Introduction
Most randomised controlled trials of treatment for hypertension in patients with diabetes have evaluated blood pressure lowering in comparison with a conventionally treated group of patients who had higher blood pressure.[1] These trials mainly used a single agent rather than comparing blood pressure lowering with different agents.
We reported results from the hypertension in diabetes study, part of the United Kingdom prospective diabetes study, in the accompanying paper.[2] Tight control of blood pressure with either an angiotensin converting enzyme inhibitor or [Beta] blocker resulted in a reduced risk of both macrovascular and microvascular complications in hypertensive patients with type 2 diabetes. The risk of any diabetes related end points was reduced by 24%, strokes by 44%, and microvascular end points by 37%.[2]
Studies with angiotensin converting enzyme inhibitors in hypertensive patients with type 1 diabetes have usually reported a decrease in unary albumin excretion,[3 4] and some have reported prevention of an increase in such excretion.[5-7] These studies have not assessed whether the reduction in albuminuria was due to blood pressure lowering or to the use of an angiotensin converting enzyme inhibitor in itself. Chan et al have suggested that enalapril may have a greater effect than nifedipine in reducing albuminuria,[8] but neither their study nor other studies have been sufficiently large or had long enough follow up to evaluate the effect of treatment on clinical complications.
Both angiotensin converting enzyme inhibitors and [Beta] blockers have been thought to have specific potential advantages. Studies of angiotensin converting enzyme inhibitors in diabetic patients have raised the possibility of a specifically beneficial effect in preventing microvascular disease in the kidneys. These agents are also effective in decreasing mortality from heart failure in non-diabetic subjects.[9] Treatment with [Beta] blockers has a protective effect on cardiac mortality after myocardial infarction,[10] and since this is the major cause of death in patients with type 2 diabetes prophylactic treatment with [Beta] blockers may be advisable. In addition, [Beta] blockers are effective in treating heart failure.[11]
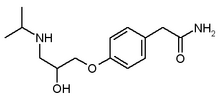
In this paper we report the results of a direct comparison of the treatment of hypertension in patients with type 2 diabetes with the angiotensin converting enzyme inhibitor captopril and the [Beta] blocker atenolol on the development of clinical complications of diabetes.
Subjects and methods
Hypertensive patients with type 2 diabetes were studied in the hypertension in diabetes study, which was introduced in a factorial design to the UK prospective diabetes study in 1987 to 20 of the 23 centres. Full details of this study, including the recruitment and randomisation procedure, are reported in the accompanying paper.[2] A total of 1148 patients (637 men (55%)) with a mean (SD) age of 56 (8) years were recruited for this study during 1987-91.[12] Table 1 shows the biometric and biochemical characteristics of patients at allocation to captopril or atenolol.
Table 1 Characteristics of patients allocated captopril or atenolol at time of randomisation to hypertension in diabetes study. Values are numbers (percentages) of patients unless stated otherwise
HDL=high density lipoprotein.
LDL=low density lipoprotein.
(*) Corrected to urinary creatinine concentration of 8 mmol/l.
Figure 1 in the accompanying paper shows that two thirds of the patients (758) were randomly allocated tight control of blood pressure aiming for a blood pressure of [is less than] 150/[is less than] 85 mm Hg by the coordinating centre; 400 patients were randomly allocated to captopril and 358 to atenolol.[2] The small imbalance in the numbers of patients allocated to these two treatments occurred by chance as the randomisation was not blocked. The other 390 patients were randomly allocated less fight control of blood pressure, aiming at a blood pressure of [is less than] 180/[is less than] 105 mm Hg but avoiding treatment with angiotensin converting enzyme inhibitors or [Beta] blockers.[2]
[Figure 1 ILLUSTRATION OMITTED]
Captopril was usually started at a dose of 25 mg twice daily, increasing to 50mg twice daily, and atenolol at a daily dose of 50 mg, increasing to 100 mg if required. If the blood pressure control criteria were not met in the tight control group despite maximum allocated treatment other agents were added, the suggested sequence being frusemide 20 mg daily (maximum 40 mg twice daily), slow release nifedipine 10mg (maximum 40 mg) twice daily, methyldopa 250 mg (maximum 500 mg) twice daily, and prazosin 1 mg (maximum 5 mg) thrice daily.
