Study objective: Eosinophilic infiltration of airway tissue is a central feature of aspirin-induced asthma (AIA). Eotaxins belong to the family of CC chemokines, which coordinate the recruitment of inflammatory cells bearing chemokine (C-C motif) receptor-3 to sites of allergic inflammation. In the present study, the levels of eotaxin-1, eotaxin-2, and eotaxin-3 following an oral aspirin provocation test (APT) were measured, and the relationship between the eotaxin level and clinical parameters in patients with asthma was evaluated.
Patients and design: An APT was performed in patients with asthma. Twenty AIA patients and 23 aspirin-tolerant asthma (ATA) patients were identified. Plasma levels of eotaxin-1, eotaxin-2, and eotaxin-3 levels were measured by enzyme-linked immunosorbent assay in the 43 patients with asthma and in 39 control subjects.
Results: The proportion of blood eosinophils was significantly higher in asthmatic patients than in control subjects. Nasal polyps were more common in AIA patients than in ATA patients (p < 0.05). In addition, the eotaxin-1 level was higher in AIA and ATA patients than in control subjects (p < 0.01 for each). The eotaxin-2 level was higher in ATA patients than in either the AIA patients (p < 0.05) or control subjects (p < 0.01). Similarly, the eotaxin-3 level was higher in ATA patients than in control subjects. A trend toward higher plasma levels of eotaxin-1 and eotaxin-3 at baseline and at 4 h after APT administration in the ATA group was noted but was not significant. Eotaxin-2 was also higher in ATA patients than in AIA patients at baseline and at 4 h after the APT.
Conclusion: This study shows that eotaxin-2 is differentially secreted in patients with asthma according to aspirin intolerance, and that secretion is not time-dependent in response to the APT in AIA and ATA patients. It therefore appears that eotaxin-2 may be up-regulated and may act differentially in patients with ATA.
Key words: aspirin; asthma; eosinophils; eotaxin
Abbreviations: AIA = aspirin-induced asthma; APT = aspirin provocation test; ATA = aspirin-tolerant asthma; CCL = CC chemokine ligand; CCR3 = CC chemokine receptor-3; IL = interleukin; P[C.sub.20] = provocative concentration of a substance causing a 20% fall in FE[V.sub.1]
**********
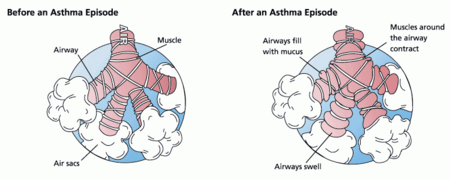
Aspirin-induced asthma (AIA) affects about 5 to 10% of asthmatic adults and is found more often in women. (1) The exacerbation develops within a couple of hours following the ingestion of aspirin, often accompanied by rhinorrhea, conjunctival irritation, and scarlet flush of the head and neck. These reactions are often dangerous; indeed, a single therapeutic dose of aspirin or other nonsteroidal anti-inflammatory drugs can provoke violent bronchospasm, shock, loss of consciousness, and respiratory arrest. (2,3) Persistent inflammation with marked eosin ophilia is found in the airways of affected patients,(4) and eosinophilic infiltration of airway tissue is a central feature of AIA. The number of eosinophils in AIA patients is 4 times that in patients with aspirintolerant asthma (ATA) and is 15 times that in people without asthma. (5)
Based on the results of animal studies, (6,7) eotaxin-1 or eotaxin-2 cooperates with interleukin (IL)-5 to facilitate tissue infiltration by eosinophils. In human experimental studies, (8,9) the cooperative actions of IL-5 and eotaxin-i have also been shown. Systemic IL-5 induces the peripheral mobilization of eosinophils into the circulation, increases the number of circulating eosinophil progenitors, and causes terminal differentiation of eosinophils by increasing CC chemokine receptor-3 (CCR3) expression. (10,11) Thus, IL-5 and eotaxins locally produced in the airways of asthmatic patients are thought to have a synergistic effect on airway inflammation in AIA patients.
