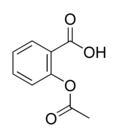
Objectives: Release of thromboxane (Tx) [A.sub.2] by platelets may be one of multiple factors that are responsible for lung injury after cardiopulmonary bypass, leading to pulmonary vasoconstriction and impaired oxygenation. In experimental models, the inhibition of Tx receptor or its production improved lung function. The use of aspirin, which is used widely in the treatment of ischemic heart disease because of its antiplatelet activity, is usually discontinued a week before the patient undergoes the operation to restore normal platelet hemostatic function. The purpose of this study was to determine the relationship between the time of cessation of aspirin before coronary artery bypass surgery, and postoperative oxygenation and bleeding.
Design: A prospective clinical study comparing the effect of aspirin on postoperative oxygenation in patients who had been treated or had not been treated with aspirin.
Setting: Tx levels in the pericardial fluid, oxygenation, and bleeding were compared between the two groups.
Patients: Thirty-two patients with coronary artery disease who were undergoing coronary artery bypass grafting. Fourteen of these patients received aspirin until the day of the operation, whereas 18 patients stopped receiving aspirin at least 1 week before undergoing the operation.
Main results: Mean ([+ or -]SD) Tx levels in the pericardial fluid were significantly lower in the aspirin group (117 [+ or -] 47 pg/mL) compared to those in the control group (1,306 [+ or -] 2,048 pg/mL; p = 0.02). The duration of ventilation after the operation was significantly longer in the nonaspirin group (9.6 [+ or -] 5.6 h vs 3.8 [+ or -] 1.4 h, respectively; p = 0.0004). P[O.sub.2] reached a higher level while patients breathed 100% [O.sub.2] in the aspirin group (235 [+ or -] 54 mm Hg vs 176 [+ or -] 27 mm Hg, respectively; p = 0.001). The mean amount of bleeding during the first 24 h after surgery was increased in the aspirin group (710 [+ or -] 202 mL) compared with the nonaspirin group (539 [+ or -] 143 mL; p = 0.01), but these patients did not require more transfusions.
Conclusions: The administration of aspirin until the operation may improve oxygenation with only a slight increase in bleeding. This improvement is probably mediated by antiplatelet activity and Tx inhibition by aspirin.
Key words: aspirin; cardiopulmonary bypass; coronary disease; oxygenation; thromboxane; ventilation
Abbreviations: CABG = coronary artery bypass graft; CPB = cardiopulmonary bypass pump; FI[O.sub.2] = fraction of inspired oxygen; Tx = thromboxane
**********
Lung injury is a frequent complication after cardiac surgery using cardiopulmonary bypass (CPB). (1,2) It has been shown that when the effects of general anesthesia and surgical injury are similar, the use of CPB may be the dominant factor worsening postoperative respiratory dysfunction. (1) Various inflammatory mediators, produced or released during CPB, are believed to exert a damaging effect through the activation of WBCs. (3-5) The depletion of these activated leukocytes was performed in the clinical setting in an attempt to improve lung function. (6,7) The activation and degranulation of platelets, with the release of thromboxane (Tx) [A.sub.2], also has been implicated as a causative factor in pulmonary dysfunction. (8) In animal models, the production of Tx has been related to myocardial dysfunction (9) and to pulmonary hypertension following CPB. (10) The blockade of Tx receptors (11,12) or the inhibition of Tx synthesis (13) may virtually eliminate pulmonary injury and significantly improve contractile function after CPB. (9) In the canine model, a decline in systemic oxygenation was associated with CPB due to the augmentation of hypoxic pulmonary vasoconstriction. This was ameliorated by indomethacin, inhibiting Tx synthesis. (4)
Low-dose aspirin therapy is indicated in many patients with coronary artery disease. Aspirin reduces the risk of complications secondary to coronary artery disease, owing to the inhibition of platelet aggregation and Tx production. Since the tendency for bleeding may increase in patients receiving aspirin, its administration is routinely stopped 7 to 10 days before the patient undergoes elective surgery. Tx levels are therefore expected to increase to normal values at the time of surgery. Some candidates for coronary artery bypass grafting (CABG) continue to receive aspirin until the operation because of early referral, because of the confusion with brand names of medications containing aspirin, or because they become unstable and need an urgent operation. In some patients, aspirin therapy is contraindicated because of peptic ulcer disease.