Clinical end points
Twenty one clinical end points were aggregated for analysis. The three predefined primary outcome analyses were the time to the occurrence of (a) a first clinical end point related to diabetes; (b) death related to diabetes; and (c) death from all causes. Four additional clinical end point aggregates were used to assess the effect of treatments on different types of vascular disease in secondary outcome analyses. These were myocardial infarction, stroke, amputation or death from peripheral vascular disease, and microvascular complications.
Subclinical, surrogate variables included urinary albumin concentration, with microalbuminuria defined as a concentration [is greater than or equal to]50mg/1 and clinical grade albuminuria as [is greater than or equal to]300 mg/1; retinopathy, with progression defined by a two step change in modified ETDRS (early treatment of diabetic retinopathy study) final grade assessed on retinal photographs; and visual acuity, with deterioration defined as a deterioration of three lines in the ability to read an ETDRS chart with the better eye.[2]
Primary analysis was on an intention to treat basis. Patients allocated to tight control of blood pressure with captopril were compared with those allocated to atenolol. Life table analyses were performed with log rank tests, and hazard ratios were obtained from Cox's proportional hazards models and used to estimate relative risks. For the primary and secondary outcome analyses of clinical end point aggregates, 95% confidence intervals are quoted. For single end points 99% confidence intervals are quoted to make allowance for potential type 1 errors. Similarly, 99% confidence intervals are used for assessment of surrogate variables that were measured at triennial visits. Mean (SD), geometric mean (1SD interval), or median (interquartile range) values have been quoted for the biometric and biochemical variables, using Wilcoxon, t, or [chi square] tests for comparison. Risk reductions were derived from frequency tables. Survival function estimates were calculated using the product limit (Kaplan-Meier) method. Blood pressure control was assessed in the cohort with nine years of follow up. Further details of the analyses used are described in the accompanying paper.[2]
Results
Blood pressure control
The patients allocated to captopril and to atenolol both had the same mean (SD) blood pressure 159 (20)/93 (10) mm Hg at randomisation to blood pressure control policy. Over nine years those allocated to captopril or atenolol had similarly reduced blood pressures, 144 (14)/83 (8) mm Hg and 143 (14)/81 (7) mm Hg respectively (fig 1). The differences (95% confidence interval) between the groups given captopril or atenolol were 1 (-1 to 3)/1 (0 to 2) mm Hg, with no significant difference for systolic pressure and a clinically small difference for diastolic pressure (P = 0.02). Those allocated to less tight consol of blood pressure, which did not include captopril or atenolol, had a mean blood pressure of 154 (16)/87 (7) mm Hg over nine years (fig 1).
Compliance with allocated treatment
Compliance was similar between the two groups over the first four years but subsequently more patients in the atenolol group than in the captopril group discontinued taking their allocated treatment (P [is less than] 0.0001). The difference in compliance was mostly because impaired peripheral circulation or bronchospasm occurred in the patients taking atenolol (table 2). Four per cent of patients allocated captopril discontinued the treatment because of a cough. Of the five patients in whom captopril was withdrawn because of a rise in creatinine concentration, one eventually required renal replacement, but the initial rise in creatinine had occurred before captopril treatment was started. During the study patients assigned captopril and atenolol took their treatment for 80% and 74% respectively of the total person years of follow up. Figure 2 shows that increasing numbers of blood pressure lowering agents were required to obtain the tight blood pressure control target of [is less than]150/[is less than]85mm Hg. A similar proportion of patients were taking three or more agents in the two groups (27% in the captopril group and 31% in the atenolol group). Nifedipine was used in 24% of person years of follow up in those allocated to less fight control of blood pressure, in 36% in those allocated to atenolol and 27% in those allocated to captopril.
[Figure 2 ILLUSTRATION OMITTED]
Table 2 Reasons for non-compliance with allocated treatment in group under tight control of blood pressure. Values are numbers (percentages) of patients; patients may have had more than one reason for not complying with allocated treatment
(*) At last clinic visit.