To date, three members of the eotaxin family have been identified: eotaxin-1 (CC chemokine ligand [CCL]-11) (12); eotaxin-2 (CCL24) (13); and eotaxin-3 (CCL26). (14) As the three eotaxins share the same CCR3 and have the potential to activate eosinophils in vitro, (15-17) eotaxin-2 and eotaxin-3 may play important roles in the development of asthma, as does eotaxin-1. However, it is still unclear which types of eotaxins are mainly involved in the development of hypersensitivity to aspirin. Given that eosinophilic infiltration is more extensive in the airways of AIA patients than in those of ATA patients, we hypothesized that the number of eotaxins are increased accordingly. We therefore compared the plasma levels of eotaxin-1, eotaxin-2, and eotaxin-3 in patients with AIA and ATA at baseline and in response to provocation with aspirin.
MATERIALS AND METHODS
Subjects
The study examined 39 healthy subjects and 43 asthmatic patients who were recruited from the outpatient clinics of Bucheon Hospital of Soonchunhyang University. The patients had mild-to-moderate persistent asthma, based on their symptom severity and initial FE[V.sub.1], but had not experienced an acute exacerbation or ingested systemic steroids in the 6 weeks prior to the study. (15) All of the patients had clinical symptoms of asthma, a positive bronchodilator test result (ie, a > 15% increase in FE[V.sub.1]), and/or airway hyper-reactivity (ie, provocative concentration of a substance [methacholine] causing a 20% fall in FE[V.sub.1] [P[C.sub.20]] of < 10 mg/mL), (19) as measured using a modified version of the method of Chai et al. (20) Healthy subjects had normal FE[V.sub.1] levels (ie, > 75% predicted), normal values for P[C.sub.20] for methacholine (> 25 mg/mL), and normal findings on a simple chest radiogram. Complete cell counts and differential cell counts were done automatically using a cell counter (COULTER COUNTER; Beckman Coulter; Fullerton, CA). Total IgE level was measured (CAP system; Pharmacia Diagnostics; Uppsala, Sweden). Atopy was defined as the presence of an immediate skin reaction (ie, a wheal > 3 mm in diameter) to [greater than or equal to] 1 of 24 common aeroallergens. (21) None of the subjects had received any drugs, such as antihistamine, eromolyn, theophylline, sympathomimeties, or inhaled steroids, that could have interfered with the aspirin provocation test (APT) within 72 h of testing. The study was approved by the institutional review board of the hospital.
Oral APT
The oral APT was administered over 2 days using a modification of the method of Stevenson and Simon. (22) On the first day, the patient ingested placebo capsules every 2 h. Spirometry, including flow-volume loops, was recorded every hour, and FE[V.sub.1] did not vary by > 15% from baseline during the full day of placebo challenges. Patients were tested with a starting dose of aspirin of 10 mg. If no symptoms were observed, this dose was increased to 625 mg during the 2-day provocation time.
All challenges were earried out in the morning in the presence of a highly trained and experienced physician, and with emergency treatment available. The reaction was considered to be positive only if a fall in FE[V.sub.1] of > 20% occurred, accompanied by symptoms of bronchial obstruction and irritation of the nose or eyes. Blood sampling was done immediately when the FE[V.sub.1] fell by > 20% (ie, positive responder) during the aspirin challenge test or at 2 h after the last dose administered in the aspirin challenge if FE[V.sub.1] did not fall > 20% during the postchallenge observation (ie, negative responder).
Aspirin tolerance was characterized by a change of < 15% in FE[V.sub.1] following aspirin provocation, as described above, and without respiratory and skin manifestations. Healthy subjects had no history of aspirin hypersensitivity and did not take the APT.
Measurement of Eotaxin-1, Eotaxin-2, and Eotaxin-3 by Enzyme-Linked Immunosorbent Assay
Plasma eotaxin-1, eotaxin-2, and eotaxin-3 were measured in plasma using a quantitative sandwich enzyme immunoassay kit (R&D Systems; San Diego, CA). The lower limits of detection for eotaxin-1, eotaxin-2, and eotaxin-3 were 6.25, 15.6, and 62.5 pg/mL, respectively. Values below this limit were assumed to be zero for the statistical analysis. The interassay and intraassay coefficients of variance were < 10%.
