The length of human pregnancy is variable, reflecting the advantages to the fetus, which would benefit by staying in the uterus to grow more, and to the mother, for whom earlier delivery might reduce pelvic damage (see the second article in the series). The result of this interaction is a relatively high incidence of premature deliveries. In the United Kingdom the incidence of preterm delivery (before 37 weeks) is about 7%, and in many developing countries, it is much higher. The baby is delivered before its homeostatic mechanisms are properly developed and so is prone principally to the respiratory distress syndrome, hypothermia, hypoglycaemia, and jaundice.
Causes
Socioeconomic factors influence the incidence of preterm labour. Preterm birth is significantly more common in young women, those with low body weight (body mass index [is less than] 19), those of lower social class, unmarried or unsupported mothers, and smokers. Some medical factors may increase the risk of preterm birth--for example, previous preterm delivery, persistent vaginal bleeding in early pregnancy, and heart disease. Cervical incompetence is a rare cause of preterm labour, sometimes preventable by cervical cerclage (a purse string suture around the cervix as close to the internal os as possible). The Medical Research Council's trial showed a small but significant benefit from this procedure, even in women with equivocal risk factors.
Risk factors for preterm labour
* Young age of mother ([is less than or equal to] 15 years)
* Lower socioeconomic class
* Unmarried or unsupported
* Underweight
* Cigarette smoking
* Previous preterm baby
* Multiple pregnancy
* Cervical incompetence
* Premature rupture of the membranes
Infection, usually chorioamnionitis, is a significant component in many cases of spontaneous preterm labour. The ascent of any organism through the cervical mucus plug into the uterus stimulates an inflammatory reaction in the placenta, fetal membranes, and maternal decidua. This leads to the release of cytokines such as interleukin 1 [Beta] and interleukin 6 from endothelial cells and tumour necrosis [Alpha] from macrophages. These stimulate the cascade of prostaglandin production, which in turn produces cervical ripening and uterine contractions. The commonest groups of organisms are the streptococci, mycoplasmas, and fusiform bacilli. Bacterial vaginosis (Gardnerella vaginalis) associated with a vaginal pH value of 5.4 seems to promote preterm labour, possibly reducing the efficiency of the cervical barrier to infection. Preliminary studies suggest that treatment with metronidazole or clindamycin in women with bacterial vaginosis may reduce the incidence of preterm labour, and prospective studies are under way.
Major risks of early preterm delivery
* Death
* Respiratory distress syndrome
* Hypothermia
* Hypoglycaemia
* Necrotising enterocolitis
* Jaundice
* Infection
* Retinopathy of prematurity
Major causes of preterm labour
* Iatrogenic (induction for medical reasons)
* Infection
* Premature rupture of the membranes
* Multiple pregnancy
* Polyhydramnios
* Intrauterine death
* Fetal abnormalities
* Uterine abnormalities
* Cervical incompetence
About 30% of preterm births are iatrogenic--that is, induced by obstetricians for maternal indications such as fulminating pre-eclampsia or for fetal indications such as severe intrauterine growth restriction. In recent years, since the increased use of assisted reproduction, multiple pregnancy has become a growing cause of preterm labour. The incidence of fetal abnormality is higher in pregnancies complicated by preterm labour.
Diagnosis of preterm labour
The precise diagnosis of preterm labour is not easy. The only absolute proof is progressive dilatation of the cervix, but once this has happened, it is too late to attempt preventive treatment. The finding of fetal fibronectin, a fetal protein involved in cell to cell adhesion, in vaginal secretions suggests that the cervical mucus plug is becoming ineffective. This has been proposed as a sensitive screen for preterm labour, but its poor specificity, together with a relatively high false positive rate, makes it unsuitable for routine use.
The diagnosis of labour often has to be made on the basis of reported uterine contractions. However, Braxton Hicks contractions are noticed in most pregnancies from about 24 weeks' gestation onwards, and many women find these painful. This means that the diagnosis of preterm labour is often wrong; two thirds of women diagnosed as being in labour will not have delivered within 48 hours, and over one third go to term. Diagnosis with home uterine contraction monitoring has been tested in a number of trials, but no consensus on its value has emerged.
Diagnosis remains essentially clinical, with a careful history and a speculum examination being important components. Abdominal pain of any type, or any vaginal bleeding, requires a careful speculum examination of the cervix. Digital examinations should be avoided if there is any suggestion of ruptured membranes as they increase the risk of ascending infection. Seeing amniotic fluid trickling through the cervix remains the only certain way of diagnosing ruptured membranes. The use of an acidity indicator, such as nitrazine sticks (Amnicator, Corsham), is not reliable, as this indicates only that the vagina is no longer acid, an effect that can be produced by urine or bath water.