Primary outcome measures
The incidence of end points related to diabetes, which include macrovascular and microvascular complications, was similar in hypertensive patients with type 2 diabetes allocated to either captopril or atenolol treatment (figs 3 and 4). The incidence of diabetic deaths and all cause mortality was also similar in both groups (figs 4 and 5).
[Figures 3 & 5 ILLUSTRATION OMITTED]
Secondary outcome measures
Macrovascular disease
There was no difference in the incidence of myocardial infarction or strokes between the groups assigned [Beta] blocker or angiotensin converting enzyme inhibitor (figs 4 and 6). There were no differences in any of the single clinical end points, including heart failure and angina (fig 7). Neither was there a difference when all end points relating to macrovascular disease were aggregated.
[Figures 6 & 7 ILLUSTRATION OMITTED]
Microvascular disease
There was no difference in the incidence of aggregate microvascular clinical end points between the groups allocated [Beta] blocker or angiotensin converting enzyme inhibitor (figs 4 and 6). Similar proportions of patients required retinal photocoagulation, progressed to renal failure, or required an amputation, which can arise from a combination of macrovascular and microvascular disease.
Surrogate end points
Microvascular disease
Retinopathy--The progression of retinopathy was similar in those allocated to captopril and atenolol; at nine years 37% in the group assigned captopril (59/160) and 37% in that assigned atenolol (52/140) had deteriorated by two or more steps of retinopathy compared with 51% in the group assigned to less tight control of blood pressure (78/152). There was no difference between the captopril and atenolol groups in the deterioration of visual acuity by one letter on the ETDRS chart reduction.
Renal failure--The progression of albuminuria was similar in those allocated to captopril and atenolol. The proportion of patients who at nine years had a urinary albumin concentration [is greater than or equal to] 50 mg/1 were 31% (48/153) and 26% (38/146) (P = 0.31) and who had clinical proteinuria [is greater than or equal to]300mg/1 were 5% (7/153) and 10% (14/146) (P=0.090) respectively. There was also no difference in plasma creatinine concentrations or in the proportion of patients who had a twofold increase in creatinine concentration from randomisation. The surrogate indices of neuropathy and autonomic neuropathy were not different between the allocations.
Macrovascular disease
There was no difference in the proportion of patients who developed a silent infarction, shown in an electrocardiogram. Similarly, there was no difference in non-specific T waves or ST abnormalities, cardiomegaly assessed by electrocardiography or chest radiography, or peripheral vascular disease assessed by Doppler blood pressure recordings or absent peripheral pulses (data not shown).
Other treatment effects
Glycated haemoglobin (haemoglobin [A.sub.1c])--Over the first four years of follow up the patients allocated to atenolol had a higher mean glycated haemoglobin (haemoglobin [A.sub.1c]) concentration than those allocated captopril (7.5% (1.4%) v 7.0% (1.4%), P=0.0044), although over the second four years the values were similar (8.4% (1.5%) and 8.3% (1.7%) respectively). After four years of follow up 66% of the patients allocated to atenolol were receiving an additional glucose lowering treatment since randomisation compared with 53% in those allocated to captopril (P = 0.0015). This difference was also present at eight years, with 81% and 71% respectively requiring an additional treatment (P = 0.029).
Hypoglycaemia-There was no overall difference in the rates of hypoglycaemia in the captopril and atenolol groups. In patients allocated to and taking angiotensin converting enzyme inhibitors and [Beta] blockers and those in the group assigned to less tight control of blood pressure the cumulative proportions of patients who reported minor or major hypoglycaemic reactions were 41%, 41%, and 43% respectively and in those who reported a major hypoglycaemic episode 6.5%, 5.6%, and 4.4%. There were no fatal hypoglycaemic events in patients allocated to these treatments.
Weight gain--The patients allocated to atenolol gained more weight than those allocated to captopril (mean weight gain 3.4 (8.0) kg v 1.6 (9.1) kg over nine years, P = 0.020).
Lipid concentrations--There were no consistent trends in concentrations of triglyceride, total cholesterol, or high density lipoprotein cholesterol over nine years.
