An 18-year-old Caucasian woman came to the emergency department with a pruritic rash and localized swelling, most marked in the periorbital area. The rash had started 5 days earlier on her upper lip and subsequently spread to her face and upper chest.
Two days before, the patient was treated with amoxicillin/clavulanate (Augmentin), prednisone, and hydroxyzine (Atarax), but her symptoms worsened. She said she felt feverish but did not have any visual disturbances. She had no contacts with others ill with herpes or Varicella, although she did admit to having an unprotected sexual encounter 2 weeks before the rash's onset. Her medical history was significant for untreated atopic dermatitis.
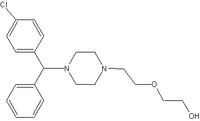
On exam, the patient was afebrile and had a diffuse maculopapular rash with areas of confluence over her face and hands (Figure 1). The face and hands also showed crusting and scaling. Discrete lesions were found on her upper and lower back (Figure 2), chest, volar wrist, and popliteal fossa. No vesicular lesions were present, although some isolated scabbed areas suggested previous vesicular lesions. The facial lesions were tender to palpation, and there was periorbital edema. No oral lesions were seen. Wound cultures grew methicillin-resistant Staphylococcus aureus.
[FIGURES 1-2 OMMITTED]
* WHAT IS THE DIAGNOSIS?
* HOW CAN THE DIAGNOSIS BE CONFIRMED?
* HOW SHOULD THIS DISEASE BE TREATED?
* DIAGNOSIS: ECZEMA HERPETICUM
Eczema herpeticum is an overwhelming herpesvirus infection on skin already affected by atopic dermatitis. It is a dermatologic emergency--untreated infections may lead to complications, including herpes keratitis and disseminated herpes simplex virus (HSV) infections with visceral involvement. Mortality is 1%-9%, (1) although before antiviral therapy it was as high as 75%. (2)
The rash begins as dome-shaped vesicles, which subsequently disappear and become punched-out excoriations, crusts, and erythematous plaques. The head, neck, and trunk are the most commonly affected areas. Systemic symptoms such as fever and malaise usually accompany the rash.
Causes of eczema herpeticum
The cause of eczema herpeticum is always HSV type I. (3) The exact pathophysiology is unknown, but it is thought to involve HSV entering the skin when skin barrier function is compromised due to dermatitis. Defective cytokine secretion in the affected skin also plays an important role. (3)
The severity of preexisting eczema does not seem to dictate the severity of eczema herpeticum. (4) Secondary bacterial skin infections are very common. A mixture of aerobic and anaerobic bacteria are commonly isolated, the most common being S aureus, Group A [beta]-hemolytic Streptococcus, Pseudomonas, and Peptostreptococcus. (6,7)
Risks
It is not clear which patients with atopic dermatitis are more at risk for developing eczema herpeticum. High total serum immunoglobulin E (IgE) and early age of onset are 2 risk factors that have been identified. (7,8)
Some researchers have suggested that use of topical corticosteroids predisposes those with atopic dermatitis to develop eczema herpeticum, but larger studies do not support this. (8) However, topical calcineurin inhibitors do seem to pose a higher risk and are thus contraindicated during an eczema herpeticum infection. (9)
* DIFFERENTIAL DIAGNOSIS
Kaposi's varicelliform eruption is a disseminated eruption of HSV on skin already affected with another dermatitis; eczema herpeticum refers specifically to the occurrence of an eruption on skin affected by atopic dermatitis. Thus, other types of Kaposi's varicelliform eruption should be considered in the differential diagnosis. These include HSV infections on skin affected by Darier-White disease, pemphigus foliaceus, and mycosis fungoides. A good history taken from the patient regarding coexisting skin disorders makes the difference clear.
Other generalized vesicular eruptions such as Varicella should also be considered before making the diagnosis. Since distinct vesicles are not often present by the time the patient presents for care, the rash may also be confused with impetigo or other bacterial infections.
* LABORATORY TESTS
Several tests are available to detect the presence of HSV in the skin lesions of eczema herpeticum. These include polymerase chain reaction (PCR), immunofluorescence, and electron microscopy. Electron microscopy is not widely available and PCR can take several days, so often it is helpful to do direct fluorescent antibody testing while PCR results are pending. Light microscopy can be used to do a Tzanck test, which looks for multinucleated giant cells in blister fluid.
Serologies are often ordered, but results are nonspecific. Viral cultures are not very sensitive and take a while to get results. Aerobic and anaerobic bacterial cultures should be done because superinfection is common.
