Abstract
Background: There are no published studies examining either the effectiveness of topical steroids in the treatment of stasis dermatitis or indicating what steroid strength or duration of treatment is optimal to treat this common condition.
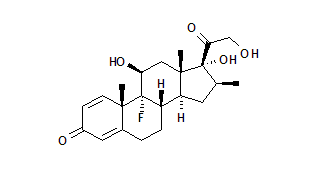
Objective: To investigate the efficacy of twice-daily application of the topical steroid betamethasone valerate 0.12% foam for the treatment of stasis dermatitis.
Design: 42-day randomized, double-blinded, vehicle-controlled, pilot study.
Settings: Outpatient dermatology clinic at a university-affiliated clinic.
Subjects: 19 subjects, mean age of 73, with mild to moderate bilateral stasis dermatitis.
Intervention: Twice-daily application of betamethasone valerate 0.12% foam versus vehicle foam to bilateral randomly assigned lower legs for 28 days with follow-up to day 42.
Main Outcome Measures: The primary clinical endpoints were the mean change in erythema, scale, swelling, petechiae, post-inflammatory hyperpigmentation, and self-reported pruritus, assessed on a 5-point Likert scale (0 = clear, 1 = almost clear, 2 = mild, 3 = moderate, 4 = severe). Secondary endpoints were changes in health related quality of life (HRQL) using the EuroQol-5D (EQ-5D) utility score and visual analog scale (VAS) and the Dermatology Life Quality Index (DLQI).
Results: Although there was no overall difference between the foam and vehicle-treated leg at days 14 and 28, the steroid-treated leg, but not the vehicle-treated leg, showed statistical improvement over baseline. Improvement in the steroid-treated leg was statistically better than vehicle at days 14 and 28 in terms of erythema (P < .05) and petechiae (P < .05). Improvement in VAS was notable at days 14 (7.1%), 28 (9.7%), and 42 (9.6%) (P < .001). Similarly, there was a statistically significant improvement in the DLQI compared to baseline on visit days 14 (188.9%) and 28 (126.1%) (P < .001).
Conclusions: This study suggests that betamethasone valerate 0.12% foam is an effective and well-tolerated short-term treatment of stasis dermatitis, but that higher potency steroids may be needed to achieve better efficacy. Furthermore, these results are the first to suggest that the application of effective topical anti-inflammatory therapy can lead to improvement in HRQL.
**********
Introduction
Stasis dermatitis, a common inflammatory skin disease, affects approximately 7% of individuals over 50 years of age. (1,2) Although the fundamental problem is venous stasis, the capillaritis that often follows can lead to eczematous changes of the lower extremity. (3) These changes are most commonly found on the medial ankle and can be acute, subacute, or chronic. In the acute phase, physical examination may reveal erythematous, pruritic plaques with weeping, and crusting. (4) In contrast, chronic inflammation can result in ulceration, hyperpigmentation due to deposition of hemosiderin, and lipodermatosclerosis due to sclerosis of the subcutaneous tissue from fat necrosis. (5) Persistent rubbing, in an effort to alleviate the discomfort associated with the disease, can lead to lichenification and hyperpigmentation.
Traditional treatments have included compression, topical therapy, and occlusive dressings. Topical corticosteroids and non-medicated emollients are thought to reduce pruritus and inflammation. (6-11) Despite the lack of reports or randomized studies examining the efficacy of topical corticosteroids, they remain a mainstay of treatment based on the principle that the dermatitic component is, at least in part, a variant of eczematous dermatitis.
There has also been no controlled assessment of the impact of stasis dermatitis on the subjects' health related quality of life (HRQL). HRQL defines the functional effect of an illness and its therapy as perceived by the subject. It serves as a useful tool for measuring the impact of a chronic disease on a subject's life because it represents the summation of functional health, well-being, and participation.
The objective of this study was to assess the use of betamethasone valerate 0.12% in a unique foam delivery as a treatment for stasis dermatitis, both in terms of clinical improvement and change in HRQL.
Patients and Methods
Subjects
Patients were recruited from dermatology and non-dermatology clinics in an academic medical center. Twenty-three subjects over 18 years of age, who spoke English, with mild-to-moderate bilateral stasis dermatitis, were enrolled. Nineteen subjects (82.6%) completed the study. The protocol and survey instruments were approved by the Panel on Human Subjects in Medical Research at Stanford University School of Medicine.
