Rationale: Genetic variation of the β2-adrenoceptor (ADRB2) influences receptor function m vitro. There are reports that, in vivo, bronchodilator response is related to ADRB2 genotype, and that clinical outcomes during chronic therapy with β2-agonist drugs are also influenced by genotype. Whether these features are related to single nucleotide polymorphisms or to combinations (haplotypes) is unclear. Objectives: Our aim was to measure bronchodilator response in patients with asthma stratified by ADRB2 haplotype. This was done after eliminating the confounding effect of prior drug treatment with inhaled β2-agonists and corticosteroids. Methods: ADRB2 haplotype was determined in 176 patients with asthma, of whom 161 harbored the six most common combinations. Treatment with inhaled β2-agonists and inhaled corticosteroids was withheld for appropriate intervals. Spirometric changes 20 minutes after a single dose of albuterol (2.5 mg by nebulizer) were then recorded. Results: There were no significant differences in bronchodilator response (% improvement in FEV^sub 1^) with respect to any of the major ADRB2 haplotypes or genotypes. Conclusions: Genetic variation of the ADRB2 does not influence the immediate response to inhaled β2-agonist. The confounding effect of tolerance resulting from regular β2-agonists use must be controlled when assessing the pharmacogenetic influences on clinical outcomes with β2-agonists.
Keywords: asthma therapy; β2-adrenoceptor; β2-agonist; haplotype
Single nucleotide polymorphisms (SNPs) of the β2-adrenoceptor (ADRB2) and its regulator peptide are common (1), and in vitro studies have demonstrated their functional importance (2-6). Amino-acid substitutions at positions 16 (Gly to Arg) and 27 (Gln to Glu) of the β2-receptor, as well as position 19 (Cys to Arg) of the upstream peptide appear to confer altered capacity for receptor downregulation and expression (7). Clinical studies have also provided evidence both in healthy volunteers (8-10) and in patients with asthma (11, 12) that acute in vivo responses to β-agonist (10, 11), as well as the capacity to develop receptor desensitization (9), are modified in relation to ADRB2 genotype. Further, there is a growing body of evidence that ADRB2 genotype (position 16) is a marker for adverse clinical outcomes with chronic β2-agonist exposure (13, 14).
Unfortunately, it has been difficult to establish consistent relationships between in vitro and in vivo data. The reasons for this are complex, but at least two appear important. First, there is the issue of "endogenous downregulation" (1). Paradoxically, for reasons determined by genotype, the acute response to pharmacologic concentrations of β2-agonists in vivo may be greatest in patients harboring receptors that are theoretically resistant to downregulation with exposure to physiologic concentrations of endogenous catecholamine (15). This may explain why, in vivo, acute responses are greater in Arg-16 homozygotes (11, 12), whereas the same genotype predisposes to adverse outcomes, possibly resulting from enhanced pharmacologically induced downregulation during long-term β-agonist exposure (13, 14). Second, because of linkage disequilibrium, the distribution of SNPs is not random. Rather, particular combinations of SNPs (haplotypes) occur, and these may be of more importance in determining the clinical phenotype, particularly if each SNP has a functional role and where one SNP operates in an opposite direction to the other (16). Against this background, Drysdale and colleagues have described the common haplotypes of ADRB2, comprising a relatively small number of combinations of SNPs (17).
A significant relationship between ADRB2 haplotype and the acute response to β2-agomst has been reported, but remains unclear (17). In the present study, our aim was to confirm that there are consistent between-haplotype differences in the response to single doses of inhaled albuterol in patients with asthma. Given the importance of pharmacologic tolerance in relation to our study question, we rigorously sought to minimize any confounding influence of current asthma treatment by withdrawing both inhaled corticosteroid and β2-agonist therapy before patient assessment.
Some of the data contained in this manuscript have been reported in an earlier abstract (18).