Statistical Analysis
All data were analyzed using a statistical software package (SPSS, version 11.0; SPSS; Chicago, IL). The data are expressed as the mean [+ or -] SE. Intergroup comparisons were assessed by the Mann-Whitney U test or the [chi squre] test. The correlation between variables was examined by the Spearman rank correlation coefficient. A p value of < 5% was regarded as being statistically significant.
RESULTS
The clinical parameters of the study subjects are summarized in Table 1. The percentage of blood eosinophils was significantly higher in the AIA and ATA patients than in that in healthy control subjects (p < 0.01). Nasal polyps were more common in AIA patients than in ATA patients (p < 0.05). The mean percentages by which FE[V.sub.1] fell following the APT were 26.7 [+ or -] 2.82% in the AIA group and 3.34 [+ or -] 1.12% in the ATA group (p < 0.01).
The mean basal eotaxin-1 levels were significantly higher in the AIA and ATA groups than in control subjects (71.49 [+ or -] 11.06 and 92.46 [+ or -] 17.34 pg/mL, respectively, vs 25.78 [+ or -] 2.85 pg/mL; p < 0.01) [Fig 1, left, A]. However, there was no difference in the basal eotaxin-1 levels between the two groups of asthmatic patients (p > 0.05). The mean basal eotaxin-2 level was significantly higher in the ATA group than in control subjects (175.59 [+ or -] 14.24 vs 127.06 [+ or -] 7.73 pg/mL, respectively; p < 0.01) and patients in the AIA group (175.59 [+ or -] 14.24 vs 140.99 [+ or -] 20.77 pg/mL, respectively; p < 0.05) [Fig 1, middle, B]. AIA patients had eotaxin-2 levels that were comparable to those of healthy control subjects (p > 0.05). The basal eotaxin-3 level was detected in 1 of 39 healthy control subjects (2%), 3 of 20 patients with AIA (15%), and 6 of 9.3 patients with ATA (26%). Thus, the mean eotaxin-3 level in the ATA group, but not in the AIA group, was significantly higher than that in control subjects (p < 0.01) [Fig 1, right, C]. There was no difference in basal eotaxin-3 levels between AIA and ATA patients (p > 0.05). The levels of eotaxin-1, eotaxin-2, and eotaxin-3 were not significantly changed by APT in the AIA and ATA groups (p > 0.05) [Fig 2]. When the postchallenge levels of eotaxin-1, eotaxin-2, and eotaxin-3 were compared between these two groups, the level of eotaxin-2, but not those of eotaxin-1 or eotaxin-3, was persistently higher in ATA patients than in AIA patients.
[FIGURES 1-2 OMITTED]
DISCUSSION
Although there is low sequence similarity among the eotaxins, all three have been shown to signal via CCR3. (16,17,23,24) CCR3 is expressed on eosinophils, T-helper type 2 lymphocytes, basophils, and mast cells, (6,) all of which play important roles in the development of asthma. As the three eotaxins share the same CCR3 and have the potential to activate eosinophils in vitro, (15-17,23) eotaxin-2 and eotaxin-3, like eotaxin-1, are expected to play important roles in the development of asthma. The identification of three eotaxins raises the issue of the distinct role of each of these functionally analogous CC chemokines in allergic inflammation. However, it is still unclear which types of eotaxins are mainly involved in the development of the aspirin-tolerant and aspirinintolerant forms of asthma. In order to determine whether eotaxins are associated with asthma and aspirin hypersensitivity, we compared the plasma levels of eotaxin-1, eotaxin-2, and eotaxin-3 at baseline in patients with AIA and ATA, before and after oral aspirin provocation. The results show that ATA patients have higher levels of eotaxin-1, eotaxin-2, and eotaxin-3 compared with those of healthy control subjects. In AIA patients, eotaxin-1 levels, but not those of eotaxin-2 or eotxin-3, were significantly elevated when compared with those of healthy control subjects. Considering that the frequency of aspirin intolerance is 5 to 10% of asthma patients, (17) our data suggest that each type of eotaxin may contribute to the development of asthma.