Our purpose was to study the influence of aspirin administration until the day of surgery on postoperative oxygenation in a group of patients undergoing CABG operation and to compare it to that in a group of patients in whom aspirin therapy was stopped a week or more before the operation. We also compared Tx and aspirin levels in the two groups, as well as bleeding and the need for blood transfusion in the postoperative course.
MATERIALS AND METHODS
Thirty-two consecutive patients undergoing CABG were enrolled in the study. The institutional human ethics committee was consulted for the need of approval according to the study design. Since all results were taken from routine tests, and no invasive procedures were performed on patients for the purpose of the study, the committee waived the review and the need for approval. Patients who received 100 mg of aspirin daily until the operation were included in the aspirin group (ie, the study group; n = 14), and those in whom aspirin therapy was stopped at least 7 days before the operation were included in the nonaspirin group (ie, the control group; n = 18). We excluded patients with known pulmonary disease and reoperation. We also excluded patients who had recently experienced myocardial infarction, had poor left ventricular function (ejection fraction, < 0.35), and were in New York Heart Association functional class III-IV, as these three conditions increase plasma Tx levels. (14-15) All patients had a measured oxygen saturation of [greater than or equal to] 95% while breathing room air before the surgery. Patients were defined as smokers whenever a history of smoking existed during the year before the operation. Renal failure was defined as a serum creatinine level of > 120 [micro]g/mL. The urgency of each operation was recorded.
An urgent operation was defined as one that had been performed within 48 h from the time of cardiac department admission or catheterization in patients with refractory angina, who were receiving full medical treatment. The remaining cases were defined as elective. Patients with COPD were defined as those who were having clinical manifestations related to emphysema, chronic bronchitis, or asthma with laboratory evidence from at least one pulmonary function test showing an FE[V.sub.1] of < 70% predicted and an FE[V.sub.1]/FVC ratio of < 60%, as measured by spirometric testing. As shown in Table 1, there were no significant differences between the two groups in the preoperative data.
All patients received anesthesia using a standard technique. Ventilation parameters during the operation were as follows: fraction of inspired oxygen (FI[O.sub.2]), 50%; tidal volume, 8 to 10 mL/kg; and no positive end-expiratory pressure.
All operations were performed through a median sternotomy incision. The left internal mammary (thoracic) artery was harvested in all patients, and the left pleura was opened and subsequently drained separately in all patients. The right internal mammary artery was not harvested, and the right pleura remained intact in all patients.
The pericardial fluid was sampled immediately after the pericardial opening and was stored at -20[degrees]C. We sampled the pericardia] fluid to determine Tx levels in a body compartment that is less sensitive to short-term fluid shifts occurring during the perioperative period. (16-18) Tx [B.sub.2], a more stable derivative of Tx [A.sub.2], was determined by enzyme-linked immunosorbent assay in our laboratory (R&D Systems; Minneapolis, MN). All patients had the same protocol of CPB and myocardial protection. Topical cooling was not used, and there was no direct or indirect left ventricular venting. During CPB, the lungs remained deflated.
The maximum P[O.sub.2] recorded was the arterial [O.sub.2] tension on arrival at the ICU, which was recorded after manual ventilation with 100% [O.sub.2] for at least 15 min. A chest radiograph that was performed on arrival at the ICU excluded pneumothorax and pleura/effusion, and confirmed adequate ventilation.
In the ICU, the patients received ventilation using a standard ventilation formula: FI[O.sub.2], 60%; tidal volume, 8 to 10 mL/kg; positive end-expiratory pressure, 5 cm [H.sub.2]O for 1 h and then adjusted individually, aiming at early extubation. The use of F1[O.sub.2] of > 70% was avoided to prevent oxygen toxicity and resorption collapse. Ventilation duration was the time interval between connection to the ventilator and extubation. Hypoxia was defined as a Poe of < 60 mm Hg. Weaning and extubation were performed by the nursing staff, who were not informed of the study, according to standard criteria in all patients. To qualify for extubation, a patient had to be alert, hemodynamically stable, and capable of maintaining self-ventilation. The minimum Poe was obtained retrospectively from the patient chart when the patient was extubated and breathing spontaneously through a facemask with 40% [O.sub.2]. Postoperative care, including treatment for bleeding, was performed according to standard routines in all patients.