Subjects who met eligibility criteria and consented to participate served as their own controls. Betamethasone valerate 0.12% foam and vehicle foam were randomly assigned in a double-blind fashion for application to the right and left leg. Subjects were examined at an initial screening visit, day 0, and at days 7, 14, 28, and 42. Treatment was stopped after day 28. Subjects were evaluated at day 42 for follow-up and final assessments.
Outcome Measures
Clinical improvement was measured by 6 criteria: erythema, scale, swelling, petechiae, post-inflammatory hyperpigmentation, and self-reported pruritus. Measurements were on a 5-point Likert scale (0 = clear, 1 = almost clear, 2 = mild, 3 = moderate, 4 = severe).
HRQL was measured using self-response to a questionnaire that included the Euro-Qol 5D (EQ-5D) (12) and the Dermatology Life Quality Index (DLQI). (13) The EQ-5D is a standardized and validated generic model for quantifying health states and has been described in a previous paper by 2 of the authors. (14) The DLQI is a self-administered, validated questionnaire designed for use with adults and usually completed in 1 to 2 minutes. The total score is calculated by adding the score of each question. The DLQI results in a score range of 30 to 0. The higher the score, the more quality of life is impaired. The DLQI can also be expressed as a percentage of the maximum possible score of 30. (15)
Statistical Analysis
For each dependent variable, ie, clinical improvement, EQ-5D (utility and visual analog scale [VAS] score) and DLQI, a stepwise multiple linear regression analysis was performed to determine which, if any, of the independent variables, ie, age, sex, race, use of compression stockings, total mass of betamethasone valerate 0.12% foam used, were significant explanatory/predictor variables. Spearman's rank correlation coefficient was used to assess associations between continuous variables. Difference in clinical improvement between the treated and control areas was assessed using a paired samples t-test. P values [less than or equal to] .05 were considered to indicate a significant difference and are presented throughout.
Results
Subject Characteristics
Table 1 provides the socio-demographic characteristics of the 19 subjects who completed the study. The mean age was 71.3 years. Thirteen subjects (68.4%) were male and the majority (78.9%) were Caucasian. Four subjects (21.1%) had used compression stockings prior to enrolling and continued to use them throughout the study. The baseline severity score in the treated leg was 2.1 and in the vehicle leg 2.2 (P = .59) (Table 2). The average mass of betamethasone foam used by each subject was 138.7 g compared to the 132 g (P = 0.62) of vehicle foam. Three of the 4 subjects who dropped out of the study did so before the day 7 visit. There was no appreciable difference in the four patients who withdrew from the study compared to the 19 patients who completed the study.
Effect of therapy
The steroid-treated leg showed statistical improvement over baseline, but there was no overall difference between the steroid-treated and vehicle-treated leg at days 14 and 28. (Table 2). Most of the improvement in the steroid-treated leg occurred because of reductions in erythema and petechiae. These improvements were not present in the vehicle-treated leg (p [less than or equal to] .05) (Table 2). At day 14, 15.8% of the legs treated with betamethasone valerate 0.12% foam were considered clear or almost clear by the physician compared to only 5.3% of the vehicle-treated legs (P = .08). There were no significant differences noted in scale, swelling, post-inflammatory hyperpigmentation, or pruritus between the two legs (Table 2).
In multivariate analysis, men were more likely to see improvement at day 14 (P = .05). Being Caucasian and using a larger quantity of medication were significant independent predictors of improvement at day 42 (p = 0.01, p = .02).
Patient Impact
During the length of therapy, subjects noted a beneficial change in their quality of life as measured by the EQ-5D VAS and DLQI. Improvement in VAS compared to baseline was notable at days 14 (7.1%), 28 (9.7%), and 42 (9.6%) (P < .001). Similarly, there was a statistically significant improvement in the DLQI compared to baseline on visit days 14 (188.9%) and 28 (126.1%) (P <0.001) (Table 3).
The DLQI asks specifically about 10 different aspects of life. Analysis showed that treatment had a positive affect on subjects' level of embarrassment at days 14, 0.60 units (300%, p = .02,) and 28, 0.59 units (280%, p = .01); subjects' ability to carry out chores on days 14, 0.50 units (250%; p = .02), 28, 0.54 units (343%; p = .01), and 42, 0.44 units (166%; p = .04); subjects' leisure activities on days 14, 0.40 units (400%; p = .04) and 28, 0.39 units (375%; p = .04); subjects' interaction with their partner on day 28, 0.20 units (375%; p = .04); and subjects' choice of clothes on day 28, 0.43 units (137.5%; p = .05). Two weeks after the medication was discontinued at day 42, there was no significant difference in the DLQI compared to baseline.