Eotaxin-1 has been relatively well-studied compared with eotaxin-2 and eotaxin-3 in terms of its biological role in asthma. The expression of eotaxin-1 messenger RNA and protein is increased in the bronchial epithelium and submucosal layer of the airways of patients with chronic asthma. Furthermore, the elevation of eotaxin-1 levels in those with asthma is proportional to eosinophil infiltration of the bronchi and bronchial hyperreactivity (25,26) as well as impaired lung function. (27,28) Athough eotaxin-1 is important for eosinophilic inflammation in the early phase of the asthmatic response, it does not account for the ongoing late asthmatic response. (29) A comparative studya (30) of the different roles of the three eotaxins showed that eotaxin-3, rather than eotaxin-1 or eotaxin-2, may account for eosinophil recruitment into asthmatic airways in the later stage of the asthmatic response. These data, together with those from our study, suggest that each of the three eotaxins may be involved at a certain stage of the development of asthma, especially ATA.
The present study also showed that AIA patients had different patterns of eotaxin-1, eotaxin-2, and eotaxin-3 expression in their plasma compared with those of ATA patients. The AIA group also had a higher level of plasma eotaxin-1, but not of eotaxin-2 and eotaxin-3, than did healthy control subjects. The elevation of basal levels of eotaxin-1 in AIA patients suggests a relationship between aspirin intolerance and eotaxin-1. To elucidate this relationship, we measured eotaxin levels before and after the aspirin challenge. There was no significant change in eotaxin-1, eotaxin-2, and eotaxin-3 levels between the two time intervals in the AIA and ATA groups, suggesting that eotaxin-1, eotaxin-2, or eotaxin-3 may not be related to the development of AIA.
One interesting finding is that the level of eotaxin-2 was higher in ATA patients than in patients with AIA before and after challenge (Fig 2, middle, B), indicating that eotaxin-2 may be associated with ATA rather than AIA. The plasma eotaxin-2 and eotaxin-3 levels and the peripheral blood eosinophil count may depend on the severity and acute exacerbation of asthma or on steroid treatment, as does the level of eotaxin-1. (9,31) Therefore, we selected study subjects with mild-to-moderate persistent asthma who did not experience an acute exacerbation and had not been treated with systemic steroids within 6 weeks before the study. The initial values of the FE[V.sub.1] percent predicted, P[C.sub.20], and percentage of eosinophils, and the incidence of atopy were comparable in the AIA and ATA groups (Table 1). These data indicate that the levels of eotaxins measured in our study were not biased by demographic characteristics. The limitation of our study is that the plasma levels of eotaxins may not reflect their concentrations in local tissues. In the nasal mucosa of aspirin-intolerant subjects, the synthesis of eotaxin-1 and eotaxin-2 is significantly higher (p < 0.05) than that in ATA patients. (32) A comparison of the levels of eotaxins in plasma and in airway secretions will provide insight into the role of eotaxins in the development of asthma and aspirin intolerance.
In summary, we showed that plasma eotaxin eotaxin-2 concentrations differed in asthmatic patients with respect to aspirin intolerance and tolerance, and that the concentrations were not changed by aspirin provocation, indicating that eotaxin-2 may be differentially up-regulated according to aspirin intolerance.