When examining the cervix, a vaginal swab should be taken for culture. This will enable appropriate antibiotic treatment if signs of infection develop later.
Management
Tocolysis
Suppression of uterine contractions would seem to be the obvious solution to the problem of preterm labour. However, tocolytic agents do not work effectively for longer than about 48 hours, probably because of tachyphylaxis. Their major use is to postpone delivery--for example, for in utero transfer to a tertiary centre--or to allow the administration of corticosteroids to the mother and so to her fetus to promote surfactant release in the fetal lung and reduce the incidence of the neonatal respiratory distress syndrome by up to 50%. This effect is only significant at gestations up to 34 weeks; after this it is usual to allow preterm labour to progress.
However, there are many situations in which the use of tocolytics is inappropriate. In a typical maternity unit, delivering about 3000 women a year, only about 50 women a year will be suitable for tocolysis (about one a week).
Many tocolytics are currently used. Sympathomimetics such as ritodrine and salbutamol are generally the safest choice for the mother and fetus, although they can cause tachycardia and pulmonary oedema if given in overdose. Indomethacin can be used before 32 weeks, and because it restricts fetal urine output it is useful if there is polyhydramnios. However, it may cause premature closure of the fetal ductus arteriosus if used after 32 weeks' gestation, which can lead to significant pulmonary hypertension. Alcohol and isoxuprine hydrochloride are no longer used, while calcium channel blockers cause significant hypotension. Atosiban, an oxytocin antagonist, shows promise, as does nimesulide, a selective cyclo-oxygenase type 2 inhibitor. Nitric oxide donors such as glyceryl trinitrate are also being evaluated. No evidence exists that prophylactic tocolytics, given orally throughout the first and second trimesters of pregnancy, are of benefit.
When the membranes have ruptured, the use of tocolytics is controversial. The concern is that contractions may result from occult chorioamnionitis, and suppressing labour could allow infection to spread. If tocolytics are used in this situation--for example, to allow transfer of the baby in utero to a tertiary centre--intravenous broad spectrum antibiotics should probably also be given. The routine administration of antibiotics with ruptured membranes has not been proved to be valuable and is currently the subject of the ORACLE trial. Most cases will be managed conservatively, with labour being induced at 36 weeks. Close observation for signs of a developing infection is mandatory; monitoring of maternal temperature, white blood cell count, and blood concentrations of C reactive protein is usual. In the United States amniocentesis is sometimes used to screen for occult infection but has not been shown to be effective in prospective trials and is rarely performed in Britain. Re-examinations of the vagina should be avoided, as they increase the risk of infection.
Antenatal steroids
Meta-analyses of the use of tocolytics suggest that they have little effect on perinatal mortality. However, they do allow time for the administration of antenatal steroids, which, if given at least 24-48 hours before birth, can halve the incidence and severity of respiratory distress and mortality in newborn infants. The effect of steroids lasts up to about a week. The benefit of repeated doses of steroids to the fetus has not been shown; their safety and efficacy needs to be tested in a prospective trial.
Preterm delivery
The preferred method of delivery in preterm labour depends on the fetal presentation and the stage of gestation. If the baby is presenting by the head, then vaginal delivery is probably safe in most cases, with caesarean delivery being performed only for the usual obstetric indications. In a breech presentation before 32 weeks it is possibly safer for the baby to be delivered by cesarean section. This, however, considerably raises the risk to the mother as in many cases the operation is not straightforward because the lower segment may not be well formed.
The preterm baby
The conditions into which the baby is born have a major influence on its chance of survival. Very preterm babies (those born at less than 28 weeks) do best when delivered in a tertiary referral centre with a neonatal intensive care unit. Deliveries should be conducted by experienced midwives or obstetricians, with an experienced paediatrician present. The delivery room should be warm, and there should be adequate equipment for resuscitation (see final article in this series). If preterm labour starts at home, or in a smaller hospital, transfer of the mother in early labour should be considered, for the mother is the ideal incubator. However, in some cases the mother is also unwell--for example, with high blood pressure--and her condition must be taken into account. In one study 17% of such mothers ended their transfer in the adult intensive care unit. Care must be taken to stabilise maternal condition before transfer. Transfer is probably unwise if labour is progressing rapidly or there is substantial vaginal bleeding.