METHODS
The study was conducted in the course of assessing patients for a larger clinical trial. Primary care patients with doctor-diagnosed mild to moderate bronchial asthma treated for 6 months or longer, of whom nearly 80% were taking regular inhaled corticosteroid, were invited to participate. Current smokers and ex-smokers with a cumulative consumption of greater than 10 pack years were excluded. At the first study visit, a 10 ml venous blood sample was obtained and, after DNA extraction, ADRB2 haplotype was determined using previously described methods (19) and classified according to Drysdale and colleagues (17). The nonsynonymous polymorphisms comprising the common haplotypes were as follows: Arg-BUP19, Gly-16, Glu-27, and Thr-164 (haplotype 2); Cys-BUP19, Arg-16, Gin-27, and Thr-164 (haplotype 4); Cys-BUP19, Gly-16, Gin-27, and Thr-164 (haplotype 6); and Cys-BUP19, Gly-16, Gin-27, and Ile-164 (haplotype 7). Patients harboring the 2/2, 2/4, 2/6, 4/4, 4/6, 6/6, and X/7 haplotypes (where X was 2, 4, or 6) continued in the study, but those with rarer or indeterminate haplotypes were withdrawn. The investigators undertaking the clinical component of the study remained blinded to haplotype data.
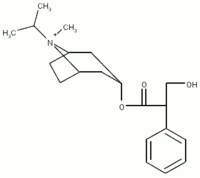
Before bronchodilator response measurement, all β2-agonist and inhaled corticosteroid treatment was withdrawn in a sequential manner. Long- and short-acting β2-agonists were withdrawn at the first study visit to allow reversal of any downregulation resulting from regular β2-agonists exposure. Each patient was provided with a substitute "reliever" inhaler containing 20 µg/puff ipratropium (Atrovent; Boehringer, Ingelheim, Germany). They also received an inhaler containing albuterol (Ventolin; GlaxoSmithKline, Greenford, UK) strictly for emergency use, a supply of 20 mg prednisone tablets, and a personalized action plan to guide the use of these drugs in the event of deteriorating asthma. After 2 weeks (or earlier, if necessary), patients attended for further assessment. Those unable to tolerate β2-agonist withdrawal were excluded from the study. Those who tolerated β2-agonist withdrawal and who were not taking inhaled corticosteroid therapy underwent the bronchodilator response test.
For those patients taking inhaled corticosteroid, this treatment was discontinued for 3 weeks before bronchodilator response was assessed. During this period, patients monitored their symptoms and peak flows twice daily, and were telephoned by an investigator every 3 days. They continued to refrain from all β2-agonist use. Predetermined individualized criteria, based on peak flow and symptoms, were set to determine "unacceptable deterioration." If this occurred before 3 weeks, then patients were instructed to contact the researchers promptly, and their bronchodilator response was measured. Where albuterol use was unavoidable for reasons of safety, patients were withdrawn if β2-agonist use had occurred on more than one single occasion. If used on one occasion only, then spirometric measurements were delayed for at least 6 hours. Patients had 24-hour access to study investigators. The protocol for β2-agonist and inhaled steroid withdrawal has been safely undertaken previously by the investigators (20).
Bronchodilator response was measured by spirometry before and 20 minutes after a single dose of inhaled albuterol (2.5 mg. given via nebulizer). Spirometers were calibrated before use. Three acceptable tests using American Thoracic Society criteria (21) were obtained; each measurement of FEV^sub 1^ and FVC was reproducible to within 100 ml.
The study protocol was approved by the Otago and Canterbury Ethics Committees, and each participant gave written, informed consent.
Statistical Analyses
No power calculation was undertaken a priori, given that the reported data were derived from a study that had another primary outcome. Bronchodilator response was calculated as the percent change in FEV^sub 1^ from baseline. It was further classified as "positive" if the percent change was 12% or greater and a minimum of 200 ml. The effects of ADRB2 haplotype and genotype were determined by analysis of covariance using baseline FEV^sub 1^ as the covariate.
