Background & objectives: Metallo betalactamase (MBL)-mediated resistance to carbapenems is an emerging threat in hospital isolates of Pseudomonas aeruginosa. Though there are several screening methods to detect this enzyme production, the National Committee for Clinical Laboratory Standards (NCCLS) does not have performance standards documented so far. There is not enough information from the Indian subcontinent regarding the prevalence and the screening methods for these enzymes. The present study was undertaken to detect MBL in nosocomial isolates of P. aeruginosa by two screening methods.
Methods: Fifty consecutive P. aeruginosa isolates obtained from hospitalized patients were subjected to susceptibility testing to antipseudomonal drugs by disc diffusion, and minimum inhibitory concentration (MIC) of imipenem was determined. The production of MBL was detected by 4-fold reduction in MIC with imipenem-ethylene diamine tetraacetic acid (EDTA) and the zone size enhancement with EDTA impregnated imipenem and ceftazidime discs.
Results: Sixteen per cent of the isolates tested were resistant to imipenem by disc diffusion method of which 87.5 per cent exhibited a zone size enhancement with EDTA impregnated imipenem and ceftazidime discs as well as a 4-fold reduction in MIC with imipenem EDTA. The imipenem susceptible isolates (84%) had normal MIC values and exhibited no zone diameter enhancement with EDTA impregnated antibiotic discs.
Interpretation & conclusion: MBL-mediated imipenem resistance in P. aeruginosa is a cause for concern in the therapy of critically ill patients. The two confirmatory methods i.e., zone diameter enhancement with EDTA impregnated imipenem and ceftazidime discs and 4-fold reduction in MIC with imipenem EDTA combination are equally effective for their detection.
Key words Carpapeiiems - imipenem - metallo betalactamase - Pseudomonas aeruginosa
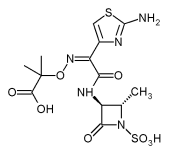
The introduction of carbapenems into clinical practice represented a great advance for the treatment of serious bacterial infections caused by β-lactamresistant bacteria1. However, carbapenem resistance has been observed frequently in nonfermenting bacilli such as Pseudomonas aeruginosa andAcinetobacter spp. The common form of resistance is mediated by lack of drug penetration (i.e., porin mutations and efflux pumps) and/or carbapenem-hydrolyzing β-lactamases. Based on molecular studies, carbapenemhydrolyzing enzymes are classified into four groups A, B, C and D. The métallo betalactamases (MBLs) belong to group B and are enzymes requiring divalent cations as cofactors for enzyme activity, being inhibited by the action of a metal ion chelator2. The MBLs efficiently hydrolyze all β-lactams, except aztreonam in vitro3.
P. aeruginosa is a common Gram-negative bacillus associated with hospital infections and is often difficult to eradicate due to its resistant drug profile. Therefore, detection of MBL-producing Gram-negative bacilli especially P. aeruginosa is crucial for the optimal treatment of patients particularly in critically ill and hospitalized patients, and to control the spread of resistance4. There is not much information available on MBL producing/^ aeruginosa isolates from India. We therefore undertook this study to detect the MBL in P. aeruginosa isolates obtained from hospitalized critically ill patients. Two different screening methods were used to find out their effectiveness in the detection of these isolates.
Material & Methods
Fifty consecutive non-repetitive isolates of P. aeruginosa from various specimens like urine (10), blood (2), respiratory specimen-BAL-broncho alveolar lavage (18) and exudates (20) were collected over a period of 1 month (June-July 2003). All the isolates were from critically ill patients from the intensive care unit of a tertiary care centre in south India.
The susceptibility to antipseudomonal drugs was done on Mueller Hinton agar by disc diffusion method in accordance with National Committee for Clinical Laboratory Standards (NCCLS) standards incorporating standard strain of P. aeruginosa (ATCC 2V853)5. The antibiotics tested were gentamycin, amikacin, piperacillin, ciprofloxacin, ceftazidime, piperacillin-tazobactam, aztreonam (Hi-media Laboratories, Mumbai) and imipenem (BD Diagnostics, USA) LDTA, extra pure (Hi-media Laboratories, Mumbai) powder was used for screening MBL production.
