Study objectives: The central role of apoptosis in the regulation of lung inflammation is increasingly recognized. The aim of this study was to determine the parameters of cell activation and apoptosis on neutrophils from the circulation and the pulmonary compartment in patients with community-acquired pneumonia (CAP), and to assess the role of the Fas system and of complement-regulating molecules in this context.
Design and methods: The study population consisted of nine patients with CAP (group 1) and six age-matched control patients without evidence of bronchopulmonary inflammation (group 2). Apoptosis rate and expression of CD11b, CD16, CD55, CD59, CD95, and CD114 surface molecules on systemic and bronchoalveolar neutrophils were assessed ex vivo using fluorescence-activated cell sorter analysis.
Results: In patients with CAP, we found a significant decrease of the mean apoptosis rate in pulmonary neutrophils compared to systemic neutrophils, without concomitant changes in Fas expression. In contrast, cell activation markers were significantly increased on pulmonary cells (CD11b, 288 [+ or -] 98.2 relative mean fluorescence intensity [rMFI] vs 53.8 [+ or -] 10.8 rMFI on peripheral cells), and similar changes were observed with respect to the expression of complement-regulating molecules. Pulmonary polymorphonuclear neutrophils of the control group showed analogous changes, compared to systemic neutrophils, but a significantly higher rate of apoptosis and a lower increase of activation-marker expression were found, compared to pulmonary neutrophils of patients with pneumonia.
Conclusions: Pulmonary neutrophils from patients with CAP show a decreased rate of apoptosis and increased activation status in the alveolar compartment, which may be important for effective control of pulmonary inflammation.
(CHEST 2000; 117:1679-1684)
Key words: apoptosis; complement; lung inflammation; neutrophil transmigration; pneumonia
Abbreviations: CAP = community-acquired pneumonia; G-CSF = granulocyte colony-stimulating factor; GM-CSF = granulocyte-macrophage colony-stimulating factor; IL = interleukin; ML = minilavage; PMN = polymorphonuclear neutrophils; rMFI = relative mean fluorescence intensity
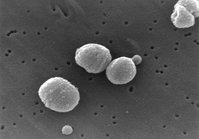
Bacterial infection of the lower respiratory tract initiates an acute inflammatory response characterized by rapid influx of polymorphonuclear neutrophils (PMN) into the affected lung parenchyma.[1] In humans, little is known about the function and survival of PMN in acutely inflamed tissues. According to experimental data, the process of leukocyte transmigration is associated with increased cellular activation and a significant delay of spontaneous apoptosis.[2]
The regulation of neutrophil survival is critical to the propagation and resolution of inflammation, and has been implicated in the pathogenesis of prolonged or inappropriate inflammation in severe infection and autoimmune disorders.[3] In chronic inflammatory diseases, such as bronchial asthma, chronic bronchitis, and rheumatoid arthritis, persistent accumulation and activation of PMN are associated with tissue injury leading to organ dysfunction and failure.[4] Patients with systemic inflammatory response syndrome show a dysregulated expression of programmed cell death in systemic neutrophils.[5]
At the site of inflammation, neutrophil apoptosis is influenced by a variety of mediators and mechanisms, including microbial products such as lipopolysaccharide, complement, cytokines, and hematopoetic growth factors. An important role of the Fas receptor/Fas ligand pathway of apoptosis induction has been demonstrated in a variety of inflammatory disorders.[6] In human PMN, this mechanism may play a critical role in the regulation of apoptosis, since neutrophils are highly susceptible to Fastriggered apoptosis in vitro and show a coexpression of Fas receptor and Fas ligand, which facilitates the autocrine induction of programmed cell death.[7] For efficient resolution of inflammation, a fine balance between the need for clearance of the inflammatory stimulus and the risk of damage to the host tissue is important. Human PMN are protected from complement damage in the inflammatory microenvironment by several membrane inhibitors, including membrane-attack-complex inhibitory factor (CD59) and decay-accelerating factor (CD55). Increased surface expression of complement regulatory molecules on PMN is a protective mechanism improving cell survival and function in the inflammatory milieu.[8] To elucidate the role of neutrophil activation, apoptosis, and complement regulation in pulmonary infection, we comparatively evaluated circulating neutrophils and cells obtained by BAL in patients with community-acquired pneumonia (CAP) and age-matched control patients without evidence of bronchopulmonary inflammation.