To determine the direct effects of aspirin, we measured aspirin levels in the serum and pericardial fluid of all patients. Aspirin concentration was determined by reflectance spectrophotometry (Vitros System 950; Ortho Clinical Diagnostics Inc; Rochester, NY), with a sensitivity range of 1 to 40 mg/dL. The postoperative complications and outcome, including ICU stay and hospitalization time, were also recorded.
Statistical Analysis
All values were reported as the mean [+ or -] SD. The univariate comparisons between the two groups were performed using the Student t test and [chi square] test where appropriate. In all measurements, a p value of < 0.05 was considered to be significant. After univariate analysis, variables with p < 0.05 were analyzed by multivariate analysis to identify the independent predictors of postoperative oxygenation. The correlation between parameters was determined by Pearson test, with an r value of [greater than or equal to] 0.4 considered to be a good correlation.
RESULTS
No mortality occurred in either the study group or the control group. As shown in Table 2, the operative data were similar for both groups except for the mean operation time of 3.1 [+ or -] 0.4 h in the aspirin group, which was longer than that in the control group (2.7 [+ or -] 0.4 h; p = 0.03). As expected, a significant difference in Tx levels was found between the study group (117 [+ or -] 47 pg/mL) and the control group (1,306 [+ or -] 2,048 pg/mL; p = 0.02). Aspirin was not detected in any sample, neither in the pericardial fluid nor in the serum of patients (both groups).
Data regarding the postoperative course is summarized in Table 3. Mean ventilation time was significantly shorter in the aspirin group compared to the control group (3.8 [+ or -] 1.4 h vs 9.6 [+ or -] 5.6 h; p = 0.0004). Pa[O.sub.2] reached a maximum of 235 [+ or -] 54 mm Hg in the study group, when ventilated manually with an FI[O.sub.2] of 1.0, and 176 [+ or -] 27 mm Hg in the control group (p = 0.001). The minimal value of Pa[O.sub.2] in the study group was also higher compared to that in the control group (90 [+ or -] 9 mm Hg vs 76 [+ or -] 8 mm Hg; p = 0.0001). A significant negative correlation was found between Tx levels and minimal Pa[O.sub.2] (r = -0.44) and maximal Pa[O.sub.2] (r = -0.51). Tx levels also correlated well with ventilation time (r = 0.45).
The effect of hemodilution or hemoconcentration, which could alter the extravascular fluid volume state, was negligible since no significant differences in fluid infusion and urine output were found between the two groups. Although total drainage through the chest tubes was greater than that in the aspirin group, the need for blood and blood products was similar in both groups, and no significant difference was seen in hemoglobin levels on hospital discharge (Table 3). The length of ICU stay for the control group was significantly longer than that for the study group; however, the total length of hospital stay was similar for both groups.
Using the multivariate analysis model, the association between preoperative variables that could potentially influence outcome parameters in this study was examined. In the univariate model, only smoking history was associated with the postoperative minimum P[O.sub.2] (p = 0.04) and maximum P[O.sub.2] (p = 0.03). However, in the multivariate model, the group effect was the only independent factor determining the outcome parameters (Table 4).
DISCUSSION
Some reports have demonstrated important benefits from the preoperative administration of aspirin in patients undergoing CABG, reducing the rate of perioperative myocardial infarction, (19) and even reducing the in-hospital mortality rate by 27% or 30%. (20) The benefit of perioperative aspirin use on graft patency is well established. Although a number of studies (21) have reported that patients receiving aspirin before undergoing CABG had increased blood loss, increased transfusion requirements, and a higher incidence of reoperation for bleeding, other studies (20,22) have not documented any significant increase in bleeding tendency.
In this study, we tried to determine whether the antiplatelet effect of aspirin, mediated by the inhibition of Tx synthesis, may improve lung function in patients undergoing CABG surgery. The patients in the study group were significantly better in their oxygenation capability. Fifteen minutes after manual ventilation with pure oxygen, they had a significantly higher Pa[O.sub.2] (maximum P[O.sub.2]). Also, the mean nadir of the Pa[O.sub.2] while breathing with a facemask with an FI[O.sub.2] of 0.4 was 90 [+ or -] 9 mm Hg in the study group, which was higher than that of the control group (76 [+ or -] 8 mm Hg). Ventilation time was also significantly shorter among patients receiving aspirin until the operation.