MIC of imipenem for these isolates was done by agar dilution method in accordance with NCCLS standards6. The pure form of the drug was obtained from Ranbaxy Laboratories, Mumbai.
Various methods have been recommended for screening MBL. These include the modified Hodge test7, double disc synergy test using imipenem and EDTA discs or ceftazidime and EDTA discs8. EDTA impregnated imipenem discs9, and the MIC reduction of minimum four-fold with imipenem EDTA combination10. We used zone enhancement with EDTA impregnated imipenem and ceftazidime discs9, and minimum of four-fold reduction in MIC of the isolates with imipenem-EDTA combination10 in this study.
(i) Zone enhancement with EDTA impregnated imipenem and ceftazidime discs: Test organisms were inoculated on to plates with Mueller Hinton agar as recommended by the NCCLS5. A 0.5 M EDTA solution was prepared by dissolving 186.1 g of disodium EDTA .2H^sub 2^O in 1000 ml of distilled water and adjusting it to pH 8.0 by usingNaOH. The mixture was sterilized by autoclaving. Two 10 μg imipenem discs and two 30 µg ceftazidime discs were placed on the surface of an agar plate and EDTA solution was added to one of them to obtain a desired concentration of 750 µg. The inhibition zones of imipenem, ceftazidime and imipenem EDTA and ceftazidime EDTA discs were compared after 16-18 h of incubation in air at 35°C.
The EDTA impregnated antibiotic discs were dried immediately in an incubator and stored at -4°C and -20°C in airtight vials without desiccant.
(ii) MIC of imipenem EDTA combination: A previous study10 reports the use of simple microdilution method for the determination of the MIC with a combination of imipenem and EDTA. However, we adopted the agar dilution method to determine the same.
EDTA (1 ml) solution was added to 1 ml of the imipenem solution spanning similar concentrations as done for MIC to imipenem alone. Each 2 ml of EDTA and imipenem in graded concentrations was added to 18 ml of molten Mueller Hinton agar and poured on plates that were allowed to set. A fixed inoculum of the test strains was spot inoculated on these plates before incubation. The reading was taken after 18-24 h of incubation. The highest dilution inhibition the growth of the organisms was taken as the MIC.
Results & Discussion
Of the 50 isolates of P. aeruginosa, 8 (16%) showed resistance to imipenem by the disc diffusion method. These isolates also had high MIC values to imipenem ranging from 8-128 μ§/ιη1. Seven of these 8 isolates exhibited a significant zone size enhancement with the EDTA impregnated discs when compared with the plain antibiotic discs. Four isolates had zone size enhancement with both ceftazidime EDTA (caEDTA) and imipenem EDTA (imEDTA) discs. The zone size enhancement was 5-28 mm for caEDTA and 7-27 mm for imEDTA. Two isolates exhibited a zone size increase only with caEDTA disc and one only with imEDTA disc. A 8-128 fold reduction of MIC with imipenem EDTA combination was observed in all the 7 isolates which had a significant zone diameter increase with the EDTA impregnated antibiotic discs. The ATCC 27853 P. aeruginosa neither exhibited a zone size enhancement nor a fall in MIC.
The remaining 42 isolates were susceptible to imipenem with their MIC levels within the acceptable range and showed a zone size increase of only 0-5 mm with the EDTA impregnated antibiotic discs. Twenty three (46%) of the 50 isolates were resistant to the third generation cephalosporins tested.
All the 8 isolates which exhibited high imipenem MIC values were also resistant to fluoroquinolones and aminoglycosides.
There are reports on MBL production in P. aeruginosa from various countries like Brazil", Korea12, Singapore13, and France14. Metallobetalactamase was first reported as a zinc dependent enzyme in Bacillus cereus in mid 1960s15. A few decades later, imipenem-hydrolyzing métallo enzymes were found in Aeromonas hydrophila^ and Bacleroides fragilis{1. All these enzymes-were produced by chromosomal genes and at first were recovered only from single clinical isolates. In 1991, Japan reported the first plasmid-mediated métallo betalactamase in P. aeruginosa18. This was soon followed by another report of transferable metalloenzyme in B. fragilis}9. Apart from P. aeruginosa, other bacteria like Serratia, Klebsiella pneumoniae, Escherichia coli, Enterobacter aerogenes, E. cloacae, Citrobacter freudii, Proteus vulgaris, P. putida, Acinetobacter and Alcaligenes xylosoxidans were also shown to produce MBL20.