RESULTS
A total of 176 patients entered the study, 15 of whom had either an indeterminate haplotype or a rare combination and were excluded. The remaining 161 patients harbored the 2/2 (n = 35, 21.7%), 2/4 (n = 51, 31.7%), 2/6 (n = 25, 15.5%), 4/4 (n = 23, 14.3%), 4/6 (n = 22, 13.7%), and 6/6 or X/7 ("other"; n = 5, 3.1%) ADRB2 combinations, respectively. The distribution of haplotypes was found to be in Hardy-Weinberg equilibrium when analyzed using Arlequin software (Department of Anthropology, University of Geneva, Geneva, Switzerland [22]), with haplotypes treated as multiple alleles at a single locus. The demographic data for the study population are shown in Table 1.
Because of the small sample size, results for the "other" group (n = 5) were not analyzed and are not reported further. Eighteen subjects failed to complete the study protocol. Of these, four withdrew because of clinical deterioration requiring treatment intervention, six withdrew because of inability to tolerate β2-agonist withdrawal, and eight withdrew due to protocol violation or withdrawal of consent. Among those who were unable to tolerate β2-agonist withdrawal, there was no predominance of any one haplotype (2/2, n = 2; 2/4, n = 2; 2/6, n = 1; and 4/4, n = 1). The negative changes in prebronchodilator FEV^sub 1^, which occurred after β2-agonist and inhaled corticosteroid withdrawal, were not significantly different between haplotype groups, ranging from 0.14 L in the 4/4 haplotype group (SD = 0.21) to 0.21 (SD = 0.27) in the 4/6 group (not significant).
The mean % change in FEV^sub 1^ after single doses of albuterol ranged from 11.6% (SD = 8.2) for 2/4 subjects to 16.0% (SD = 10.6) for 2/2 subjects. The results are shown in Figure 1. There were no significant differences between haplotype groups by analysis of covariance (p = 0.21). There was no evidence that haplotype groups 2/2 and 4/4 consistently had the lowest and highest bronchodilator responses. When bronchodilator response was defined as an improvement in FEV^sub 1^ of 12% or greater, the percentage of patients with a positive response was 52, 41, 48, 48, and 37% for 2/2, 2/4, 2/6, 4/4, and 4/6 haplotype groups, respectively (not significant).
Further analysis by position 16 genotype revealed that the mean percent change in FEV^sub 1^ for homozygous Arg-16 subjects (15.6%, SD = 15.0; n = 19) was not significantly different from the percent increase in FEV^sub 1^ among homozygous Gly-16 subjects (15.5%, SD = 12.0; n = 56; mean difference = 0.1%; 95% confidence interval = -7.0 to 7.1; p = 0.99).
DISCUSSION
The results of the present study have failed to confirm a significant and consistent relationship between ADRB2 haplotype and the magnitude of response to a single inhalation of albuterol. This was true whether that response was assessed linearly (% increase in FEV^sub 1^) or categorically (> or
We also compared patients in our study who were homozygous for the Arg-16 and Gly-16 genotypes (the genotype that has been featured most frequently in the literature [11-13, 23]). These additional analyses also failed to confirm a significant relationship between genotype and bronchodilator response. Thus, whether comparisons were made by haplotype or only for selected single polymorphisms, we are unable to confirm a clearcut relationship between genotype/haplotype and bronchodilator response.
The reasons for the apparent discrepancy between the present results and those reported previously may be related to issues of subject selection and study protocol. Drysdale and colleagues (17) studied a group of subjects with asthma for whom the inclusion criteria already included a positive bronchodilator response (see also Reference 24) Arguably, excluding subjects who failed to demonstrate bronchodilator response may have led to selection bias with respect to the primary end-point. Any definition of asthma that includes "reversible airflow obstruction" is obviously problematic in this regard, and for this reason we included patients with "doctor-diagnosed" rather than spirometrically defined asthma.