Discussion
Our accompanying paper showed that tight control of blood pressure with either captopril or atenolol in hypertensive patients with type 2 diabetes significantly reduced the risk of fatal and non-fatal macrovascular and microvascular complications over nine years of follow up.[2] This paper compares, within the patients allocated to tight blood pressure control, captopril and atenolol. Both treatments reduced blood pressure to the same extent and were similarly effective in reducing the risk of macrovascular and microvascular complications of diabetes.
Microvascular disease
These results are interesting given the current debate over whether any specific class of antihypertensive agents, and angiotensin converting enzyme inhibitors in particular, might be more effective than others in protecting against renal disease.[1 13 14] In this study the proportion of patients who developed albuminuria [is greater than or equal to] 50 mg/1, proteinuria ([is greater than or equal to] 300 mg/l), a twofold increase in plasma creatinine concentration, end stage renal failure, or progression of retinopathy was similar in the groups assigned captopril or atenolol.
The increase in plasma creatinine concentration, which led to captopril treatment being withdrawn in five patients, may have been partially due to unrecognised renal artery stenosis, which seems to be particularly common in type 2 diabetes.[15] Nevertheless, none of these patients developed acute renal failure, and in the one who developed chronic renal failure and eventually required dialysis the initial increase in plasma creatinine concentration had happened before the introduction of captopril. Moreover, mean plasma creatinine concentration as well as the incidence of renal failure was similar in the captopril and atenolol groups. Contrary to recent suggestions,[16] our data do not support the need for routine screening with imaging techniques for renal artery stenosis of patients with type 2 diabetes before the introduction of angiotensin converting enzyme inhibitors, although measurement of plasma creatinine concentration before and after the start of treatment remains advisable.
Macrovascular disease
The patients allocated to either captopril or atenolol had a reduced risk of death related to diabetes and stroke compared with the group assigned to less tight control of blood pressure. The incidence of myocardial infarction and of heart failure was similar in the captopril and atenolol groups. The negative inotropic effect of [Beta] blockers might have been expected to increase the incidence of heart failure, but the protection against heart failure was as great for atenolol as for captopril. This suggests that the beneficial effect of [Beta] blockade on autonomic control of ventricular function and myocardial energy balance predominated.[17] A trend to fewer sudden deaths with the [Beta] blockers than with the angiotensin converting enzyme inhibitor was not significant.
A specific beneficial effect of angiotensin converting enzyme inhibitors in diabetic patients has been questioned in an extensive review, which found no evidence for it.[13] The similar effect of captopril and atenolol on clinical end points suggests either that both [Beta] blockers and angiotensin converting enzyme inhibitors have specific beneficial effects or that the decrease in blood pressure is the important factor and not the type of treatment. The diabetic subgroup of the systolic hypertension in the elderly programme also showed prevention of myocardial infarction by blood pressure lowering, the initial treatment being a thiazide (chlorthalidone), with 20% of patients also taking atenolol.[18]
In the hypertension in diabetes study the use of a long acting calcium antagonist, nifedipine, was recommended as the second blood pressure lowering agent in the group assigned to less tight control of blood pressure and as the third agent in the group assigned to fight control. In view of the possibility, as yet unproved, of an increased risk of myocardial infarction in type 2 diabetes with a calcium channel blocker compared with an angiotensin converting enzyme inhibitor,[17] we noted that nifedipine was used in 24% of person years of follow up in those allocated to less fight control of blood pressure, 36% in those allocated to atenolol, and 27% in those allocated to captopril. As the group assigned to tight blood pressure control had a trend to a reduced risk for myocardial infarction compared with the group assigned to less tight control, the data do not support the contention that calcium channel blocking agents are potentially harmful.[18]
Side effects
The development of cold feet, intermittent claudication, or bronchospasm in some patients was the main reason for the slightly lower rate of compliance for atenolol. However, a similar proportion of patients assigned the two drugs developed peripheral vascular disease, had absent foot pulses on examination, or had amputations.
The patients given atenolol gained 1.8 kg more weight than those given captopril over nine years, and they had higher glycated haemoglobin concentrations over the first four years.