There are frequent reports of MBL production in P. aeruginosa from the Asian and the Pacific countries, namely Hong Kong21, Taiwan21 and Japan21. In this study, we observed 16 per cent resistance to carbapenem among the P. aeruginosa screened and 87.5 per cent of this was MBL mediated as per the screening results. Another study from south India reported 12 per cent MBL-mediated imipenem resistance in P. aeruginosa22.
Though there are several screening methods recommended for the detection of MBL production, no single test when used alone is specific for these enzymes. The modified Hodge test which is used to screen the carbapenemase production in Gramnegative bacilli can also produce false negative results8. The use of EDTA impregnated imipenem and ceftazidime discs resulted in a significant increase in the zone size for the MBL producers when compared to the non producers in this study. Similar observations have been made with use of EDTA by other workers9. However, we found that the ceftazidime EDTA disc could pick up additional isolates of MBL producer as compared to the imipenem EDTA disc.
A MIC reduction of 8-128 fold with imipenem EDTA combination was observed in our study as compared to a 4-512-fold reduction reported by Migliavaccaeia/10. One isolate which showed a high MIC to imipenem did not exhibit zone size potentiation with the EDTA impregnated antibiotics discs suggesting other mechanisms of resistance such as permeability of the outer membrane and/or active efflux probably associated with overproduction of endogenous class C betalactamase.
MBL production is a significant problem in hospital isolates of P. aeruginosa. With increasing isolation of ESBL producing isolates in the hospital setting necessitating the use of carbapenems, the problem of MBL production is also increasing. The development of simple screening tests, designed to detect acquired MBL production will be a crucial step towards large scale monitoring of these emerging resistant determinants. The two methods used for screening of MBL production namely, the use of EDTA impregnated antibiotic discs and the MIC to imipenem EDTA combination both proved equally effective for the detection of MBL-producing isolates.
References
1. Kahan FM, Kropp H, Sundelof JG, Birnbaum J, Thienamycin: development of imipenen-cilastatin. JAntimicrob Agents Chemother 1983; 12 (Suppl D): SI-35.
2. Ambler RP. The structure of beta-lactamases. Philos Trans R Soc London Bio Sd 1980; 289 : 321-31.
3. Bush K, Jacoby GA, Medeiros AA. A functional classification scheme for β-lactamascs and its correlation with molecular structure. Antimicrob Agents Chemother 1995; 39: 1211-33.
4. Richet HM, Mohammed J, McDonald LC, Jarvis WR. Building communication networks: international network for the study and prevention of emerging antimicrobial resistance. Emerg Infect Dis 2001; 7 : 319-22.
5. National Committee for Clinical Laboratory Standards. Performance standards for antimicrobial susceptibility testing; llth informational supplement. MlOO-SIl. National Committee for Clinical Laboratory Standards, Wayne, Pa; 2001.
6. National Committee for Clinical Laboratory Standards. Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically. NCCLS approved standard M-7-A5. National Committee for Clinical Laboratory Standards, Wayne, Pa; 2000.
7. Lee K, Chong Y, Shin HB, Kirn YA, Yong D, Yum JH. Modified Hodge and EDTA-disk synergy tests to screen metallo-p-lactamase-producing strains of Pseudomonas and Acinetobacter species. Clin Microbiol Infect 2001; 7 : 88-91.
8. Lee K. Lim YS, Yong D, Yum JH, Chong Y. Evaluation of the Hodge test and the imipenem-EDTA double-disk synergy test for differentiating metallo-p-lactamaseproducing isolates of Pseudomonas spp. and Acinetobacter spp.JClin Microbiol 2003; 41 : 4623-9.