Another important issue is the effect of prior drug use on bronchodilator response. Given that the functional consequences of genetic variation of ADRB2 theoretically include differences in predisposition to receptor downregulation, current treatment with β2-agonists may be important. In previous studies (11, 12, 17), prior exposure to β2-agonist treatment was permitted. Arguably, if a particular haplotype is associated with the development of greater degrees of bronchodilator tolerance, then current treatment with β2-agonist may have a confounding effect on the measured relationship between genotype/haplotype and bronchodilation after single doses of β2-agonist. Recent data provide supportive evidence that airway function is significantly altered in relation to ADRB2 genotype, depending on whether regular β2-agonist treatment has recently been started or stopped (13). Inhaled corticosteroid treatment may also have an influence. By reducing bronchial hyperresponsiveness and improving airway opening, inhaled corticosteroid therapy may reduce the available response to bronchodilator and confound the overall results. Ideally, for these reasons, treatment-naive subjects should be studied. In practice, however, this is not feasible, but these problems provided the rationale for our treatment-withdrawal protocol.
More recent studies report inconsistent relationships between ADRB2 genotype/haplotype and bronchodilator response. In the report by Silverman and colleagues (25), a significant relationship was found for a single synonymous polymorphism (at nucleotide 523), which has hitherto been unreported. For associated haplotypes, the pattern of relationship to bronchodilator response was in fact opposite to that reported by Drysdale and colleagues (17). In contrast, although in the Genetics of Asthma in Latino Americans study (23) the impact of ADRB2 genotype/ haplotype was similar to that reported previously (11, 12) (i.e., subjects harboring the Arg-16 moiety demonstrated enhanced bronchodilator response), this was limited to certain ethnic groups (i.e., Puerto Ricans, but not Mexicans). Also this relationship was observed only in subjects whose asthma was characterized by a prebronchodilator FEV^sub 1^ of less than 80% predicted. In both studies (23, 25), no attempts were made to withdraw β2-agonist treatment before the albuterol challenge, again raising the possibility that the overall inconsistencies (in relation to ethnicity or asthma phenotype) may have been due to confounding by preexisting pharmacologie tolerance. In our own study population, comprised only of New Zealanders of European descent, ethnic background is unlikely to be a reason for our negative findings. Likewise there were no important differences in the severity of airflow obstruction between the present study population and those studied by Choudhry and colleagues (23), which might account for our negative results.
In the recently published study by Israel and colleagues (13), regular inhaled albuterol was associated with impaired lung function in patients harboring the Arg-16 genotype. Similarly, asthma exacerbation rates were increased with regular albuterol compared with "as-required" use in the same genotype group (14). The relevance of ADRB2 haplotypes, rather than SNPs, has not been assessed in these long-term studies. Clearly, the absence of a relationship between ADRB2 genotype/haplotype and acute changes in airway opening with β2-agonist reported in this and other studies (26) does not preclude the potential importance of ADRB2 pharmacogenetics in determining outcomes when β2-agonist drugs are administered regularly (27).
Conflict of Interest Statement: D.R.T. has received a research grant from GlaxoSmithKline, and has acted as an expert witness on behalf of AstraZeneca; M.I.E. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; M.A.K. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; A.D.S. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; S.I. received an educational grant of $40,000 (NZ) per annum for 2 years (2001-2003) from GlaxoSmithKline; A.L.M. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; M.D.L. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; J.O.C. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; T.H. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; M.P.S. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; K.P.B. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; G.P.H. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript.
References
1. Small KM, McGraw DW, Liggett SB. Pharmacology and physiology of human adrenergic receptor polymorphisms. Annu Rev Pharmacol Toxicol 2003;43:381-411.
2. Green SA, Cole G, Jacinto M, Innis M, Liggett SB. A polymorphism of the human beta 2-adrenergic receptor within the fourth transmembrane domain alters ligand binding and functional properties of the receptor. J Biol Chem 1993;268:23116-23121.
