An in-depth look at the side effects that come with glaucoma treatments, as well as tips to manage these effects.
The primary goal in the medical management of glaucoma is to slow the progressive optic nerve damage and associated visual field loss to the point where your patient will maintain his visual function for the duration of his life. Unfortunately, patients often don't notice any deterioration in vision in the early stages of glaucoma, nor do they experience any ocular discomfort. Also, some of the therapeutic agents we commonly use are accompanied by unwanted side effects.
This article will discuss some of those complications as well as strategies you can use to minimize their impact on your patients' health and well being.
Tolerability vs. safety
The first thing to do when considering complications of the medical management of glaucoma is to consider the difference between tolerability and safety issues. Tolerability issues are generally those that aren't life-threatening or health-damaging. They include burning, stinging, hyperemia, etc.
In general, patients don't necessarily have to stop taking these medications for tolerability issues. Some of these issues resolve with time; others the patient must learn to live with. If the patient refuses, then you must consider alternative therapy. Safety issues, however, do threaten a patient's health and typically necessitate cessation of therapy.
The issues of safety and tolerability are prevalent in all four commonly prescribed drug classes we have in our arsenal to treat glaucoma:
1. alpha-adrenergic agonists
2. beta adrenergic antagonists
3. carbonic anhydrase inhibitors
4. prostaglandin analogs.
Alpha-adrenergic agonists
The only useful agent in this class is brimonidine, which works by a dual mechanism of decreasing aqueous humor production and increasing uveoscleral outflow. Brimonidine (0.2% Alphagan and 0.15% Alphagan P with Purite preservative) is indicated for t.i.d. dosing, but is frequently dosed b.i.d. - presumably to aid in patient compliance.
* Side effects. Patients typically tolerate brimonidine well. The most common ocular side effects relate to discomfort (ocular allergy, burning and stinging), which 10% to 25% of patients report.
Brimonidine has a lipophilic nature, which means that there's a possibility of some central nervous system side effects, including sedation. Other systemic side effects include dry mouth in nearly one-third of patients, and fatigue and drowsiness in less than 5% of cases, as well as a few reports of headaches. Avoid using brimonidine in infants and in small children who have juvenile glaucoma because the literature has reported apneic spells and cyanosis.
Carbonic anhydrase inhibitors
Topical carbonic anhydrase inhibitors (CAIs) lower IOP by inhibiting aqueous humor formation through the reversible and noncompetitive binding of the enzyme carbonic anhydrase. The first agent in this class was dorzolamide (Trusopt) but a more recent agent (brinzolamide [Azopt]) has become available.
* Side effects. Adverse ocular reactions of topical CAIs includes burning and stinging upon instillation, foreign body sensation, superficial punctate keratopathy and allergic blepharoconjunctivitis. Some of the stinging on instillation is related to the active ingredients of the medication, but some results because this medication is kept at a low pH (5.8) to keep the relatively insoluble compound in solution.
Systemic side effects included digestive system disturbances such as diarrhea, nausea and gastroenteritis. One fairly common systemic effect is a bitter taste after administration, which approximately 25% of patients notice. Use caution when prescribing this type of drug for patients who have sulfa allergy.
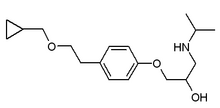
Beta blockers
Five fairly distinct formulations of topical beta blockers are available in the United States (see below) with additional preparations available in generic formulations.
1. timolol (various trade names)
2. levobunolol HCl (various trade names)
3. carteolol HCl (Ocupress)
4. betaxolol HCl (Betopic S)
5. metipranolol HCl (OptiPranolol)
Generally speaking, you can prescribe these beta blockers for once-a-day dosing instead of the traditional b.i.d. schedule. The one notable exception to this rule is African-American patients, who will still require the 0.5% solution and b.i.d. dosing.
The most likely mechanism on how beta-blockers decrease IOP is through the suppression of the formation of aqueous humor. Most patients demonstrate a 20% to 40% lowering of IOP when started on topical beta-blockers.
* Side effects. The most common ocular complaint with the use of beta blockers is transient stinging and burning. Other commonly reported symptoms associated with topical beta blockers include blurred vision, foreign body sensation, photophobia, itching and ocular irritation. Objective ocular signs consist of superficial punctate keratitis, keratitis sicca, corneal hypoesthesia, lid ptosis and allergic blepharoconjunctivitis.
Because many glaucoma patients also have other systemic medical conditions, do some serious thinking before initiating or changing treatment. Beta blockers in particular can possibly induce significant systemic side effects because these receptors exist not only in the eye, but also in organs throughout the body. Unintentional interference with these receptors can produce adverse pulmonary, cardiovascular, neurological/psychiatric and metabolic side effects. Experts have estimated that roughly 80% of an eye drop passes through the nasal nasolacrimal ducts and into the nasal mucosa and its microvasculature. Over the long term, this can present problems for the patient.
In the respiratory system, beta blockers cause bronchoconstriction. For this reason, the nonselective beta blockers (timolol, levobunolol, metipranolol and carteolol) are contraindicated in patients who have a history of reactive airway diseases such as asthma, emphysema and chronic bronchitis.