The operation in the aspirin group was on average about 24 min longer than that in the control group. This difference may be explained by the extra time needed for meticulous hemostasis. Patients in the aspirin group also had a larger amount of drainage through the chest drains during the first 24 h. It should be emphasized, however, that the longer duration of the operation and the increased drainage had no implications on outcome. The difference between the groups in terms of length of ICU stay was most probably due to the longer ventilation time in the control group. Although the difference between the groups was of only a few hours, it should be realized that the longer the ICU stay, the greater the potential for ICU-related complications.
The question arising from these results is whether the advantages observed in the study (aspirin) group can be attributed to the significantly lower levels of Tx in this group at the time of surgery, or whether some unrelated factors are responsible for the improvement in lung function after CABG in these patients. This hypothesis is supported by the significant (negative) correlation between Tx levels and oxygenation, in the absence of differences in aspirin levels (which were negligible) between the groups and when multivariate analysis did not detect any other factor independently influencing postoperative lung function.
The beneficial effect of Tx receptor blockade on oxygenation was demonstrated by Thies et al (23) in an experimental model. Johnson et al (3) showed how the decrease in oxygen tension after extracorporeal perfusion in dogs was ameliorated after pretreatment with indomethacin. In most studies on Tx and its effects, a selective Tx receptor blocking agent such as SQ30741 (24) or a Tx production inhibitor (dazmegrel) (13) were used to investigate the effects of Tx elimination. These studies characterized the direct action of Tx and the effect of its inhibition.
The potent vasoactive effect of Tx on the lungs is mediated directly by lung tissue but also indirectly by other ischemic organs releasing Tx. During extracorporeal perfusion or later, ischemia may occur in multiple organs like muscles, kidneys, heart, and all other organs as long as it does in the lung tissue. The Tx, which is generated during ischemia, has an injurious effect on the lung, no matter its origin. Increased lung permeability following lower torso ischemia and reperfusion has been attributed to Tx. (25) The lower Tx levels in our study group could account for the decreased permeability of the lung tissue in that group, explaining the better oxygenation.
In this study, we excluded the patients who had experienced myocardial infarction, had poor left ventricular function, and had a higher New York Heart Association functional class to eliminate a possible bias and to produce a homogenous group. Since these patients have a higher level of Tx in their plasma, they will probably benefit even more from its inhibition.
CONCLUSIONS
The preoperative inhibition of Tx synthesis in platelets by aspirin reduced Tx levels significantly before onset of CPB. The resulting low levels of Tx contributed to improved oxygenation and shorter ventilation time after CPB. This, in turn, shortened the ICU stay, which is an important advantage in itself. Although a larger amount of drainage was recorded postoperatively in patients in the aspirin group, there was no need for more blood transfusion in this group, and subjects in both the study group and the control group were discharged from the hospital with similar hemoglobin levels. These beneficial effects may be attributed to aspirin, thereby supporting the recommendation not to discontinue aspirin therapy before CABG with CPB.
* From the Department of Cardiothoracic Surgery (Dr. Gerrah), Assuta Medical Center, Tel Aviv, Israel; the Department of Cardiothoracic Surgery (Dr. Elami), Hebrew University, Hadassah Medical School. Jerusalem Israel; the Department of Cardiothoracic Surgery (Dr. Stamler), Rabin Medical Center, Sackler Medical School, Tel Aviv, Israel; and the Department of Internal Medicine (Ms. Smirnov and Dr. Stoeger), Kaplan Medical Center, Rehovot, Israel.
