Atropine hypersensitivity is a rarely reported condition. However, in the military environment, such reactions are of significant concern given the threat of chemical warfare and the use of atropine as a nerve agent antidote. Upon deployment to regions where chemical attacks are a threat, each service member is issued three 2-mg intramuscular autoinjectors of atropine for self-treatment. In the case presented here, an active duty service member presented to his Aid Station to request red dog tags for a previously identified allergy to atropine. Sensitivity testing revealed a significant reaction to
Introduction
Atropine allergy or sensitivity is a rarely recognized condition that has serious implications for military deployability and suitability. Through increased awareness, alternative treatments or standard policy could be developed for military members with atropine sensitivity that face chemical warfare threats.
Case Report
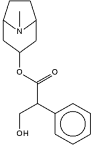
A 21-year-old Caucasian man presented to his military medical facility to request red dog tags for his reported allergy to atropine. Upon questioning, the patient reported that at the age of 7, he underwent a routine dilated eye examination while living in the Ukraine. Approximately 20 minutes after his eyes were dilated, the patient reported that he began shaking and became unresponsive. At that time, he was taken to the emergency room for monitoring, and no resuscitation was required. After the event, the patient was told he was allergic to the atropine in the eye drops. As a result of ongoing training and increased media coverage of the threat of chemical weapons before a deployment in support of Operation Enduring Freedom, the military member recognized the importance of atropine in the treatment of nerve agent poisoning and requested red dog tags to avoid inadvertent exposure to the drug. Because of the unusual nature of the described reaction and the implications for military service, further investigation was initiated. The patient was referred to an allergist, where an atropine challenge was performed in a monitored setting. The patient was prick tested with 0.01% atropine followed by 0.1%, with negative results. Incremental intradermal testing of 0.01% atropine and 0.1% initially resulted in an irritant skin reaction. However, within 15 minutes of the final 0.1% intradermal test, the patient began to experience signs of atropine poisoning that included twitching, flushed skin, dilated pupils, tachycardia, rapid deep breathing, and altered sensorium. He recovered after the administration of 3 mg of physostigmine.
It is estimated that the patient received a total of 0.02 to 0.03 mg of atropine during the test, and therapeutic doses for a chemical attack can exceed 5 mg. Therefore, in a chemical warfare environment where nerve agents are used, this military member is at risk from both the nerve agent and its antidote.
Discussion
The above case demonstrates that very small doses of atropine can result in severe adverse reactions in sensitive individuals. Adverse reactions after administration of subtherapeutic doses of medications are likely allergic or idiosyncratic. In this case, the reaction appears to be idiosyncratic because the patient exhibited signs and symptoms of atropine toxicity at doses approximately 100 times less than the usual therapeutic dose after nerve agent exposure. The reaction resolved with physostigmine, an acetycholinesterase inhibitor, and did not require the administration of epinephrine or other usual treatments for anaphylaxis.
Idiosyncratic "Toxic" Reactions
Gallasch et al.1 described 31 pediatric patients who developed local and systemic signs of atropine toxicity after the administration of atropine eye drops for the purpose of assessing refraction. Systemic signs included increased temperature and diffuse dry red skin. Two patients developed periorbital dermatitis. In all cases, skin testing was negative for atropine allergy, and local and systemic toxic effects to relatively low doses of atropine in eye drops was suspected.
Case reports suggest a wide variation in physiologic response to atropine when administered to a large population. A report in the ophthalmology literature described a toxic reaction in a child resembling the reaction in this case, although it was likely due to a larger dose much closer to the toxic range.2 However, a widely variable toxic range is noted in their review, with an average lethal dose after eye drop instillation of about 100 mg (200 drops of 1% atropine), but there was also a case report of one patient recovering after a parenteral 1-g dose. In a survey of South Carolina ophthalmologists, one case of fever, two episodes of acute asthma exacerbation, and one seizure were noted after atropine instillation in the office setting over a 2-year period.3 Assuming no accidental overadministration, these cases demonstrate the capability of a therapeutic dose to cause symptoms consistent with atropine overdose in sensitive individuals. Cases demonstrating similar hypersensitivity to perioperative therapeutic parenteral doses of atropine have been described, including one incident where a patient developed tachycardia, hypertension, vision disturbance, mydriasis, and a central nervous system (CNS) disturbance that responded to neostigmine.4
Allergic Reactions
Although this patient did not appear to have a true allergic reaction, actual allergy to atropine-containing preparations has been described. Decraene et al,5 described a patient that developed a red, swollen eye accompanied by an id-like dermatitis over the entire body 1 day after ophthalmologic surgery. Patch testing revealed positive reaction to atropine and other mydriatic agents containing structural homologs to atropine. Six other patients with similar reactions were observed retrospectively. None developed systemic noncutaneous symptoms. In another report, a patient was found to have marked local sensitivity to atropine and homatropine without systemic toxicity after developing severe periorbital dermatitis after eye drop administration.6
In addition to local reactions, generalized anaphylactic reactions to atropine administration have been reported, albeit rarely.7 Such reactions may occur due to additives. Specifically, some atropine preparations may contain sodium metabisulfite, which has been shown to cause anaphylaxis and less severe systemic reactions in susceptible individuals. In the United States and Canada, over 260 severe adverse allergic reactions due to sulfites, including seven deaths, have been described.8 In the past, many drugs have contained metabisulfite additives, including medications used in the treatment of anaphylaxis, such as epinephrine and albuterol.9,10 The Food and Drug Administration now requires the labeling of drugs containing metabisulfite additives, and the labeling for the atropine autoinjector used by the U.S. military does not have such a warning. In addition, the atropine used in the testing of this patient did not contain sulfite additives.