MATERIALS AND METHODS
Study Design
The study population consisted of two groups. Group 1 was composed of nine patients (seven men and two women; eight smokers and one nonsmoker; median age, 66 years) with CAP and serious predisposing diseases, such as COPD, bronchial asthma, coronary artery disease, diabetes mellitus, chronic renal failure, and asbestosis. Median WBC count was 11,700 cells/[micro]L. For the diagnosis of pneumonia, a new or progressive inifiltrate on the chest radiograph suggestive of pneumonia had to be present, together with two or more of the following criteria: pulmonary symptoms (such as productive cough, chest pain, or auscultatory findings); fever or hypothermia; purulent tracheal secretions ([is greater than] 70% neutrophils in bronchial minilavage [ML]); positive blood or ML culture; or [is less than] 7% intracellular bacteria in Gram's stains of ML samples. Bronchial ML samples in this group yielded Streptococcus pneumoniae in seven cases, Haemophilus influenzae in one case, and remained sterile in one patient with antibiotic pretreatment. Group 2 was composed of six patients (five men and one woman; five smokers and one nonsmoker; median age, 61 years) with peripheral nodules evaluated by fiberoptic bronchoscopy for diagnostic reasons without evidence for bronchopulmonary inflammation. Median WBC count was 4,200 cells/[micro]L; median neutrophil percentage in the bronchial ML was 4%.
This study was approved by the ethical committee of the Medical University of Lubeck.
Bronchoscopy
In both groups, bronchoalveolar PMN recovered from bronchial ML were compared to autologous peripheral PMN. Bronchoscopy was performed at admission according to standard conditions after local anesthesia.[9] Bronchoscopically guided ML was performed in the most severely affected area, otherwise in the right middle lobe with instillation of 5 to 10 mL of 0.9% NaCl. The ML fluid was immediately reaspirated; recovery was 60 to 120%. The lavage fluid was diluted to a final volume of 50 mL and vortexed until homogenous in appearance. To eliminate remaining mucus, the sample was filtrated through four layers of gauze. After centrifugation at 400g for 10 min, the cell pellet was resuspended in 2 mL of phosphate-buffered saline solution. Total cell count was performed on a hemocytometer (Coulter Electronics LTD; Luton, UK). Cells were differentiated counting a minimum of 600 cells of a cytocentrifuge smear (Cytospin II; Shandon; Frankfurt, Germany) stained with May-Grunwald/ Giemsa solution. Viability was determined by trypan blue dye exclusion, and the sample was diluted to a concentration of [10.sup.6] viable cells/mL.
Blood
Ten milliliters of venous blood was collected in ethylene diamine tetraacetic acid tubes. For lysis of erythrocytes, 300 [micro]L of blood was immediately diluted 1:15 in lysis solution (Becton Dickinson; Heidelberg, Germany). Cells were lysed for 10 min at room temperature and centrifuged for 4 min at 300g. The pellet was resuspended in phosphate-buffered saline solution supplemented with 4% fetal calf serum at 4 [degrees] C and centrifuged at 300g.
Flow Cytometry
Surface markers and apoptosis rate was determined by using three-color flow cytometry as described previously.[10] Briefly, flowcytometric analysis was done on a fluorescence-activated cell sorter scan analyzer (Becton Dickinson), and data acquisition and analysis were performed with CellQuest software (Becton Dickinson). Each measurement contained [is greater than or equal to] 10,000 cells in the granulocyte population, as determined by forward/orthogonal light scattering, positive CD66b expression, and missing human leukocyte antigen-DR expression. Detection kits and antibodies against the following epitopes were used: fluorescein isothiocyanate-labeled: deoxynucleotidyl transferase-mediated dUTP-biotin nick-end labeling (ApopTag direct in situ apoptosis detection kit; Appligene Oncor; Heidelberg, Germany), CD66b; phycoerythrin-labeled: isotype control, CD11b (complement receptor 3), CD16 (Fc[Gamma]III receptor), complement regulatory proteins CD55 (decay-accelerating factor) and CD59 (membrane-attack-complex inhibitory factor), CD95 (Fas receptor), CD114 (granulocyte colony-stimulating factor [G-CSF] receptor), the latter all purchased from Pharmingen (Hamburg, Germany); and phycoerythrin-cyanine-5-labeled: isotype control (Coulter; Hamburg, Germany). Two distinct populations were detected after deoxynucleotidyl transferase-mediated dUTP (TUNEL) nick-end labeling staining, the one with the higher fluorescence intensity representing apoptotic cells. Because no bimodal distribution was found in the expression of surface markers, this was calculated as relative mean fluorescence intensity (rMFI; monoclonal antibody/corresponding isotype control).
