Abstracts presented at ARVO demonstrate the effectiveness of the fourth generation.
Infections are among tne most common disease processes affecting the eyes. They can range from mild infections that are essentially self-limiting to severe sight-threatening conditions that require aggressive measures to preserve sight. Thus, the ability to prescribe has been a boon to primary care optometrists who want to provide the highest level of care for their patients. Additionally, more and more optometrists are also involved with co-managing surgical patients. It is our responsibility then to stay abreast of the latest developments and research in anti-infective therapy so we can provide our patients the most up-to-date care.
The current standard of care in anti-infective therapy is fourthgeneration fluoroquinolones. They've been adopted by optometry due to their safety and potency. Because there is much ongoing research with these medications, I will briefly discuss in this article some of the research abstracts presented at the 2005 Association of Researchers in Vision and Ophthalmology (ARVO) meeting.
Snapshot of the resistance
Antibiotic resistance is a growing concern in all health care fields. Is it important in eye care? A laboratory study of antibiotic resistance trends from 1996 to 2004 for common antibiotics used in the treatment of conjunctivitis (Kowalski, et. al.). It found increased resistance to six antibiotics: these were bacitracin, erythromycin, gentamycin, trimethoprim, polymyxin B and sulfa.
Yet in the same study, the authors found resistance to four antibiotics had decreased; these were iprofloxacin, ofloxacin, levofloxacin and tobramycin. They noted that the fourth-generation fluoroquinolone moxifloxacin demonstrated high susceptibility for Strep. Pneumoniae and Haemophilus Influenzae and the highest susceptibility among the tested fluoroquinolones for Staph. Aureus. The other fourth-generation fluoroquinolone, gatifloxacin, was not included in this study.
Their potency is proven
We've all heard or read how much more potent the fourth-generation fluoroquinolones are when compared with their earlier counterparts. Well, recent studies bear out this finding. Researchers investigated in vitro susceptibilities of Staphylococcus species to the fluoroquinolones (Kim, et al.). They found the order of susceptibility for all Staph. species to be greatest for moxifloxacin and gatifloxacin, followed by the earlier generation fluoroquinolones.
This study suggests that the fourth-generation fluoroquinolones are more potent than the second- and third-generation fluoroquinolones for methicillinresistant Staph. aureus (MRSA).
The study also found that within the fourth-generation fluoroquinolones, moxifloxacin is more potent than gatifloxacin against all Staph. species, though the potency is equal for both the fourth-generation fluoroquinolones for MRSA. Another study (Hedlin and Blondeau) found gatifloxacin to provide a much faster and complete killing of Haemophilus Influenzae than did earlier generation fluoroquinolones. Moxifloxacin was not included in this study.
The preservative factor
What effect do preservatives have on these antibiotics? Vigamox (moxifloxacin HCI ophthalmic solution, Alcon) is a self-preserved antibiotic; is that effective? Investigators attempted to culture bacteria from 40 bottles of Vigamox used by patients post-operatively for one week following cataract surgery (Hass, et al.). They found no bacterial growth on culture from any of the bottles tested, so clearly the self-preservative works for the period of this study.
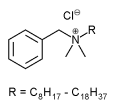
What about benzalkonium chloride (BAK), used in Zymar (gatifloxacin ophthalmic solution, Allergan)? What effect, if any, does BAK have on the antibiotic? J.M. Blondeau, et al., compared gatifloxacin with and without BAK against several ocular pathogens, including Staph., Streptococci, Haemophilus and Pseudomonas. They found the presence of varying concentrations of BAK with gatifloxacin resulted in a reduction in the minimum inhibitory concentrations (MICs) of clinically bacterial pathogens. They concluded that BAK has an additive effect when used with gatifloxacin in reducing bacterial MICs in vitro and "this observation may have important clinical implications."
We use the fourth-generation fluoroquinolones in our cataract patients for pre-operative prophylaxis. And prescribing fluoroquinolones prophylactically following surgery is now considered the standard of care.
Inside the eye
Ever wonder which antibiotic has a greater concentration in the anterior chamber? J.D. Aronowicz took aqueous humor samples from 46 eyes when the anterior chamber was open for phacoemulsification. All had been pre-operatively treated with either moxifloxacin or gatifloxacin. His study concluded that "moxifloxacin in the commercial preparation Vigamox resulted in a statistically significant greater penetration of fourthgeneration fluoroquinolone into the aqueous humor compared with gatifloxacin in commercial Zymar." Another abstract of fifty patients undergoing cataract extraction produced similar results.
The fourth-generation fluoroquinolones also achieved greater conjunctival tissue penetration than ofloxacin or ciprofloxacin in results from a separate study (R.S. Wagner, et. al.). The authors looked at 54 patients administered fluoroquinolones 20 minutes prior to conjunctival biopsy. They conclude "moxifloxacin's conjunctival depot effect may enhance treatment of bacterial conjunctivitis compared with other fluoroquinolones."
What about healing?
What about wound healing and toxicity? Anything that will impede the wound from healing (such as corneal toxicity) is a concern for the clinician. How do the fourth-generation fluoroquinolones impact these two factors? In a study comparing the healing rate of 35 subjects treated with fourth-generation fluoroquinolones following photorefractive keratectomy, the authors concluded that while mean healing time for both groups was four days, "eyes treated with Vigamox healed faster and had smaller defects compared to those with Zymar." In an animal study, gatifloxacin was found to have better epithelial healing time versus moxifloxacin.
In a study comparing fluoroquinolone toxicity in vitro with corneal and conjunctival cells in culture, all the topical fluoroquinolones tested showed evidence of both corneal and conjunctival toxicity. Moxifloxacin showed the least amount of toxicity and was the only statistically significant antibiotic; all other fluoroquinolones were statistically indistinguishable. Whether these findings translate to in vivo wound healing remains to be seen.
The jury is still out
It's important to remember the studies described above appeared as abstracts and many have yet to be published in respected journals. Cleary, in order for the validity of these findings to be established, these abstracts have to pass the rigors of the peer review process to become published studies. When asked to evaluate an animal model or in vitro model and derive some clinical relevance, it becomes apparent that in many cases there isn't strong clinical relevance.
Given that for some conditions it may not be practical to use human subjects, however, we should then look carefully at animal models in the peer-reviewed literature to see if we can derive any clinical significance.
However, current research makes some things clear. It demonstrates that fourth-generation fluoroquinolones are superior in their potency, show less bacterial resistance and are less toxic to the eye than the options that were previously available to us. They represent the best products commercially available to us in the battle against ocular infection.
References available on request.
BY ERNEST L. BOWLING, O.D., M.S., F.A.A.O., DIPL.
Summerville, Ga.
Dr. Bowling is optometric editor of Boucher Communication's Internet newsletters Diagnostic Digest and Comprehensive Optometry. He is a primary care diplomate of the American Academy of Optometry and is in private practice.
Copyright Boucher Communications, Inc. Oct 2005
Provided by ProQuest Information and Learning Company. All rights Reserved