Study objectives: Hypoxemia increases corrected QT dispersion (QTcD), which is the difference between the maximum and minimum QT intervals and is a strong risk factor for cardiovascular mortality. The aim of this study was to investigate the QTcD in patients with obstructive sleep apnea-hypopnea syndrome (OSAHS), and the relationship between the QTcD and [sup.123]I-metaiodobenzylguanidine (MIBG) cardiac imaging, which reflects cardiac sympathetic activity.
Setting: A university hospital.
Patients: Forty-eight OSAHS patients without cardiac diseases (mean [[+ or -] SD] age, 45.9 [+ or -] 10.8 years; apnea-hypopnea index [AHI] 51.9 [+ or -] 18.5 events per hour) who underwent polysomnography before treatment and on the first night of nasal continuous positive airway pressure (nCPAP) treatment.
Methods: Before and after nCPAP treatment was started, we measured the QTcD with computer software, before, during, and after sleep, as well as the washout rate of the MIBG administered for cardiac imaging. As a control, QTcD was also measured in the morning from 26 healthy subjects.
Results: Before treatment, the mean QTcD during sleep (65.0 [+ or -] 14.6 ms) was greater than that before sleep (57.0 [+ or -] 13.5 ms; p < 0.0001). Meanwhile, after 1 night of nCPAP therapy, the QTcD during sleep (50.6 [+ or -] 11.4 ms) decreased from that before treatment (p < 0.0001) and was smaller than the QTcD before sleep (56.2 [+ or -] 13.3 ms; p = 0.003). Before treatment, the QTcD during sleep correlated with the AHI (r = 0.38; p = 0.009) and the percentage of time that Sa[0.sub.2] was < 90% (Sa[O.sub.2] < 90% time) [r = 0.34; p = 0.018]. The QTcD did not correlate with the body mass index or the washout rate of MIBG. However, the washout rate of MIBG correlated with the AHI and the Sa[O.sub.2] < 90% time.
Conclusions: Nocturnal QTcD is increased in OSAHS patients but is decreased by nCPAP therapy independently of cardiac sympathetic function.
Key words: cardiac sympathetic function; corrected QT dispersion; iodine-123-metaiodobenzylgunidine imaging; nasal continuous positive airway pressure treatment; obstructive sleep apnea-hypopnea syndrome
Abbreviations: AHI = apnea-hypopnea index; BMI = body mass index; MIBG = [sup.123]I-metaiodobenzylguanidine; nCPAP = nasal continuous positive airway pressure; OSAHS = obstructive sleep apnea-hypopnea syndrome; QTcD = corrected QT dispersion; Sa[O.sub.2] = arterial oxygen saturation; Sa[O.sub.2] < 90% time = percentage of time that arterial oxygen saturation was below 90%; WR = washout rate
**********
An increase in cardiovascular mortality has been suggested in untreated patients with obstructive sleep apnea hypopnea syndrome (OSAHS), (1) and mortality was decreased with nasal continuous positive airway pressure (nCPAP) therapy. (2) Some large prospective studies (3-5) have demonstrated that OSAHS has a close relationship with hypertension, cardiac failure, and myocardial infarction.
QT dispersion, which is the difference between the maximum and minimum QT intervals on ECG, reflects inconsistencies in ventricular repolarization and myocardial electrical instability. (6) A large prospective study (the Rotterdam Study) (7) has demonstrated that an increased corrected QT dispersion (QTcD) [> 60 ms] is a strong and independent risk factor for cardiac mortality. QTcD is increased by blood gas derangement (8) and sympathetic strain. (9) OSAHS patients experience apnea-related repetitive hypoxemia during sleep (10) and elevated cardiac sympathetic activity, as assessed by [sub.123]I-metaiodobenzylguanidine (MIBG) imaging. (11) However, no report has examined the relationship between OSAHS and the QTcD.
We hypothesized that the QTcD would be in creased during sleep in OSAHS patients with repetitive apnea-related blood gas derangements and that the elevated QTcD would improve with nCPAP therapy. To test this hypothesis, we examined the QTcD during sleep in OSAHS patients who did not have cardiac disease prior to nCPAP treatment, on the first night of nCPAP treatment, and after 1 month of nCPAP treatment. In addition, we examined the relationships among QTcD, the degree of hypoxemia, and cardiac sympathetic activity, as assessed by MIBG imaging.