The only socio-demographic characteristic predictive of change in HRQL was race. In multivariate analysis, at day 14, Caucasians were more likely to see improvement in the EQ-5D utility score (p = .01).
In terms of how HRQL related to clinical improvement, at day 14, the reduction in erythema was correlated with the improvement from baseline in the EQ-5D utility score (r = -.58, p = .007). At day 28, the reduction in erythema (r = -.57, p = .01) and scale (r = -.56, p = .01) correlated with the improvement from baseline in the VAS.
Adverse Events
No serious adverse events were encountered during the study. Four subjects (21.1%) reported burning after application of foam, but stated that it resolved upon drying. Of those 4 patients, all 4 complained of burning upon application of the vehicle foam, but only 2 complained of burning upon application of the medicated foam. To the question of whether the treatment was bothersome (DLQI question 10), the median response at all time points was not at all.
Discussion
Stasis dermatitis is a chronic condition that affects a significant proportion of the population. Although anti-inflammatory therapy is a commonly used therapeutic option, there have been no reports or randomized studies examining its efficacy that can be used to establish clinical recommendations regarding dose or duration of therapy. This study demonstrates that use of topical steroids can acutely alleviate some of the physical symptoms of stasis dermatitis, with the most pronounced change in disease noted 2 weeks after initiating therapy.
By day 14, the leg treated with betamethasone valerate 0.12% foam demonstrated clinical improvement in 2 dimensions when compared to the leg treated with vehicle. Not surprisingly, given the anti-inflammatory properties of steroids, the changes were most pronounced in erythema and petechiae. However, the improvement was not sustained. At day 42, 14 days after study medication was withdrawn, no difference could be detected when the treated leg was compared both to baseline and to the vehicle leg. Additionally, given the mild to moderate degree of clinical improvement, it may be appropriate to consider higher strength topical steroids.
Application of a topical therapy in a dermatitic condition can be uncomfortable, especially initially. In this study, despite the fact that the lower legs are commonly xerotic in the elderly, the foam vehicle was generally well-tolerated. Only 2 subjects complained of burning in the treated leg and only 2 additional subjects complained about the vehicle foam. Furthermore, when asked whether the treatment was bothersome in terms of impact on quality life, participants generally felt that it was without impact. There were no other significant adverse events reported.
Second, previous to this study, there had not been any controlled assessment of the impact of stasis dermatitis on subjects' HRQL. Our study illustrates that the effect of stasis dermatitis is substantial using 3 standard metrics that evaluate well-being. The subjects' self-perceived health status improved significantly throughout the course of the trial, as measured by EQ-5D VAS score. The DLQI was also found to improve on visit days 14 and 28. Yet, after medication was discontinued and clinical scores neared baseline, the DLQI was not significantly different than baseline, suggesting that subjects with stasis dermatitis associate a lower quality of life and health status with their disease severity.
Finally, this study suggests that the subjective experience of stasis dermatitis is significant, because during the course of the trial there were significant daily life improvements. Although only one leg received medicated treatment during the study, both steroid-treated and vehicle-treated legs improved and we found a corresponding improvement along 2 different metrics of QOL. Subjects' clinical improvements were associated with an increased desire to carry out leisurely activities, improved interactions with their partners, and decreased embarrassment levels throughout the course of treatment. Additionally, the subjects found that use of the medication decreased their preoccupation with choice of clothing for their lower legs. This suggests that because stasis dermatitis can have such a pronounced effect on QOL, even mild improvement can produce substantial gains in QOL.
The primary limitation of our study is the nature of the population of subjects. The sample size is small and therefore may not be representative of the general population with stasis dermatitis. Patients who seek experimental care at a major academic medical center possibly have a perception of greater disease severity than the general population. Moreover, those that seek care at academic medical centers are likely frustrated with the therapies previously prescribed in the community, possibly topical steroids in different vehicles. Lastly, studies with an effective vehicle, such as this one, may require significantly larger populations to establish a definitive treatment effect; larger studies could be performed to determine an optimal treatment regimen.