Implications of Adverse Reactions to Atropine
Although adverse reactions to atropine are rare, cases such as this will likely arise occasionally in military members. Given the pervasive threat of nonconventional weapons in today's world, the ability to receive appropriate medical therapies in the event of nerve agent attack is critical. With the growing number of civilian first responders in homeland security chemical and biological incident response teams, more individuals with such adverse reactions to atropine are likely to be identified. If these individuals are going to be retained in positions where nerve agent exposure is possible, alternatives to atropine may be needed.
It is assumed that any agent with cholinergic blocking activity has the potential to be a nerve agent antidote. In fact, agents with greater lipid solubility may provide for better CNS penetration and more effective treatment of the central effects of nerve agents. In the past, mixtures of the centrally acting incapacitating agent 3-quinuclidinyl benzilate or benactyzine with atropine were tested but were found to have undesirable CNS side effects that made their use in a military setting impractical.11
More useful alternatives are found in clinical medicine, particularly in anesthesia where glycopyrronium bromide (glycopyrrolate) and scopolamine hydrobromide have been used in lieu of atropine in clinical situations where atropine hypersensitivity exists.7,12 Clinical uses for scopolamine and glycopyrrolate include preoperative administration to diminish respiratory secretions, intraoperative prevention of adverse cholinergic reactions, and postoperative administration with the anticholinesterase neostigmine (which can be used to terminate curarization) to prevent its adverse muscarinic effects. Glycopyrrolate does not penetrate the CNS and may not be as effective at reversing CNS effects of nerve agents, but it is also less likely to have adverse CNS consequences. Scopolamine readily crosses the bloodbrain barrier. Both compounds can be administered IV or IM. Robenshtok, et al.13 reviewed the use of these agents as atropine alternatives in the setting of nerve agent or organophosphate pesticide exposure. A treatment algorithm is presented that outlines the initial use of glycopyrrolate either IV or IM, combined with benzodiazepines or scopolamine as needed based on the presence of seizures or CNS symptoms from nerve agent exposure.
Questions remain to be answered regarding the use of glycopyrrolate or scopolamine for this indication, however. Given that these agents are infrequently used, it is not clear whether they would be available in sufficient quantities and in a usable form to be beneficial after large-scale exposure to nerve agents. Current military training allows for the easy administration of atropine autoinjectors in the event of a nerve agent mass casualty. Even if these agents were available in a packaging system like the atropine autoinjector, it is possible that attempting to incorporate their use into training programs for the relatively small number of individuals likely to have allergy or hypersensitivity to atropine may not be practical.
Conclusion
In a combat environment where the threat of nerve agent exposure exists, effective antidotes with cholinergic blocking properties are needed. Atropine has been the agent of choice for this indication for decades and is safe and effective in the vast majority of military service members. However, this case underscores the need for alternatives in select individuals who have adverse reactions to atropine if they are going to be retained on active duty and be placed in combat environments. Although there are potentially effective alternatives to atropine, there is little experience with procuring and using these agents in these relatively rare cases. Additional research and the formulation of guidelines for management of service members with atropine sensitivity would assist in the management of these isolated cases.
References
1. Gallasch G, et al: [Side-effects of atropine: pharmacological, allergie, pseudoallergic or toxic reactions?]. Klin Monatsbl Augenheilkd 1982; 181: 96-9.
2. O'Connor PS, Mumma JV: Atropine toxicity. Am J Ophthalmol 1985; 99: 613-4.
3. Stokes HR: Drug reactions reported in a survey of South Carolina. Ophthalmology 1979; 86: 161-5.
4. Economacos G, Kanakis J: A case of hypersensitivily to atropine. Anesth Analg 1981; 38: 748.
5. Decraene T, Goossens A: Contact allergy to atropine and other mydriatic agents in eye drops. Contact Dermatitis 2001; 45: 309-10.
6. Yoshikawa K, Kawahara S: Contact allergy to atropine and other mydriatic agents. Contact Dermatitis 1985; 12: 56-7.
7. Moyano P, et al: Anesthesia in 2 cases of allergy to atropine In strabismus surgery. Rev Esp Anestesiol Reanim 1997; 44: 290-1.
8. Yang WH, Purchase EC: Adverse reactions to sulfites. Can Mecl Assoc J 1985; 133: 865-7, 880.
9. Jamieson DM, et al: Metabisulfite sensitivity: case report and literature review. Ann Allergy 1985; 54: 115-21.
10. Riggs BS, Harchelroad FP Jr., Poole C: Allergic reaction to sulflling agents. Ann EmergMed 1986; 15: 77-9.
11. Sidell FR, Takafuji E, Franz D: Medical Aspects of Chemical and Biological Warfare. Washington, DC, TMM Publications, 1997.
12. Dundee JW, Mirakhur RK: Hypersensitivity Io atropine. Br J Anacsth 1978: 50: 866.
13. Robenshtok E, et al: Adverse reaction to atropine and the treatment of orgariophosphate intoxication. Isr Med Assoc J 2002: 4: 535-9.
Guarantor: LT Jenifer D. Hague, MC USN
Contributors: LT Jenifer D. Hague, MC USN*; LCDR Jeffrey J. Derr, MC USNR[dagger]
* General Medical Officer, Marine Air Control Group 28, 2nd Marine Air Wing, Cherry Point, North Carolina, 28530.
[dagger] Occupational Medicine, Marine Air Control Group 28, 2nd Marine Air Wing, Cherry Point, North Carolina, 28530.
The opinions or assertions contained herein are the private views of the authors and are not to be construed as official or as reflecting the view of the Department of the Navy.
This manuscript was received for review in May 2003 and was accepted for publication in July 2003.
Reprint & Copyright © by Association of Military Surgeons of U.S., 2004.
Copyright Association of Military Surgeons of the United States May 2004
Provided by ProQuest Information and Learning Company. All rights Reserved