REFERENCES
(1) Taggart DP, El-Fiky M, Carter R, et al. Respiratory dysfunction after uncomplicated cardiopulmonary bypass. Ann Thorac Surg 1993; 56:1123-1128
(2) Birch I, Regragui IA, Izzat MB, et al. Effects of cardiopulmonary bypass temperature on pulmonary gas exchange after coronary artery operations. Ann Thorac Surg 1996; 61:118-123
(3) Johnson D, Thomson D, Hurst T, et al. Neutrophil-mediated acute lung injury after extracorporeal perfusion. J Thorac Cardiovasc Surg 1994; 107:1193-1202
(4) Asimakopoulos G, Smith PL, Ratnatunga CP, et al. Lung injury and acute respiratory distress syndrome after cardiopulmonary bypass. Ann Thorac Surg 1999; 68:1107-1115
(5) Paparella D, Yau TM, Young E. Cardiopulmonary bypass induced inflammation: pathophysiology and treatment: an update. Eur J Cardiothorac Surg 2002; 21:232-244
(6) Morioka K, Muraoka R, Chiba Y, et al. Leukocyte and platelet depletion with a blood cell separator: effects on lung injury after cardiac surgery with cardiopulmonary bypass. J Thorac Cardiovasc Surg 1996; 111:45-54
(7) Mihaljevic T, Tonz M, yon Segesser LK, et al. The influence of leukocyte filtration during cardiopulmonary bypass on postoperative lung function: a clinical study. J Thorac Cardiovasc Surg 1995; 109:1138-1145
(8) Collman RW. Platelet and neutrophil activation in cardiopulmonary bypass. Ann Thorac Surg 1990; 49:32-34
(9) Byrne JG, Appleyard RF, Sun SC, et al. Cardiac derived thromboxane A.a: an initiating mediator of of reperfusion injury. J Thorac Cardiovasc Surg 1993; 105:689-693
(10) Cave AC, Manche A, Derias NW, et al. Thromboxane A2 mediates pulmonary hypertension after cardiopulmonary bypass in the rabbit. J Thorac Cardiovasc Surg 1993; 106:959-967
(11) Mendeloff EN, Liang IY, Swan JA, et al. Thromboxane A2 receptor-specific antagonism in hypothermic cardiopulmonary bypass. Ann Thorac Surg 1994; 57:999-1006
(12) Smith WJ, Murphy MP, Applleyard RF, et al. Prevention of complement-induced pulmonary hypertension and improvement of right ventricular function selective thromboxane receptor antagonism. J Thorac Cardiovasc Surg 1994; 107: 800-806
(13) Friedman M, Wang SY, Sellke FW, et al. Pulmonary injury after total or partial cardiopulmonary bypass with thromboxane synthesis inhibition. Ann Thorac Surg 1995; 59:598-603
(14) Lelcuk S, Alexander F, Valeri CR, et al. Ischemia stimulates tissue thromboxane synthesis. Surg Forum 1984; 35:76-78
(15) Bhat AM, Sacks HM, Osborne JA, et al. Protective effect of the specific thromboxane receptor antagonist, BM-13505, in reperfusion injury following acute myocardial ischemia in cats. Am Heart J 1989; 117:799-803
(16) Gibson AT, Segal MB. A study of the composition of pericardial fluid, with special reference to the probable mechanism of fluid formation. J Physiol 1978; 277:367-377
(17) Meyers DG, Meyers RE, Prendergast TW. The usefulness of diagnostic tests on pericardial fluid. Chest 1997; 111:1213-1221
(18) Fujita M, Komeda M, Hasegawa K, et al. Pericarchal fluid as a new material for clinical heart research. Int J Cardiol 2001; 77:113-118
(19) Klein M, Keith PR, Dauben HP, et al. Aprotinin counterbalances an increased risk of peri-operative hemorrhage in CABG patients pre-treated with aspirin. Eur J Cardiothorac Surg 1998; 14:360-366
(20) Dacey LJ, Munoz JJ, Johnson ER, et al. Effect of preoperative aspirin use on mortality in coronary artery bypass grafting patients. Ann Thorac Surg 2000; 70:1986-1990
(21) Ferraris VA, Ferraris SP, Joseph O, et al. Aspirin and postoperative bleeding after coronary artery bypass grafting. Ann Surg 2002; 235:820-827
(22) Reich DL, Patel GC, Vela-Cantos F, et al. Aspirin does not increase homologous blood requirements in elective coronary bypass surgery. Anesth Analg 1994; 79:4-8
(23) Thies SD, Corbin RS, Goff CD, et al. Thromboxane receptor blockade improves oxygenation in an experimental model of acute lung injury. Ann Thorac Surg 1996; 61:1453-1457
(24) Goff CD, Corbin RS, Theiss SD, et al. Postinjury thromboxane receptor blockade ameliorates acute lung injury. Ann Thorac Surg 1997; 64:826-829
(25) Klausner JM, Paterson IS, Goldman G, et al. Thromboxane A2 mediates increased pulmonary microvascular permeability following limb ischemia. Circ Res 1989; 64:1178-1189
Manuscript received July 30, 2004; revision accepted November 11, 2004.
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (www.chestjournal. org/misc/reprints.shtml).
Correspondence to: Rabin Gerrah, MD, 15 Hagana St, Apartment 3, Holon 58275, Israel; e-mail: rabin@assuta.com
COPYRIGHT 2005 American College of Chest Physicians
COPYRIGHT 2005 Gale Group