REFERENCES
(1) Szczeklik A, Stevenson DD. Aspirin-induced asthma: advances in pathogenesis, diagnosis, and management. J Allergy Clin Immunol 2003; 111:913-921
(2) Stevenson DD. Diagnosis, prevention, and treatment of adverse reactions to aspirin and nonsteroidal anti-inflammatory drugs. J Allergy Clin Immunol 1984; 74:617-622
(3) Szczeklik A, Virchow C, Schmitz-Schumann M. Pathophysiology, pharmacology of aspirin-induced asthma. In: Page CP, Barnes PJ, eds. Pharmacology of asthma: handbook of experhnental pharmacology. Berlin, Germany: Springer-Verlag, 1991; 291-314
(4) Nasser SM, Pfister R, Christie PE, et al. Inflammatory cell populations in bronchial biopsies from aspirin-sensitive asthmatic subjects. Am J Respir Crit Care Med 1996; 153:90-96
(5) Sampson AP, Cowburn AS, Sladek K, et al. Profound over-expression of leukotriene C4 synthase in bronchial biopsies from aspirin-intolerant asthmatic patients. Int Arch Allergy Immunol 1997; 113:355-357
(6) Daugherty BL, Siciliano SJ, DeMartino JA, et al. Cloning, expression, and characterization of the human eosinophil eotaxin receptor. J Exp Med 1996; 183:2349-2354
(7) Yang M, Hogan SP, Mahalingam S, et al. Eotaxin-2 and IL-5 cooperate in the lung to regulate IL-13 production and airway eosinophilia and hyperreactivity, J Allergy Clin Immunol 2003; 112:935-943
(8) Ponath PD, Qin S, Post TW, et al. Molecular cloning and characterization of a human eotaxin receptor expressed selectively on eosinophils, J Exp Med 1996; 183:2437-2448
(9) Park SW, Kim DJ, Chang HS, et al. Association of interleukin-5 and eotaxin with acute exacerbation of asthma. Int Arch Allergy Immunol 2003; 31:283-290
(10) Jose PJ, Griffiths-Johnson DA, Collins PD, et al. Eotaxin: a potent eosinophil chemoattractant cytokine detected in a guinea pig model of allergic airways inflammation. J Exp Med 1994; 179:881-887
(11) Garcia-Zepeda EA, Rothenberg ME, Ownbey RT, et al. Human eotaxin is a specific chemoattractant for eosinophil cells and provides a new mechanism to explain tissue eosinophilia. Nat Med 1996; 2:449-456
(12) Gareia-Zepeda EA, Rothenberg ME, Weremowicz S, et al. Genomic organization, complete sequence, and chromosomal location of the gene for human eotaxin (SCYA11), an eosinophil-specific CC chemokine. Genomics 1997; 41:471-476
(13) Nomiyama H, Osborne LR, Imai T, et al. Assignment of the human CC chemokine MPIF-2/eotaxin-2 (SCYA24) to chromosome 7q11.23. Genomics 1998; 49:339-340
(14) Guo RF, Ward PA, Hu SM, et al. Molecular cloning and characterization of a novel hmnan CC ehemokine, SCYA26. Genomics 1999; 58:313-317
(15) White JR, Imburgia C, Dul E, et al. Cloning and functional characterization of a novel human CC chemokine that binds to the CCR3 receptor and activates human eosinophils. J Leukoc Biol 1997; 62:667-675
(16) Patel VP, Kreider BL, Li Y, et al. Molecular and functional characterization of two novel human C-C chemokines as inhibitors of two distinct classes of myeloid progenitors. J Exp Med 1997; 185:1163-1172
(17) Ponath PD, Qin S, Ringler DJ, et al. Cloning of the human eosinophil ehemoattractant, eotaxin. Expression, receptor binding, and functional properties suggest a mechanism for the selective recruitment of eosinophils. J Clin Invest 1996; 97:604-612
(18) National Institutes of Health. Global strategy for asthma management and prevention: NHLBI/WHO workshop report; National Heart, Lung, and Blood Institute. Bethesda, MD: National Institutes of Health; Publication No. 2002-3659
(19) American Thoracic Society. Standards for the diagnosis and treatment of patients with chronic obstructive pulmonary disease (COPD) and asthma. Am Rev Respir Dis 1989; 136:225-244
