PURPOSE: Idiopathic pulmonary fibrosis (IPF) is a relentless, progressive and fatal disease with no known effective treatment. Increased acid gastro-esophageal reflux (GER) has been associated with IPF. We speculate that acid gastroesophageal reflux (GER) is an important factor for the development and/or progression of IPF.
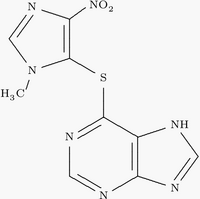
METHODS: Patients with new onset IPF and presenting with symptoms and documented gastro-esophageal reflux disease (GERD) or abnormal acid GER by 24-hour esophageal pH probe testing, who refused conventional therapy (prednisone and azathioprine) or other concurrent medical treatments implicated for IPF and chose to be treated solely with anti-acid GER therapy.
RESULTS: Adequate suppression of acid GER was ascertained by 24-hour esophageal pH monitoring. Patients were followed regularly with pulmonary function tests (PFT) over 2-6 years. The PFTs (Forced vital capacity [FVC] and diffusion capacity for carbon monoxide [DLCO]) in all 4 patients stabilised or improved while being maintained on adequate daily treatment for acid GER, and were alive at last follow-up. None of the patients manifested acute exacerbation of IPF nor needed additional treatment for respiratory problems or antibiotics during this period. After maintaining 4 years of improved status in PFTs and exercise testing while adhering to treatment for acid GER, one patient's deterioration correlated with poor compliance to daily treatment during the 5th year, although the PFTs at last follow-up 6 years since diagnosis showed stabilisation compared to baseline. Another patient stabilised upon adhering to anti-acid GER treatment after an initial period of deterioration that was associated with non-adherence.
CONCLUSION: This case series suggests that add GER might be an important risk factor for IPF progression and that adequate treatment for abnormal acid GER may in part improve the outcome of patients with IPF. We also hypothesize that pulmonary fibrosis occurs in individuals who are genetically susceptible to develop fibrosis from recurrent chronic add GER.
CLINICAL IMPLICATIONS: Future clinical studies are indicated to determine the efficacy of treatment for acid GER in IPF either in combination with other agents or as a sole agent.
DISCLOSURE: Steve Yang, None
Ganesh Raghu MD Steve T. Yang MBBS * Carolyn Spada RN Jennifer Hayes RN Carlos Pelligrini MD Singapore General Hospital, Singapore, Singapore
COPYRIGHT 2005 American College of Chest Physicians
COPYRIGHT 2005 Gale Group