3. Green SA, Turki J, Innis M, Liggett SB. Amino-terminal polymorphisms of the human beta 2-adrenergic receptor impart distinct agonist-promoted regulatory properties. Biochemistry 1994;33:9414-9419.
4. Green SA, Turki J, Bejarano P, Hall IP, Liggett SB. Influence of beta 2-adrenergic receptor genotypes on signal transduction in human airway smooth muscle cells. Am J Respir Cell Mol Biol 1995;13:25-33.
5. McGraw DW, Forbes SL, Kramer LA, Liggett SB. Polymorphisms of the 5' leader cistron of the human beta2-adrenergic receptor regulate receptor expression. J Clin Invest 1998;102:1927-1932.
6. Moore PE, Laporte JD, Abraham JH, Schwartzman IN, Yandava CN, Silverman ES, Drazen JM, Wand MP, Panettieri RA Jr, Shore SA. Polymorphism of the beta(2)-adrenergic receptor gene and descnsitization in human airway smooth muscle. Am J Respir Crit Care Med 2000;162:2117-2124.
7. Liggett SB. Pharmacogenetics of beta-1- and beta-2-adrenergic receptors. Pharmacology 2000;61:167-173.
8. Hoit BD, Suresh DP, Craft L, Walsh RA, Liggett SB. beta2-adrenergic receptor polymorphisms at amino acid 16 differentially influence agonist-stimulated blood pressure and peripheral blood flow in normal individuals. Am Heart J 2000;139:537-542.
9. Dishy V, Sofowora GG, Xie HG, Kim RB, Byrne DW, Stein CM, Wood AJ. The effect of common polymorphisms of the beta2-adrenergic receptor on agonist-mediated vascular desensitization. N Engl J Med 2001;345:1030-1035.
10. Cockcroft JR, Gazis AG, Cross DJ, Wheatley A, Dewar J, Hall IP, Noon JP. Beta(2)-adrenoceptor polymorphism determines vascular reactivity in humans. Hypertension 2000;36:371-375.
11. Lima JJ, Thomason DB, Mohamed MH, Eberle LV, Self TH, Johnson JA. Impact of genetic polymorphisms of the beta2-adrenergic receptor on albuterol bronchodilator pharmacodynamics. Clin Pharmacol Ther 1999;65:519-525.
12. Martinez FD, Graves PE, Baldini M, Solomon S, Erickson R. Association between genetic polymorphisms of the beta2-adrenoceptor and response to albuterol in children with and without a history of wheezing. J Clin Invest 1997;100:3184-3188.
13. Israel E, Chinchilli VM, Ford JG, Boushey HA, Cherniack R, Craig TJ, Deykin A, Fagan JK, Fahy JV, Fish J, et al. Use of regularly scheduled albuterol treatment in asthma: genotype-stratified, randomised, placebo-controlled cross-over trial. Lancet 2004;364:1505-1512.
14. Taylor DR, Drazen JM, Herbison GP, Yandava CN, Hancox RJ, Town GI. Asthma exacerbations during long term beta agonist use: influence of beta(2) adrenoceptor polymorphism. Thorax 2000;55:762-767.
15. Lee DK, Bates CE, Lipworth BJ. Acute systemic effects of inhaled salbutamol in asthmatic subjects expressing common homozygous beta2-adrenoceptor haplotypes at positions 16 and 27. Br J Clin Pharmacol 2004;57:100-104.
16. Judson R, Stephens JC, Windcmuth A. The predictive power of haplotypes in clinical response. Pharmacogenomics 2000;1:15-26.
17. Drysdale CM, McGraw DW, Stack CB, Stephens JC, Judson RS, Nandabalan K, Arnold K, Ruano G, Liggett SB. Complex promoter and coding region beta 2-adrenergic receptor haplotypes alter receptor expression and predict in vivo responsiveness. Proc Natl Acad Sci USA 2000;97:10483-10488.