Our findings, like those of studies in other dermatologic diseases, (13,14) reinforce the concept that the severity of dermatologic disease must include both physical and psychosocial measures of severity. Patients with stasis dermatitis often believe that their current health state is less than ideal. This study provides evidence of the effectiveness of betamethasone foam over placebo in the treatment of stasis dermatitis, suggesting for the first time in a vehicle-controlled clinical trial that treating stasis dermatitis with topical steroids is valuable. Furthermore, these results suggest that the application of topical anti-inflammatory therapy can lead to improvements in HRQL. Continued efforts to evaluate dermatologic therapy both on its therapeutic efficacy and its ability to improve a subject's overall HRQL are important aspects of ongoing clinical research.
(A portion of this data was presented in poster form at the American Academy of Dermatology Annual Meeting, March 2003.)
Funding sources: Unrestricted grant from the Connetics Corporation.
Disclosure: Dr. Kimball has served as a consultant and received honoraria for speaking from the Connetics Corporation.
References
1. Beauregard S, Gilchrest BA. A survey of skin problems and skin care regimens in the elderly. Arch Dermatol. 1987;123:1638-43.
2. Weismann K, Krakauer R, Wanscher B. Prevalence of skin diseases in old age. Acta Derm Venereol. 1980;60:352-3.
3. Behrman HT, Labow TA, Rozen JH, ed. Common Skin Diseases: Diagnosis and Treatment. 3rd ed. New York, NY: Grune and Stratton, Inc; 1978:107.
4. Odom RB, James WD, Berger TG. Cutaneous vascular diseases. In: Fathman EM, Geisel EB, editors. Andrews' Diseases of the Skin. 9th ed. Philadelphia, PA: W.B. Saunders; 2000:1051-2.
5. Habif TP. Eczema and hand dermatitis. In: Baxter S, ed. Clinical Dermatology. 3rd ed. St. Louis, MO: Mosby; 1996. p. 74-8.
6. Torrence BP, Hovanec R, Bartunek C, Brodell RT. Stasis dermatitis: practical pearls for the dermatologic nurse. Dermatol Nurs. 1993;5:186-91, 208.
7. Dillon RS. Treatment of resistant venous stasis ulcers and dermatitis with the end-diastolic pneumatic compression boot. Angiology. 1986;37:47-56.
8. Tam M, Moschella SL. Vascular skin ulcers of limbs. Cardiol Clin. 1991;9:555-63. Review.
9. Fisher AA. The role of topical medications in the management of stasis ulcers. Angiology. 1971;22:206-10.
10. Valencia IC, Falabella A, Kirsner RS, Eaglstein WH. Chronic venous insufficiency and venous leg ulceration. J Am Acad Dermatol. 2001;44:401-21.
11. Choucair M, Phillips TJ. Compression therapy. Dermatol Surg. 1998;24:141-8.
12. EuroQol Group. EuroQol-a new facility for the measurement of health related quality of life. Health Policy. 1990;16:199-208.
13. Finlay AY, Khan GK. Dermatology Life Quality Index (DLQI): a simple practical measure for routine clinical use. Clinical and Experimental Dermatology. 1994;19:210-16.
14. Weiss SC, Kimball AB, Liewehr DJ, Blauvelt A, Turner ML, Emanuel, EJ. Quantifying the harmful effect of psoriasis on health-related quality of life. J Am Acad Dermatol. 2002;47:512-18.
15. Herd RM, Tidman MJ, Ruta DA, Hunter JA. Measurement of quality of life in atopic dermatitis: correlation and validation of two different methods. Br J Dermatol. 1997;136:502-07.
Stefan C. Weiss MD MHSc, (a) Josephine Nguyen MD, (a) Susan Chon MD, (b) Alexa B. Kimball MD MPH (c)
a. Department of Dermatology, Stanford University Medical Center, Stanford, CA
b. Department of Dermatology, MD Anderson Cancer Center, Houston, TX
c. Department of Dermatology, Harvard University Medical Center, Boston, MA
Address for Correspondence
Alexa B. Kimball MD MPH
275 Cambridge Ave., P.O. Box 4
Boston, MA 02114
Phone: 617-726-6755
Fax: 617-507-3096
e-mail: akimball@partners.org
COPYRIGHT 2005 Journal of Drugs in Dermatology, Inc.
COPYRIGHT 2005 Gale Group