Biological Perspectives
Aripiprazole (Abilify), recently approved by the FDA, is being touted as a new type of antipsychotic. If these claims hold, aripiprazole would be the first in the third generation of antipsychotics. In any historical review based on the assumption that aripiprazole is indeed a unique medicine in the fight against schizophrenia, the following lineage can be traced:
1950 to 1990: First-generation antipsychotics (or traditional agents)-e.g., chlorpromazine, haloperidol, fluphenazine
1990 to present: Second-generation antipsychotics (or atypical agents)-e.g., clozapine, risperidone, olanzapine, quetiapine, ziprasidone
Present to ?: Third-generation antipsychotics (or dopamine system stabilizers [DSSs]e.g-, aripiprazole
First-generation, or traditional, antipsychotics reduce positive symptoms but do not adequately ameliorate negative and cognitive symptoms. Further, they cause extrapyramidal side effects (EPSEs) and serum prolactin elevations, and can aggravate or induce negative and cognitive symptoms. This constellation of symptom relief, symptom aggravation/induction, and side effect causation results from their receptor-blocking profile (Table 1). Most important to this discussion is their dopamine D2 receptor antagonism. This antagonism accounts for positive symptom reduction (mesolimbic tract), negative symptom aggravation/induction (mesocortical tract), EPSEs (nigrostriatal tract), and hyperprolactinemia (turberoinfundibular tract). When tallied with other noxious consequences (e.g., orthostasis, anticholinergic reactions), the need for a different type of antipsychotic agent became apparent.
Second-generation, or atypical, antipsychotics are heralded for their effectiveness in both positive and negative symptoms of schizophrenia. Further, they reportedly cause significantly fewer and less severe EPSEs and prolactin-level elevations. In summary, atypical antipsychotics are "atypical" because negative symptoms improve, EPSEs are minimized, and prolactin levels do not rise. Many of these agents, particularly clozapine, have been exceptionally effective in treatment-refractory individuals. Like the traditional agents, atypical drugs antagonize D2 receptors; however, much of this "atypicality" is credited to a blockade of serotonin 5-HT2A receptors. This latter property is linked to improvement in negative and cognitive symptoms and minimal occurrences of EPSEs (Table 2). Some atypicals (e.g., clozapine, ziprasidone) are also partial agonists at the 5-HT1A receptor, putatively improving depression, anxiety, and negative/cognitive symptoms.
Unfortunately, D2-related side effects common to traditional antipsychotics can occur, as do other, treatment-ending problems, such as weight gain, sedation, prolongation of the QTc interval, and fatal blood dyscrasias. So, though great hope accrued, these significant problems have dampened some of the initial enthusiasm. Hence, the search continues for a drug possessing properties that reduce psychotic symptoms with minimal adverse effects. This search has ushered in what some are calling the third generation of antipsychotic agents.
Third Generation
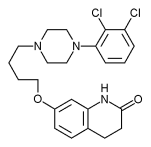
Aripiprazole's mechanism of action differs from all antipsychotics on the market. All current neuroleptics, both traditional and atypical, create their antipsychotic effect by blocking dopamine D2 receptors-that is, they are D2 antagonists (Figure 1). Aripiprazole exerts its effect by D2 partial agonism (Figure 2), and this distinction holds promise for stabilizing the dopamine system (Stahl, 2001a). It is important to note that a partial agonist can act as an agonist or an antagonist, depending on the concentration of a specific neurotransmitter (Tamminga, 2002). That is, at low dopamine levels, a partial agonist will stimulate dopamine receptors, and at high dopamine levels a partial agonist will inhibit dopamine receptors (Stahl). To understand this potential for efficacy, it is important to remember that positive symptoms are thought to be caused by hyperdopaminergic activity in the mesolimbic tract, and negative symptoms by hypodopaminergic activity in the mesocortical tract. A drug that would act to reduce mesolimbic activity while increasing mesocortical activity yet minimize side effects could fulfill the quest for a better drug. Aripiprazole may be that drug. A closer look at just how aripiprazole accomplishes this is worth review.
Several studies have found aripiprazole superior to placebo for treating schizophrenia, equieffective to haloperidol and risperidone for reducing positive symptoms, and superior to haloperidol for improving negative and depressive symptoms (Burris et al., 2002; Jordan et al., 2002; Kane et al., 2002; Stahl, 2001a, 2001b). The particular receptor occupancy profile attributable to these claims are partial agonism of dopamine D2 receptors, partial agonism of serotonin 5-HT1A receptors, and antagonism of 5-HT2 receptors as noted above (Burris et al.; Jordan et al.; Stahl, 2001b).
By partial agonism of D2 receptors, aripiprazole prevents significant amounts of endogenous dopamine in the mesolimbic area from binding with dopamine receptors there. Thus, an area with too much dopamine begins stabilizing because receptors bind to less potent ligands (i.e., agonists with less intrinsic activity). Rather than shutting down the mesolimbic pathway, partial agonism stabilizes the pathway. Likewise, in the "underdopaminized" cortical regions, partial agonism enhances neuronal activity by attaching to dopamine postsynaptic receptors "starved" for dopamine. This too becomes a stabilizing process, and improvements in negative and cognitive symptoms occur. Aripiprazole also reduces prolactin levels compared to other antipsychotics. This mechanism may be related to agonism of D2 receptors in the tuberoinfundibular tract. D2 receptors modulate dopamine's inhibition of prolactin and partial agonism of these receptors is thought to account for reductions in serum prolactin (Yokoi et al., 2002).