Statistics
Nonparametric statistics were used throughout the study. Data are given as mean [+ or -] SD unless otherwise indicated. The Wilcoxon signed rank test was used for comparison of paired samples (pulmonary vs systemic PMN from the same patients), and the Mann-Whitney U test was used for comparison of cell counts from CAP patients and control patients. A p value [is less than] 0.05 was considered significant.
RESULTS
Activation Status of Systemic and Pulmonary Neutrophils in CAP
As shown in Figure 1, we found a significant decrease of spontaneous apoptosis in pulmonary PMN compared to systemic PMN (0.3 [+ or -] 0.14% vs 1.3 [+ or -] 0.39%, respectively; p [is less than] 0.01) in pneumonia patients, which was accompanied by concomitant changes in the expression of CD16 and CD114 surface molecules (248 [+ or -] 122 rMFI [pulmonary] vs 463 [+ or -] 102.8 rMFI [systemic], and 52 [+ or -] 15.4 rMFI [pulmonary] vs 122 [+ or -] 33.6 rMFI [systemic], respectively; p [is less than] 0.01; Table 1). However, the Fas (CD95) expression on pulmonary and systemic cells was not different (11 [+ or -] 5.4 rMFI vs 12.1 [+ or -] 3.97 rMFI, respectively; p = not significant). In contrast, the expression of the activation marker CD11b (288 [+ or -] 98.2 rMFI [pulmonary] vs 53.8 [+ or -] 10.8 rMFI [systemic]; p [is less than] 0.01) and of the complement regulatory protein CD59 (68.4 [+ or -] 12.2 rMFI [pulmonary] vs 38.5 [+ or -] 11.8 rMFI [systemic]; p [is less than] 0.01) was significantly enhanced on pulmonary PMN.
[Figure 1 ILLUSTRATION OMITTED]
Table 1--Flow Cytometry Expression of Apoptosis and Binding Intensities of Monoclonal Antibodies to Surface Molecules on Peripheral and Pulmonary PMN(*)
(*) Data are presented as mean [+ or -] SD.
ND = not determined.
Differences in PMN Apoptosis and Surface Markers Between CAP Patients and Control Patients
As compared to CAP patients, the control population of patients without evidence of bronchopulmonary inflammation showed a significant enhancement of systemic PMN apoptosis (1.3 [+ or -] 0.39% vs 3.53 [+ or -] 0.94%, respectively; p [is less than] 0.01) and pulmonary PMN apoptosis (0.3 [+ or -] 0.14% vs 1.62 [+ or -] 0.44%, respectively, p [is less than] 0.01). There was no difference in the expression of CD95 on systemic and pulmonary cells (Table 1). In addition, we observed no difference in the expression of CD11b, CD59, and CD114 on systemic cells. However, the expression of CD11b and CD59 on pulmonary PMN was significantly increased in CAP patients compared to control patients (288 [+ or -] 98.2 rMFI [CD11b] vs 111 [+ or -] 23.2 rMFI [CD59], and 68.4 [+ or -] 12.2 rMFI [CD11b] vs 37.8 [+ or -] 5.4 rMFI [CD59], respectively; p < 0.01), whereas the expression of CD114 was significantly decreased in CAP patients compared to control patients (52 [+ or -] 15.4 rMFI vs 117 [+ or -] 41.4 rMFI, respectively; p [is less than] 0.01).
DISCUSSION
In this study, we determined the rate of apoptosis and expression of activation markers and complement regulatory molecules on pulmonary and systemic neutrophils from patients with CAP ex vivo.
Our major finding was a significantly increased expression of CD11b and CD59 and a decreased rate of apoptosis in pulmonary PMN compared to systemic PMN in this patient population. In addition, the apoptosis rate of pulmonary PMN was significantly decreased and CD11b expression was significantly increased in CAP patients, compared to control patients. Similar results were obtained by Watson et al[2,11] under experimental conditions. PMN transmigrated across an endothelial monolayer in vitro, and neutrophils recovered from BAL in a rat model of acute lung injury showed a decreased rate of apoptosis in association with an increased expression of CD11b.