These surrogate indices of risk of macrovascular disease have been thought to be potentially harmful, but in practice results from this study show that those allocated to atenolol had a reduced risk of cardiac events.
Choice of antihypertensive agents
Angiotensin converting enzyme inhibitors have been recommended for treatment of hypertension in type 1 or type 2 diabetes on the basis of studies showing a reduction in urinary albumin concentration or prevention of an increase in urinary albumin concentration in comparison with untreated control groups. In most studies patients treated with angiotensin converting enzyme inhibitors had a lower blood pressure than the control group,[19 20] and this alone may have been the main factor in decreasing capillary perfusion, reducing transcapillary leakage of albumin, arid, in the long term, decreasing the damage to both capillaries and arteries. Similarly, studies of angiotensin converting enzyme inhibitors in patients with normal blood pressure have evaluated patients whose blood pressures are in the upper range of normal values, although not above an arbitrary definition of hypertension?[5 19] The small decrease in blood pressure in the group given angiotensin converting enzyme inhibitors may have been sufficient to decrease urinary albumin excretion. Lewis et al studied diabetic patients with nephropathy and reported that an angiotensin converting enzyme inhibitor decreased progression to end stage renal failure and delayed the increase in plasma creatinine concentration.[21] However, the results may have been confounded because the group given angiotensin converting enzyme inhibitors also had lower blood pressures than the control group and urinary albumin excretion was mismatched at baseline. Although some studies have discounted the minor difference in blood pressure attained with angiotensin converting enzyme inhibition in normotensive patients,[19] small differences in blood pressure can affect cardiac and stroke outcome, both in the general population[22 23] and in patients with type 2 diabetes.[2] This suggests that it may be advantageous to treat even slight increases in blood pressure.
In conclusion, this paper shows that atenolol and captopril are equally effective and safe in lowering blood pressure and reducing the risk of fatal and nonfatal macrovascular and microvascular complications in patients with type 2 diabetes.
We appreciate the cooperation of the patients and many NHS and non-NHS staff at the participating centres.
Contributors: Details of participating staff and the supervising committees are listed in the accompanying paper.[2]
Funding: The main grants for this study were from the Medical Research Council, British Diabetic Association, the Department of Health, the National Eye Institute and the National Institute of Digestive, Diabetes and Kidney Disease in the National Institutes of Health in the United States, the British Heart Foundation, Novo-Nordisk, Bayer, Bristol Myers Squibb, Hoechst, Lilly, Lipha, and Farmitalia Carlo Erba. Other funding companies and agencies are listed in the accompanying paper.[2]
[1] Kasiske B, Kalil RSN, Ma JZ, Liao M, Keane WF. Effect of antihypertensive therapy on the kidney in patients with diabetes: a meta-regression analysis. Ann Intern Med 1993; 118:129-38.
[2] UK Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. BMJ 1998;317:703-13.
[3] Passa P, Leblanc H, Marre M. Effects of enalapril in insulin-dependent diabetic subjects with mild to moderate uncomplicated hypertension. Diabetes Care 1987;10:200-4.
[4] Laffel LM, McGill JB, Gans DJ. The beneficial effect of angiotensin-converting enzyme inhibition with captopril on diabetic nephropathy in normotensive IDDM patients with microalbuminuria. North American Microalbuminuria Study Group. Am J Med 1995;99:497-504.
[5] Marre M, Chatellier G, Leblanc H, Guyene TT, Menard J, Passa P. Prevention of diabetic nephropathy with enalapril in normotensive diabetics with microalbuminuria. BMJ 1988;297:1092-5.
[6] EUCLID Study Group. Randomised placebo-controlled trial of lisinopril in normotensive patients with insulin-dependent diabetes and normoalbuminuria or microalbuminuria. Lancet 1997;349:1787-92.
[7] Hjelm M, Mathiesen E. Efficacy of captopril in postponing nephropathy. BMJ 1991;303:469.
[8] Chan JCN, Cockram CS, Nicholls MG, Cheung CK, Swaminathan R. Comparison of enalapril and nifedipine in treating non-insulin dependent diabetes associated with hypertension: one year analysis. BMJ 1992;305:981-5.