(20) Chai H, Farr RS, Froehlich LA, et al. Standardization of bronchial inhalation challenge procedures. J Allergy Clin Immunol 1975; 56:323-327
(21) Park CS, Kim YY, Kang SY. Collection between RAST and skin test for inhalant offending allergens. J Kor Soc Allergol 1984; 3:1-9
(22) Stevenson DD, Simon RA. Sensitivity to aspirin and nonsteroidal anti-inflammatory drugs. In: Middleton E Jr, Reed CE, Ellis EF, et al. Allergy: principles and practice. 4th ed. St. Louis, MO: CV Mosby, 1993; 1751
(23) Kitaura M, Nakajima T, Imai T, et al. Molecular cloning of human eotaxin, an eosinophil-selective CC chemokine, and identification of a specific eosinophil eotaxin receptor, CC chemokine receptor 3. J Biol Chem 1996; 271:7725-7730
(24) Forssmann U, Uguccioni M, Loetscher P, et al. Eotaxin-2, a novel CC chemokine that is selective for the chemokine receptor CCR3, and acts like eotaxin on human eosinophil and basophil leukocytes. J Exp Med 1997; 185:2171-2176
(25) Ying S, Robinson DS, Meng Q, et al. Enhanced expression of eotaxin and CCR3 mRNA and protein in atopic asthma: association with airway hyperresponsiveness and predominant co-localization of eotaxin mRNA to bronchial epithelial and endothelial cells. Eur J Immunol 1997; 27:3507-3516
(26) Lamkhioued B, Renzi PM, Abi-Younes S, et al. Increased expression of eotaxin in bronchoalveolar lavage and airways of asthmatics contributes to the chemotaxis of eosinophils to the site of inflammation. J Immunol, 1997; 159:4593-4601
(27) Nakamura H, Weiss ST, Israel E, et al. Eotaxin and impaired lung function in asthma. Am J Respir Crit Care Med 1999; 160:1952-1956
(28) Taba RA, Laberge S, Hamid Q, et al. Increased expression of the chemoattractant cytokines eotaxin, monocyte chemotactic protein-4, and interleukin-16 in induced sputum in asthmatic patients. Chest 2001; 120:595-601
(29) Brown JR, Kleimberg J, Marini M, et al. Kinetics of eotaxin expression and its relationship to eosinophil accumulation and activation in bronchial biopsies and bronchoalveolar lavage (BAL) of asthmatic patients after allergen inhalation. Clin Exp Immunol 1998; 114:137-146
(30) Berkman N, Ohnona S, Chung FK, et al. Eotaxin-3 but not eotaxin gene expression is upregulated in asthmatics 24 hours after allergen challenge. Am J Respir Cell Mol Biol 2001; 24:682-687
(31) Lilly CM, Woodruff PG, Camargo CA Jr, et al. Elevated plasma eotaxin levels in patients with acute asthma. J Allergy Clin Immunol 1999; 104:786-790
(32) Pods R, Ross D, van Hulst S, et al. RANTES, eotaxin and eotaxin-2 expression and production in patients with aspirin triad. Allergy 2003; 58:1165-1170
Ji-Won Min; ([dagger]) An-Soo Jang, MD;([dagger]) Se-Min Park; Seung-Ha Lee; June-Hyuk Lee, MD; Sung-Woo Park, MD; and Choon-Sik Park, MD
* From the Division of Allergy and Respiratory Diseases, Genome Research Center for Allergy and Respiratory Diseases Soonehunhyang University, Bucheon Hospital, Gyeonggi Do,Korea.
([dagger])These authors contributed equally to this work.
This work was supported by a grant from the Korea Health 21 R&D Project, Ministry of Heath & Welfare, Republic of Korea (01-PJ3-PG6-01GN04-003).
Manuscript received February 11, 2005; revision accepted May 30, 2005.
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (www.chestjournal. org/misc/reprints.shtml).
Correspondence to: Choon-Sik Park, MD, Division of Allergy and Respiratory Medicine, Department of Internal Medicine, Soonchunhyang University Bucheon Hospital, 1174, Jung Dong, Wonmi Ku, Bucheon, Gyeonggi Do 420-021 Korea. e-mail: mdcspark@unitel.co.kr
COPYRIGHT 2005 American College of Chest Physicians
COPYRIGHT 2005 Gale Group