Betaxolol, which is a selective beta blocker, is theoretically safer than the other agents in this group. However, research has demonstrated that betaxolol can compromise breathing in patients who have pre-existing lung disease, so this drug is still a relative contraindication.
Beta blockers can also cause a reduction in heart rate as well as the contractile force of the heart. This combination of effects decreases cardiac output, which partially explains why beta blockers lower blood pressure. Lowered blood pressure can become a problem in the elderly because excessive blood pressure reduction can cause cerebral hypoperfusion and syncope and decreased perfusion of the heart can lead to angina, myocardial infarction and even death.
If these patients already have compromised myocardial function and they start taking beta blockers, they may suffer from congestive heart failure, heart block or bradyarrythmias. It can also become a problem for athletes.
Beta blockers can cause or worsen clinical depression by blocking these beta receptors and decreasing the concentrations of catecholamines and serotonin. In terms of the glaucoma medication, most of these systemic side effects have been seen with timolol use. It's unknown if this observation is caused by the drug's high lipophilic nature or merely by a reflection of the fact that timolol is the most widely used drug in this class.
Both oral and topical beta blockers are a relative contraindication when treating diabetic patients. The reason for this is that adrenergic outflow and beta receptors are important in the symptomatic and physiological response to hypoglycemia. Beta blockers may mask some of these signs and symptoms of hypoglycemia and could seriously delay the physiological response to an insulin reaction.
Lastly, topical beta blockers can affect how the body metabolizes lipids, which may result in increased serum levels of triglycerides and decreased high-density lipoproteins. According to most studies, carteolol has the least negative effect on high-density lipoproteins of the beta blockers.
Prostaglandins
Three basic drugs are available in this class:
1. latanoprost (Xalatan)
2. travaprost (Travatan)
3. bimatoprost (Lumigan).
The precise location that accounts for the IOP-lowering effect of the prostaglandin analogs is unknown, but experts believe it to be the ciliary muscle. They also believe that prostaglandins lower IOP by increasing uveoscleral outflow. The precise mechanism is unknown but is believed that the effect is related to structural modification of the extracellular matrix in the ciliary muscle and/or by the relaxation of the ciliary muscle.
Latanoprost is a pro-drug and has generally less ocular side effects than other prostaglandins. Latanoprost also has a half life of 17 minutes, so it quickly converts to an inactive metabolite in the liver and the patient rapidly excretes it in his urine. The lack of systemic action of this agent is demonstrated by the observation that there is no contralateral IOP-lowering effect, as there is with the beta blockers.
* Side effects. Adverse reactions include conjunctival hyperemia, eyelash thickening and elongation and iris discoloration. The iris discoloration, however, has been widely reported on this drug. It appears in roughly 7% to 12% of patients, but is most common in patients who have mixed-colored irises - most often green/brown or blue/gray/ brown. It's rare in patients who have solid-colored (pure blue or pure brown) irises. The iris discoloration most likely starts roughly 18 weeks to 26 weeks after initiation of treatment and is not reversible upon discontinuation of therapy. The pathogenesis behind this reaction is one of increased amount of melanin within the melanocyte - not an increase in the number of melanocytes. From a clinical standpoint, it doesn't harm the patient; however, you should warn patients who have mixed-color irises about this effect before you initiate therapy.
In addition to iris discoloration, some patients on latanoprost therapy have reported mild punctate corneal epithelial erosions, iritis and cystoid macular edema (CME). CME is often associated with either a prior history of CME, lens capsule rupture or some other ocular complication of ocular surgery. Other rare side effects include the possibility of migraine headaches and exacerbation of Herpes simplex corneal infections.
Systemic side effects are typically rare and minor. They include upper respiratory signs, muscle or joint pain and nonocular allergy or eczema.
Travoprost is a prostaglandin F-2 alpha analog with a chemical structure closely resembling latanoprost. However, travoprost has a higher rate of ocular hyperemia (up to 50% of patients) and the incidence of iris pigment changes are lower (about 3%). During the clinical studies, this product demonstrated a greater IOP-lowering effect in African-American patients; researchers are currently studying this effect.
Bimatroprost mildly stimulates the rate of aqueous flow by 13% to 14%, but still causes a 26% to 30% reduction in tonographic resistance to outflow, an increase in uveoscleral outflow and a lowering of the episcleral venous pressure. Bimatoprost has less incidence of iris discoloration, but a significantly higher incidence of hyperemia than any other drug in this class. In some cases, the hyperemia resolves after several weeks.
It all relates to education
Managing glaucoma complications starts with proper practitioner education. With the wide diversity of therapeutic agents on the market, we're better able than ever before to tailor treatment plans based on a patient's individual needs. And doing so will avoid the vast majority of complications altogether.
When complications do occur, we must educate patients about the ongoing need for therapy to prevent blindness. Depending on the severity, a different class of medication may be prescribed or the patient may be educated to endure the adverse reaction.
References available on request
BY DEEPAK GUPTA, O.D., F.A.A.O.
Stamford, Conn.
Dr. Gupta practices full-scope optometry and is clinical director of the Optometric Glaucoma Referral Center. Contact him at deegup4919@hotmail.com.
Copyright Boucher Communications, Inc. Aug 2004
Provided by ProQuest Information and Learning Company. All rights Reserved