Modern neonatal intensive care means that babies delivered after 30 weeks' gestation usually survive intact. However, babies delivered between 23 and 24 weeks' gestation have an increased risk of long term handicap. With babies at the limit of viability (23-24 weeks), both a paediatrician and an obstetrician should, whenever possible, discuss management with the parents, as the likelihood of handicap may exceed 50%.
Tocolytics
Currently used
* [Beta] sympathomimetics, such as ritodrine, terbutaline, salbutamol
* Magnesium sulphate (used particularly in the United States)
* Prostaglandin synthase inhibitors, such as unselective (indomethacin) and selective (cyclo-oxygenase type 2 nimesulide)
* Nitric oxide donors, such as glyceryl trinitrate
* Calcium channel blockers, such as nifedipine
No longer used
* Alcohol
* Isoxuprine
The ORACLE study
* This multicentre study is investigating the usefulness of antibiotics when membranes rupture prematurely--particularly, whether they reduce the risk of early preterm labour and improve the baby's chances of survival
* The antibiotics being used in the study are Augmentin and erythromycin
* Women take the antibiotics (or placebo) for 10 days or until the birth of their baby, whichever is the shorter time
Philip Steer is professor of obstetrics and consultant obstetrician at the Imperial College School of Medicine, Chelsea and Westminster Hospital, London; Caroline Flint is honorary professor at Thames Valley University and an independent midwife in London.
The ABC of Labour Care is edited by Geoffrey Chamberlain, emeritus professor of obstetrics and gynaecology at the Singleton Hospital, Swansea. It will be published as a book in the summer.
Conclusion
* Preterm labour needs careful management in centres with staff skilled in this field
* Antenatal steroids are of significant benefit and should always be given
* Discussion about prognosis and plans for delivery must include the pediatricians
Incidence of multiple pregnancy per 1000 multiple births in United Kingdom
All multiple pregnancy births increased about 1.4-fold; triplets increased threefold.
Accuracy of fibronectin testing in prediction of preterm delivery: meta-analysis of 723 symptomatic and 847 asymptomatic women. Values are probability percentages, unless stated otherwise; values in parentheses are 95% confidence intervals
Likelihood ratio = the probability of a positive (or negative) result among women with a preterm delivery compared with the probability of such a result in those without a preterm delivery.
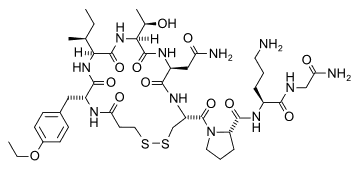
[ILLUSTRATION OMITTED]
Key references
* Morrison J, Rennie J. Aspects of fetal and neonatal care at extreme preterm periods of gestation. Br J Obstet Gynaecol 1997; 104:1341-50.
* Royal College of Obstetricians and Gynaecologists. Beta agonists for the care of women in preterm labour. London: RCOG, 1997. (Guideline No 1A.)
* Royal College of Obstetricians and Gynaecologists. Antenatal corticosteroids to prevent RDS. London: RCOG, 1996. (Guideline No 7.)
The box listing potential neonatal hazards of antenatal steroids is based on an article by Quinlivan et al (Aust NZ J Obstet Gynaecol 1998;38:1-7). The table on fibronectin testing is adapted from Chien P et al (Br J Obstet Gynaecol 1997;104:436-44). The graph of distribution of deliveries by gestational age is adapted from Gardosi et al (Br J Obstet Gynaecol 1997;104:792-7). The histogram from the cerclage trial is adapted from the MRC/RCOG Working Party (Br J Obstet Gynaecol 1993; 100:516-23). The chart showing use of tocolysis is adapted from Tucker et al (Obstet Gynecol 1991 ;77:343-7). The graph showing the meta-analysis of prophylactic betamimetics in pregnancy is adapted from Keirse (Cochrane Pregnancy and Childbirth Database; Oxford: Update Software, 1995). The graph showing the meta-analysis of effect of corticosteroids before delivery is adapted from Crowley (Cochrane Pregnancy and Childbirth Database; Oxford: Update Software, 1995). The graph of caesarean delivery is adapted from Grant et al (Br J Obstet Gynaecol 1996;103:1197-200). The bar chart showing survival rates is adapted from Emsley et al (Arch Dis Childhood 1998;78:F99-104). The photograph of the neonatal unit was taken by Douglas Neil, medical photographer at the Singleton Hospital.
COPYRIGHT 1999 British Medical Association
COPYRIGHT 2000 Gale Group