Possible mechanisms for the prolonged neutrophil life span in inflamed tissues include the following:
(1) Cross-linking of CD11b, which results in the mobilization of intracellular calcium and consecutive inhibition of apoptosis.[12] The increased expression of CD11b on pulmonary PMN from pneumonia patients shown in this study confirms previous experimental data,[13] and reflects its essential role in PMN activation and transmigration to the inflammatory focus. The clinical relevance of PMN adhesion via CD11b/CD18 is highlighted by patients with leukocyte adhesion deficiencies. Patients with these rare inherited defects in the CD11b molecule expression are at risk for severe infections.[14]
(2) Elevated local concentrations of inflammatory mediators, such as lipopolysaccharide, interferon-[Gamma] interleukin (IL)-1, IL-6, IL-8, granulocyte-macrophage colony-stimulating factor (GM-CSF), and G-CSF, which have a marked inhibitory effect on polymorphonuclear neutrophil apoptosis in vitro.[7,15,16] Many of these mediators contribute to the activation and recruitment of circulating PMN to inflamed tissues and are released spontaneously from alveolar macrophages recovered by BAL in patients with pneumonia.[17] In particular, the presence of G-CSF and GM-CSF in BAL fluid from patients with ARDS has been shown to exert antiapoptotic activity on PMN ex vivo.[18] Similar inhibitory effects on PMN apoptosis in vitro were demonstrated using cerebrospinal fluid and BAL fluid from patients with severe head and thoracic injuries.[19] Although we did not measure G-CSF levels in BAL directly, we observed a decreased expression of the G-CSF receptor CD114 on pulmonary PMN compared to systemic PMN in patients with CAP, which indicates elevated G-CSF levels at the site of inflammation because of the well-known receptor complex internalization after binding.[20] Moreover, complement regulatory molecules that showed increased expression on PMN in the pulmonary compartment could serve an important role in the regulation of neutrophil-programmed cell death. At inflammatory sites with a rapid complement turnover, protection against complement attack may be crucial for cell survival.
(3) Since the Fas receptor/Fas ligand system is supposed to play an important role in the induction of apoptosis in human PMN, a downregulation of CD95 represents a further mechanism of decreased apoptosis. However, we observed an unchanged expression of CD95 on pulmonary PMN compared to systemic PMN in pneumonia patients. This finding is in keeping with a study showing no differences in the Fas expression of PMN after transmigration in vitro,[11] and with the observation that the incubation of PMN with G-CSF, and to a lesser extent with GM-CSF, interferon-[Gamma], and tumor necrosis factor-[Alpha] in vitro, was able to suppress Fas-mediated apoptosis but had no influence on the Fas expression.[7] Thus, proinflammatory cytokines affect neutrophil apoptosis in the inflammatory milieu without alteration of Fas expression. Instead, data from an animal model of acute lung injury indicate an association of impaired apoptotic death signaling after Fas stimulation with reduced expression of IL-1[Beta]-converting enzyme family proteases, which are involved in the activation of proapoptotic enzymes.[21]
CONCLUSION
In summary, we have demonstrated that pulmonary neutrophils from patients with CAP show a decreased rate of apoptosis in association with upregulated surface molecules CD11b and CD59, as compared to the systemic compartment. Enhanced neutrophil survival, activation, and protection from complement damage increases the antimicrobial phagocyte function, and may therefore be beneficial for overcoming infectious challenges in the lung.