[9] Garg R, Yusuf S. Overview of randomized trials of angiotensin-converting enzyme inhibitors on mortality and morbidity in patients with heart failure. Collaborative Group on ACE Inhibitor Trials. JAMA 1995;273:1450-6.
[10] Yusuf S, Peto R, Lewis J, Collins R, Sleight P. Beta blockade during and after myocardial infarction: an overview of the randomised trials. Progr Cardiovascular Dis 1985;27:335-71.
[11] Heidenreich PA, Lee TT, Massie BM. Effect of beta-blockade on mortality in patients with heart failure: a meta-analysis of randomized clinical trials. J Am Coll Cardiol 1997;30:27-34.
[12] Hypertension in Diabetes Study Group HDS 3: prospective study of therapy in type 2 diabetic patients--efficacy of ACE inhibition and [Beta]-blockade. Diabet Med 1994; 11:773-82.
[13] Sawicki PT. Do ACE inhibitors offer specific benefits in the antihypertensive treatment of diabetic patients? Diabetologia 1998;41:598-602.
[14] Cooper ME. Pathogenesis, prevention and treatment of diabetic nephropathy. Lancet 1998;352:213-9.
[15] Sawicki PT, Kaiser S, Heinemann L, Frenzel H, Berger M. Prevalence of renal artery stenosis in diabetes mellitus--an autopsy study. J Intern Med 1991 ;229:489-92.
[16] Kumar A, Asim M, Davison AM. Taking precautions with ACE inhibitors. BMJ 1998;316:1921.
[17] Andersson B, Caidahl K, diLenarda A, Warren SE, Goss F, Waldenstrom A, et al. Changes in early and late diastolic filling patterns induced by long-term adrenergic beta-blockade in patients with idiopathic dilated cardiomyopathy. Circulation 1996;94:673-82.
[18] Curb JD, Pressel SL, Curler JA, Savage P, Applegate WB, Black H, et al. Effect of diuretic-based antihypertensive treatment on cardiovascular disease risk in older diabetic patients with isolated systolic hypertension. Systolic Hypertension in the Elderly Program Cooperative Research Group. JAMA 1996;276:1886-99.
[19] Ravid M, Savin H, Jutrin I, Bental T, Lang R, Lishner M. Long-term effect of ACE inhibition on development of nephropathy in diabetes mellitus type IL Kidney Int 1994;45(suppl):S 161-4.
[20] Lebovitz HE, Wiegmann TB, Cnaan A, Shahinfar S, Sica DA, Broadstone V, et al. Renal protective effects of enalapril in hypertensive NIDDM: role of baseline albuminuria. Kidney Int 1994;45(suppl):S 150-5.
[21] Lewis EJ, Hunsicker LG, Bain RP, Rohde RD. The effect of angiotensin-converting-enzyme inhibition on diabetic nephropathy. N Engl J Med 1993, 329:1456-62.
[22] Collins, Peto R, MacMahon S, Herbert P, Fiebach NH, Eberlein KA, et al. Blood pressure, stroke and coronary heart disease. Part 2. Short-term reductions in blood pressure: overview of randomised drug trials in their epidemiological content. Lancet 1990;335:827-38.
[23] Collins R, MacMahon S, Blood pressure, antihypertensive drug treatment and the risks of stroke and of coronary heart disease. Br Med Bull 1994;50:272-98.
(Accepted 20 August 1998)
RELATED ARTICLE: Key messages
* This study showed that an angiotensin converting enzyme inhibitor (captopril) or a [3 blocker (atenolol) gave similar reductions in blood pressure in hypertensive patients with type 2 diabetes
* To achieve target blood pressures additional antihypertensive agents were often required
* The two drugs were equally effective in reducing the risk of non-fatal and fatal diabetic complications, death related to diabetes, heart failure, and progression of retinopathy
* Those given atenolol gained slightly more weight and showed a slightly greater increase in glycated haemoglobin concentrations, but this did not affect the reduction in clinical end points
* The suggestion that angiotensin converting enzyme inhibitors have a specific renal protective effect in the treatment of type 2 diabetes is not supported
COPYRIGHT 1998 British Medical Association
COPYRIGHT 2000 Gale Group