass, you will receive a certificate of earned contact hours and an answer key. If you fail, you have the option of taking the test again at no additional cost.
* A passing score for this test is 12 correct answers.
* Need CE STAT? Visit http://www.nursingcenter.com for immediate results, other CE activities, and your personalized CE planner tool.
* No Internet access? Call 1-800-933-6525, ext. 331 or ext. 332, for other rush service options.
* Questions? Contact Lippincott Williams & Wilkins: 212-886-1331 or 212-886-1332.
Registration Deadline: February 28, 2006
Provider Accreditation:
This Continuing Nursing Education (CNE) activity for 2.0 contact hours is provided by Lippincott Williams & Wilkins, which is accredited as a provider of continuing education in nursing by the American Nurses Credentialing Center's Commission on Accreditation and by the American Association of Critical-Care Nurses (AACN 11696, CERP Category A). This activity is also provider approved by the California Board of Registered Nursing, Provider Number CEP 11749 for 2.0 contact hours. LWW is also an approved provider of CNE in Alabama, Florida, and Iowa and holds the following provider numbers: AL #ABNP0114, FL #FBN2454, IA #75. all of its home study activities are classified for Texas nursing continuing education requirements as Type I.
Your certificate is valid in all states. This means that your certificate of earned contact hours is valid no matter where you live.
Payment and Discounts:
* The registration fee for this test is $14.95.
* If you take two or more tests in any nursing journal published by LWW and send in your CE enrollment forms together, you may deduct $0.75 from the price of each test.
* We offer special discounts for as few as six tests and institutional bulk discounts for multiple tests. Call 1-800-933-6525, ext. 332, for more information.
References
1. Braunwald, E., Libby, P, and Zipes, D.: Heart disease: A textbook of cardiovascular medicine, 6th edition, pgs. 14311448. Philadelphia: W.B. Saunders, 2001.
2. Karmy-Jones, R., Aldea, G., and Boyle, E.: "The continuing evolution in the management of thoracic aortic dissection," Chest. 17(5):1221-1223, 2000.
3. The Merck Manual, 2nd edition. Available online: http://www.merck.com/pubs/ mmanual_home2/sec03/ch035/ch035c .htm.
4. Ibid.
5. Braunwald, E., Libby, P, and Zipes, D.: loc cit.
6. National Marfan Foundation: Emergency diagnosis and treatment of aortic dis section. Available online: http://www. marfan.org/pub/emergency.html.
7. Scott, C., Burruss, N., Kalimi, R., et al.: "Acute aortic dissection during pregnancy," American Journal of Critical Care. 10(10):417-429, 2001.
8. Braunwald, E., Libby, P, and Zipes, D.: loc cit.
9. Ibid.
10. Swalwell, C., and Davis, G.: "Methamphetamine as a risk factor for acute aortic dissection," Journal of Forensic Sciences. 44(1): 23-26, 1999.
11. Braunwald, E., Libby, P, and Zipes, D.: loc cit.
12. Ibid.
13. Ibid.
14. The Merck Manual: loc. cit.
15. Braunwald, E., Libby, P, and Zipes, D.: loc cit.
16. Ibid.
17. Erbel, R., Alfonso, F., Boileau, C., et al.: Available online: http://www.guidelines .gov/summary.aspx?doc_id=2975&nbr= 2201&string=aortic-i-AND+dissection.
18. Zollikofer, C., Klein, W., Mulder, B., and Providencia, L.: "Diagnosis and management of aortic dissection," Journal of the European Heart Association. 18(9):1642-1681, 2001.
19. Braunwald, E., Libby, P, and Zipes, D.: loc cit.
20. Ibid.
21. Ibid.
22. Ibid.
23. Ibid.
24. American College of Radiology: ACR Appropriateness Criteria, 2002. Available online: http://www.acr.org/ dyna/?id=appcrit&pdf=0001-6__acute_ chest_pain_susp_aortic_diss-ac.
25. Braunwald, E., Libby, P, and Zipes, D.: loc cit.
26. Fleck, T., Tschernich, H., Grabenwoger, M., et al.: "A double patch sandwich technique for surgical repair of acute aortic dissection type A," Annals of Thoracic Surgery. 76(2):499-500, 2003.
27. The Merck Manual: loc cit.
28. U.S. Department of Health and Human Services: Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure, NIH publication no. 03-5231, May 2003.
29. Scharrer-Pamler, R., Kotsis, T., Kapfer, X., et al.: " Complications after endovascular treatment of thoracic aortic aneurysms," Journal of Endovascular Therapy. 10(4):711-718, 2003.
30. Erbel, R., Alfonso, R, Boileau, C., et al.: loc cit.
By Cathy A. Yee, RN, MSN
About the author
Cathy A. Yee is a cardiac patient care specialist, Providence Holy Cross Medical Center, Mission Hills, Calif.
Copyright Springhouse Corporation Feb 2004
Provided by ProQuest Information and Learning Company. All rights Reserved