9. Yong D, Lee K., Yum JH, Shin HB, Rossolini GM, Chong Y. Imipenem-EDTA disk method for differentiation of metallo-p-lactamase-producing clinical isolates of Pseudomonas spp. and Acinetobacter spp. J CUn Microbiol 2002; 40: 3798-801.
10. Migliavacca R, Docquier JD, Mugnaioli C, Amicosante G, Daturi R, Lee K, et al. Simple micro dilution test for detection of metallo-p-lactamase production in Pseudomonas aeruginosa. J Clin Microbiol 2002; 40 : 4388-90.
11. Gales AC, Menezes LC, Silbert S, Sader HS. Dissemination in distinct Brazilian regions of an epidemic carbapenemresistant Pseudomonas aeruginosa producing SPM metalloβ-lactamase. JAntimicrob Chemother 2003; 52 : 699-702.
12. Lee K, Lim JB, Yum JH, Yong D, Chong Y, Kim JM, et al. è/ov|m2 cassette-containing novel intégrons in metallo-βlactamse-producing Pseudomonas aeruginosa and Pseudomonas putida isolates disseminated in a Korean hospital. Antimicrob Agents Chemother 2002; 46 : 1053-8.
13. Koh TH, Wang GC, Sng LH. IMP-1 and a novel metallo-βlactamse, VIM-6, in flurorescent pseudomonads isolated in Singapore. Antimicrob Agents Chemother 2004; 48 : 2334-6.
14. Poirel L, Naas T, Nicolas D, Collet L, Bellais S, Cavallo ID, et al. Characterization of VIM-2, a carbapenemhydrolyzing metallo-p-lactamase and its plasmid- and integron-borne gene from a Pseudomonas aeruginosa clinical isolate in France. Antimicrob Agents Chemother 2000; 44: 891-7.
15. Sabath LD, Abraham EP. Zinc as a cofactor for cephalosporinase from Bacillus cereus 569. Biochem J 1966; 98: I1C-3.
16. Shannon K, King A, Phillips I. Beta-lactamases with high activity against imipenem and Sch 34343 from Aeromonas hydrophila. J Antimicrob Chemother 1986; 17 : 45-50.
17. Cuchural GJ Jr, Malamy MH, Tally FP. Beta-lactamasemediated imipenem resistance in Bacteroids fragilis. Antimicrob Agents Chemother 1986; 30 : 645-8.
18. Watanabe M, lyobe S, Inoue M, Mitsuhashi S. Transferable imipenem resistance in Pseudomonas aeruginosa. Antimicrob Agents Chemother 1991; 35 : 147-51.
19. Bandoh K, Watanabe K, Muto Y, Tanaka Y, Kato N, Ueno K. Conjugal transfer of imipenem resistance in Bacteriodes fragilis. J Antibiot (Tokyo) 1992; 45 : 542-7.
20. Arakawa Y, Shibata N, Shibayama K, Kurokawa H, Yagi T, Fujiwara H, et al. Convenient test for screening metalloβ-lactamase-producing Gram-negative bacteria by using thiol compounds. J Clin Microbiol 2000; 38 : 40-3.
21. Bell JM, Turnidge JD. Carbapenem resistance among hospitalized patients in the Asia-Pacific region (APACO): Report from the SENTRY Antimicrobial Surveillance program, 1998-2001. Abstract P715 in the 13th European Congress of Clinical Microbiology and Infectious Diseases; 2003.
22. Navaneeth BV, Sridaran D, Sahav D, Belwadi MRS. A preliminary study on métallo β-lactamase producing Pseudomonas aeruginosa hospitalized patients. Indian J Med Res 2002; 116 : 264-7.
Hemalatha V, Uma Sekar & Vijaylakshmi Kama*
Departments of Microbiology & * Critical Care Medicine, Sri Ramachandra Medical College & Research Institute, Chennai, India
Received September 15, 2004
Reprint requests: Dr Uma Sekar, Professor, Department of Microbiology, Sri Ramachandra Medical College & Research Institute (Deemed University), Porur, Chennai 600116, India
e-mail: umasekar02@yahoo.co.in
Copyright Indian Council of Medical Research Aug 2005
Provided by ProQuest Information and Learning Company. All rights Reserved