Aripiprazole's antagonism of 5-HT2A receptors confers the same advantages noted in atypical agents. The 5-HT2A receptor is thought to modulate dopamine activity. 5-HT2A agonist activity decreases dopamine activity, while 5-HT2A antagonism increases dopamine activity. It is thought that by blocking 5HT2A receptors in the nigrostriatal tract, EPSEs are reduced and blocking 5-HT2A in the frontal cortex reduces negative and cognitive symptoms.
Aripiprazole provides a partial agonism at 5-HT1A receptors as well. It is thought that agonist activity at this receptor is associated with improvement in anxiety, depression, negative, and cognitive symptoms. Because of this feature of the drug some have contemplated referring to aripiprazole as a dopamine-serotonin system stabilizer.
A final and interesting mechanism of action mentioned here concerns aripiprazole's function as an agonist at presynaptic autoreceptors. Autoreceptors are part of a neurotransmitter's "self-regulatory" or autoregulatory system (i.e., a negative feedback system). That is, when an agonist stimulates the autoreceptor, release of the neurotransmitter is regulated downward. When an autoreceptor is blocked, the message is sent to increase transmitter release. It seems reasonable that autoreceptor stimulation could be of particular therapeutic advantage in toning down hyperdopaminergic processes in the mesolimbic area. However, exactly how this particular molecular feature facilitates reductions in schizophrenic symptomatology remains to be elucidated.
Beyond these therapeutic advances, aripiprazole appears to have a good side-effect profile-research indicates minimal weight gain, minimal sedation, no QTc interval prolongation, prolactin levels comparable to placebo, EPSEs equivalent to placebo, and minimal orthostasis (Burris et al., 2002; Jordan et al., 2002; Stahl, 2001a, 2001b). Some concerns related to increased levels of akathisia have been voiced, however, studies are not conclusive.
Summary
Schizophrenia places an incredible burden on patients, families, communities, and governments, therefore intense efforts to find therapeutic responses to this illness continue. The traditional antipsychotics were discovered by chance, the atypical antipsychotics were configured to preserve "what worked" while adding and eliminating important effects, and the next generation continues to evolve in an attempt to improve on previous generations. Aripiprazole is extoled as a new generation of antipsychotic drugs. Information to date suggests it is an effective antipsychotic with a remarkable side effect profile. We are hopeful this drug will provide a relief for the suffering associated with schizophrenia.
References
Burris, K.D., Molski, T.F., Ryan, E., Tottori, K., Kikuchi, T., Yocca, F.D., & Molinoff, P.B. (2002). Aripiprazole, a novel antipsychotic, is a high-affinity partial agonist at human dopamine D2 receptors. Journal of Pharmacology and Experimental Therapeutics, 302, 381-389.
Jordan, S., Koprivica, V., Chen, R., Tottori, K., Kikuchi, T., & Altar, C.A. (2002). The antipsychotic aripiprazole is a potent, partial agonist at the human 5-HTIA receptor. European Journal of Pharmacology, 441,137-140.
Kane, J.M., Carson, W.H., Saha, A.R., McQuade, R.D., Ingenito, G.G., Zimbroff, D.L., & Ali, M.W. (2002). Efficacy and safety of aripiprazole and haloperidol versus placebo in patients with schizophrenia and schizoaffective disorder. Journal of Clinical Psychiatry, 63, 763-771.
Stahl, S.M. (2001a). Dopamine system stabilizers, aripiprazole, and the next generation of antipsychotics, Part I: 'Goldilocks' actions at dopamine receptors. Journal of Clinical Psychiatry, 62, 841-842.
Stahl, S.M. (2001b). Dopamine system stabilizers, aripiprazole, and the next generation of antipsychotics, Part II: Illustrating their mechanism of action. Journal of Clinical Psychiatry, 62, 923-924.
Tamminga, C.A. (2002). Partial dopamine agonists in the treatment of psychosis. Journal of Neural Transmission, 109, 411-420.
Yokoi, F., Grunder, G., Biziere, K., Stephane, M., Dogan, A.S., Dannals, R.F., et al. (2002). Dopamine D2 and D3 receptor occupancy in normal humans treated with the antipsychotic drug aripiprazole (OPC 14597): A study using positron emission tomography and [11-- C]raclopride. Neuropsychopharmacology, 27, 248-259.
Search terms: Antipsychotics, aripiprazole
Norman L. Keltner, EdD, RN, and Vicki Johnson, PhD, RN, CUCNS
Norman L. Keltner, EdD, RN, Professor
Vicki Johnson, PhD, RN, CUCNS, Assistant Professor
School of Nursing, University of Alabama at Birmingham
Author contact: keltner@son.uab.edu, with a copy to the Editor: mary77@concentric.net
Copyright Nursecom, Inc. Oct-Dec 2002
Provided by ProQuest Information and Learning Company. All rights Reserved