REFERENCES
[1] Rhodes GC, Lykke AW, Tapsall JW, et al. Abnormal alveolar epithelial repair associated with failure of resolution in experimental streptococcal pneumonia. J Pathol 1989; 159:245-253
[2] Watson RW, Rotstein OD, Nathens AB, et al. Neutrophil apoptosis is modulated by endothelial transmigration and adhesion molecule engagement. J Immunol 1997; 158:945-953
[3] Tan EM. Autoimmunity and apoptosis. J Exp Med 1994; 179:1083-1086
[4] Haslett C. Granulocyte apoptosis and inflammatory disease. Br Med Bull 1997; 53:669-683
[5] Jimenez MF, Watson RWG, Parodo J, et al. Dysregulated expression of neutrophil apoptosis in the systemic inflammatory response syndrome. Arch Surg 1997; 132:1263-1269
[6] Depraetere V, Golstein P. Fas and other signaling pathways. Semin Immunol 1997; 9:93-107
[7] Liles WC, Kiener PA, Ledbetter JA, et al. Differential expression of Fas (CD95) and Fas ligand on normal human phagocytes: implications for the regulation of apoptosis in neutrophils. J Exp Med 1996; 184:429-440
[8] Jones J, Morgan BP. Apoptosis is associated with reduced expression of complement regulatory molecules, adhesion molecules and other receptors on polymorphonuclear leukocytes: functional relevance and role in inflammation. Immunology 1995; 86:651-660
[9] Dalhoff K, Braun J, Wiessmann KJ, et al. Bronchoskopische Pneumoniediagnostik mit quantitativer Keimzahlbestimmung. Dtsch Med Wochenschr 1990; 115:1459-1465
[10] Dalhoff K, Hansen F, Dromann D, et al. Inhibition of neutrophil apoptosis and modulation of the inflammatory response by granulocyte colony-stimulating factor in healthy and ethanol-treated volunteers. J Infect Dis 1998; 178:891-895
[11] Watson RW, Rotstein OD, Jimenez M, et al. Augmented intracellular glutathione inhibits Fas-triggered apoptosis of activated human neutrophils. Blood 1997; 89:4175-4181
[12] Whyte MKB, Hardwick SJ, Meagher LC, et al. Transient elevation of cytosolic free calcium retard subsequent apoptosis in neutrophils in vitro. J Clin Invest 1993; 92:446-455
[13] Hustinx WNM, Van Kessel CPM, Heezius E, et al. Effects of granulocyte colony-stimulating factor (G-CSF) treatment on granulocyte function and receptor expression in patients with ventilator-dependent pneumonia. Clin Exp Immunol 1998; 112:334-340
[14] Anderson DC, Springer TA. Leukocyte adhesion deficiency: an inherited defect in the Mac-1, LFA-1, and p150,95 Glycoproteins. Ann Rev Med 1987; 38:175-194
[15] Cox G, Gauldie J, Jordana M. Bronchial epithelial cell-derived cytokines (G-CSF and GM-CSF) promote the survival of peripheral blood neutrophils in vitro. Am J Respir Cell Mol Biol 1992; 7:507-513
[16] Colotta F, Re F, Polentarutti N, et al. Modulation of granulocyte survival and programmed cell death by cytokines and bacterial products. Blood 1992; 80:2012-2020
[17] Tazi A, Nioche S, Chastre J, et al. Spontaneous release of granulocyte colony-stimulating factor (G-CSF) by alveolar macrophages in the course of bacterial pneumonia and sarcoidosis: endotoxin-dependent and endotoxin-independent G-CSF release by cells recovered by bronchoalveolar lavage. Am J Respir Cell Mol Biol 1991; 4:140-147
[18] Matute-Bello G, Liles WC, Radella F. Neutrophil apoptosis in the acute respiratory distress syndrome. Am J Respir Crit Care Med 1997; 156:1969-1977
[19] Ertel W, Keel M, Buergi U, et al. Granulocyte colony-stimulating factor inhibits neutrophil apoptosis at the local site after severe head and thoracic injury. J Trauma 1999; 46:784-793
[20] Welte K, Gabrilove J, Bronchud MH, et al. Filgastrim (r-metHuG-CSF): the first 10 years. Blood 1996; 88:1907-1929
[21] Watson RW, Rotstein OD, Parodo J, et al. Impaired apoptotic death signaling in inflammatory lung neutrophils is associated with decreased expression of interleukin-1 beta converting enzyme family proteases (caspases). Surgery 1997; 122:163-172
Daniel Droemann, MD; Sven P. Aries, MD; Friederike Hansen, MD; Mareike Moellers; Joerg Braun, MD; Hugo A. Katus, MD; and Klaus Dalhoff, MD
(*) From the II. Department of Medicine, Medical University Luebeck, Luebeck, Germany.
Manuscript received July 14, 1999; revision accepted February 3, 2000.
Correspondence to: Klaus Dalhoff, MD, Medizinische Klinik II, Med. Universitat Lubeck, Ratzeburger Allee 160, D-23538 Lubeck, Germany
COPYRIGHT 2000 American College of Chest Physicians
COPYRIGHT 2000 Gale Group