* TREATMENT: SYSTEMIC ANTIVIRALS, ANTIBIOTICS
Systemic antiviral medications are the mainstay of treatment for eczema herpeticum. Before the advent of acyclovir, the mortality rate of eczema herpeticum was 75%. (2)
The nucleoside analogs, which work by inhibiting viral DNA replication, are the most commonly used antiviral agents. Most of the studies on the treatment of eczema herpeticum have been on acyclovir; a 7-day course of IV therapy is typical. Alternatives such as valacyclovir have also been shown to be effective and have better oral bioavailability. Topical antivirals are often used for prophylaxis of keratoconjunctivitis if lesions are found around eyelids.
Antibiotics are often necessary to treat bacterial superinfection. Topical or systemic corticosteroids are not generally recommended and may worsen disease by attenuating the immune response.
* PATIENT FOLLOW-UP
This patient was initially treated with levofloxacin (Levaquin) for a presumed diagnosis of dermatitis with bacterial superinfection. Vancomycin was added on hospital day 2 when the rash was not improving. Due to a high suspicion for eczema herpeticum, a direct fluorescent antibody test sent for herpes, When the test results came back positive, the patient was started on intravenous acyclovir. A HSV PCR also had positive results. An ophthalmology specialist found no evidence for herpes keratoconjunctivitis and made no further recommendations.
The patient responded to the treatment and was discharged on hospital day 5. She was given a 10-day course of valacyclovir and a 21-day course of levofloxacin to complete at home. The patient fully recovered from the acute infections with some residual scarring.
DRUG BRAND NAMES
Acyclovir * Zovirax
Amoxicllin/clavulanate * Augmentin
Hydroxyzine * Atarax
Levofloxacin * Levaquin
Valacyclovir * Valtrex
* SUBMITTING IMAGES TO PHOTO ROUNDS
Do you have images (slides, prints, digitized photos) of compelling clinical cases of interest to family physicians? We would like to publish them, along with a brieft description of the clinical presentation and a diagnostic question for readers. The case should include information on the differential diagnosis and treatment, the latter applying an evidence-based approach supported by current references. Submit electronic files to usatine@uthscsa.edu, or send high-quality slides and prints to:
Submissions: Richaed P. Usatine, Editor, Photo Rounds, University of Texas Health Sciences Center at San Antonio, Dept of Family and Community Medicine, MC 7794, 7703 Floyd Curl Drive, San Antonio, TX 78229-3900.
REFERENCES
(1.) Atherton DJ, Marshall WC. Eczema herpeticum. Practitioner 1982; 226:971-973.
(2.) Wollenberg A, Wetzel S, Burgdorf W, Haas J. Viral infections in atopic dermatitis: Pathogenic aspects and clinical management. J Allergy Clin Immunol 2003; 112:667-74.
(3.) Goodyear HM et al. Growth of herpes simplex type 1 on skin explants of atopic eczema. Clin Exp Dermatol 1996; 21:185-189.
(4.) Harindra V, Paffett MC. Recurrent eczema herpeticum: an underrecognised condition. Sex Transm Infect 2001; 77:76.
(5.) Brook I, Frazier EH, Yeager JK. Microbiology of infected eczema herpeticum. J Am Acad Dermatol 1998; 38:627-629.
(6.) Brook I. Secondary bacterial infections complicating skin lesions. J Med Microbiol 2002; 51:808-812.
(7.) Bork K, Brauninger W. Increasing evidence of eczema herpeticum: analysis of seventy-five cases. J Am Acad Dermatol 1988; 19:1024-1029.
(8.) Wollenberg A, Zoch C, Wetzel S, Plewig G, Przybilla B. Predisposing factors and clinical features of eczema herpeticum--a retrospective analysis of 100 cases. J Amer Acad Dermatol 2003; 49:198-205.
(9.) Wahn U, Bos JD, Goodfield M, Caputo R, Papp K, Manjra A, et al. Efficacy and safety of pimecrolimus cream in the long-term management of atopic dermatitis in children. Pediatrics 2002; 110:e2.
Correspondence: Larissa Buccolo, MD, Naval Hospital Family Practice Clinic, 2080 Child Street, Jacksonville, FL 32214. E-mail: L_S_Buccolo@sar.med.navy.mil.
Larissa S. Buccolo, MD
Family Practice Department, Naval Hospital, Jacksonville, Fla
COPYRIGHT 2004 Dowden Health Media, Inc.
COPYRIGHT 2004 Gale Group