18. Taylor DR, Smith AD, Cowan JO, Brassett KP, Hewitt T, Swanney M, Iles S, Epton MJ, Kennedy M. Beta2 adrenoceptor haplotypes: relationship to bronchodilator response in patients with asthma [abstract]. Respirology 2004;9:A89.
19. Littlejohn MD, Taylor DR, Miller AL, Kennedy MA. Determination of beta2-adrenergic receptor (ADRB2) haplotypes by a multiplexed polymerase chain reaction assay. Hum Mutat 2002;20:479.
20. Jones SL, Kittelson J, Cowan JO, Flannery EM, Hancox RJ, McLachlan CR, Taylor DR. The predictive value of exhaled nitric oxide measurements in assessing changes in asthma control. Am J Respir Crit Care Med 2001;164:738-743.
21. American Thoracic Society. Standardization of spirometry: 1987 update. Statement of the American Thoracic Society. Am Rev Respir Dis 1987; 136:1285-1298.
22. Schneider S, Roessli D, Excoffier L. Arlequin: a software for population genetics data analysis. Geneva: Department of Anthropology, University of Geneva; 2000.
23. Choudhry S, Ung N, Avila PC, Ziv E, Nazario S, Casal J, Torres A, Gorman JD, Salari K, Rodriguez-Santana JR, et al. Pharmacogenetic differences in response to albuterol between Puerto Ricans and Mexicans with asthma. Am J Respir Crit Care Med 2005;171:563-570.
24. Yan L, Galinsky RE, Bernstein JA, Liggett SB, Weinshilboum RM. Histamine N-methyltransferase pharmacogenetics: association of a common functional polymorphism with asthma. Pharmacogenetics 2000; 10:261-266.
25. Silverman EK, Kwiatkowski DJ, Sylvia JS, Lazarus R, Drazen JM, Lange C, Laird NM, Weiss ST. Family-based association analysis of beta2-adrenergic receptor polymorphisms in the childhood asthma management program. J Allergy Clin Immunol 2003;112:870-876.
26. Joos L, Weir TD, Connett JE, Anthonisen NR, Woods R, Pare PD, Sandford AJ. Polymorphisms in the beta2 adrenergic receptor and bronchodilator response, bronchial hyperresponsiveness, and rate of decline in lung function in smokers. Thorax 2003;58:703-707.
27. Tattersfield AE, Hall IP. Are beta2-adrenoceptor polymorphisms important in asthma: an unravelling story. Lancet 2004;364:1464-1466.
D. Robin Taylor, Michael J. Epton, Martin A. Kennedy, Andrew D. Smith, Steven Iles, Allison L. Miller, Matthew D. Littlejohn, Jan O. Cowan, Tracey Hewitt, Maureen P. Swanney, Karen P. Brassett, and G. Peter Herbison
Otago Respiratory Research Unit and Department of Preventive and Social Medicine, Dunedin School of Medicine; and Canterbury Respiratory Research Unit and Department of Pathology, Gene Structure and Function Laboratory, Christchurch School of Medicine, University of Otago, Dunedin, New Zealand
(Received in original form January 20, 2005; accepted in final form May 9, 2005)
Supported by a grant from the Health Research Council of New Zealand. A.D.S. and S.I. were GlaxoSmithKline Research Fellows, and received an unrestricted educational grant from GlaxoSmithKline during the conduct of the study.
Correspondence and requests for reprints should be addressed to Professor D. Robin Taylor, M.D., F.R.C.P.(C)., Dunedin School of Medicine, P.O. Box 913, Dunedin, New Zealand. E-mail: robin.taylor@stonebow.otago.ac.nz
Am J Respir Crit Care Med Vol 172. pp 700-703, 2005
Originally Published in Press as DOI: 10.1164/rccm.200501-092OC on June 23, 2005
Internet address: www.atsjournals.org
Copyright American Thoracic Society Sep 15, 2005
Provided by ProQuest Information and Learning Company. All rights Reserved