MATERIALS AND METHODS
Study Population
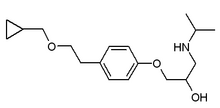
We examined 48 consecutive OSAHS patients (45 men and 3 women; mean [[+ or -] SD] age, 45.9 [+ or -] 10.8 years; mean body mass index [BMI], 30.2 [+ or -] 4.3 kg/[m.sup.2]), with an apnea-hypopnea index (AHI) of [greater than or equal to] 20, who had undergone nCPAP therapy. Each OSAHS patient underwent BP measurements, routine blood examinations, chest radiographs, ECG, echocardiography, Holter ECG monitoring, and arterial blood gas analysis. All of the patients in this study showed no cardiac diseases that required treatment, including arrhythmia, except for 16 patients with hypertension. This subset took various antihypertensive agents, including calcium channel blockers (amlodipine besilate, five patients; nifedipine, three patients; diltiazem hydrochloride, one patient: efonidipine hydrochloride, one patient; manidipine hydrochloride, one patient; and barnidipine hydrochloride, one patient), angiotensin-converting enzyme inhibitors (lisinopril, four patients; and alacepril, one patient), an [alpha]-blocker (doxazosin mesilate, four patients), and [beta]-blockers (atenolol, one patient; arotinolol hydrochloride, one patient; propranolol hydrochloride, one patient; and betaxolol hydrochloride, one patient) for > 1 month before the start of this study and throughout the study. None of the patients had received antiarrhythmic agents.
The mean systolic and diastolic BP values of the OSAHS patients in the morning were 122.7 [+ or -] 19.1 and 84.5 [+ or -] 12.1 mm Hg, respectively. Of the 16 patients with hypertension, 9 patients had a systolic BP of > 140 mm Hg, and 13 patients had a diastolic BP of > 90 into Hg. Holter ECG monitoring showed that 16 patients had no ventricular arrhythmia. The remaining 32 patients had premature ventricular contractions that were unifocal and infrequent. The frequency of the premature ventricular contractions was < I0 heats per 24 h in 23 patients, 10 to 100 beats per 24 h in 8 patients, and approximately 800 beats per 24 h in one patient. Echocardiography showed that left ventricular wall motion was good in all patients. The mean ejection fraction was 69.0 [+ or -] 9.1%. Five patients had mild concentric left ventricular hypertrophy (12 mm, four patients; 13 mm, one patient), possibly due to hypertension. None of the patients had apparent valvular disease. Arterial blood gas analysis of the patients with OSAHS showed a mean Pa[O.sub.2] of 80.9 [+ or -] 9.4 mm Hg and a mean PaC[O.sub.2] of 43.0 [+ or -] 3.1 mm Hg. The respiratory function test (42 patients) showed that the mean vital capacity was 110.5 [+ or -] 15.4% predicted, and the mean FE[V.sub.1]/FVC ratio was 78.6 [+ or -] 7.0%.
Eighteen patients had nun-insulin-dependent diabetes mellitus without neuropathy. They were receiving either diet therapy alone or in conjunction with oral drugs (three patients), including a sulfonylurea (glibenclamide, two patients) and [alpha]-glucosidase inhibitors (acarbose, one patient; and voglibose, one patient) for > 1 month before the start of this study and throughout the study. None of the patients were undergoing injection therapy with insulin. None of the patients had received reserpine, tricyclic antidepressants, or other drugs that may interfere with the uptake of MIBG. As control subjects, an ECG also was recorded in the morning from 26 age-matched and sex-matched healthy subjects (24 men and 2 women; mean age, 45.9 [+ or -] 13.4 years; mean BMI, 23.7 [+ or -] 2.2 kg/[m.sup.2]). We obtained informed consent from all subjects in accordance with guidelines from the Ethics Committee of the Graduate School of Medicine, Kyoto University.
Polysomnography
The OSAHS patients underwent polysomnography before treatment and again on the first night of nCPAP treatment, as previously described. (12) We asked the patients to consume consistent amounts of food and fluid during the study. Polysomnography was started at approximately 9:00 PM and ended at 6:30 AM. Surface electrodes were attached using standard techniques to obtain an EEG, an electrooculogram, an electromyogram of the chin, and a 12-lead ECG. Sleep stages were defined according to the criteria of Rechtschaffen and Kales. (13) Ventilation was monitored by inductive plethysmography (Respitrace; Ambulatory Monitoring; Ardsley, NY). Airflow was monitored by thermistors (Nihon Kohden; Tokyo, Japan) that were placed at the nose and the mouth. Arterial oxygen saturation (Sa[O.sub.2]) was monitored continuously with a pulse oximeter (Pulsox-7; Minolta; Osaka, Japan). A polygraph (Polygraph System RM-6000; Nihon Kohden) was run continuously, at 10 mm/s to record all of the above physiologic data simultaneously throughout the polysomnography. All parameters were stored in a data recorder (A-621; Sony Precision Technology; Tokyo, Japan) for subsequent analysis.
Apnea was defined as a complete cessation of airflow at the nose and mouth that lasts for [greater than or equal to] 10 s. Hypopnea was defined as a decrease of [greater than or equal to] 50% in thoracoabdominal motion that lasts for [greater than or equal to] 10 s and is associated with a fall in the baseline Sa[O.sub.2] of [greater than or equal to] 4%. All AHI values were calculated to express the number of episodes of apnea and hypopnea per hour of total sleep time. Before and after polysomnography, BP was measured three times, and the mean value was calculated. In each OSAIIS patient, the internal between the two polysomnographic examinations was [less than or equal to] 1 week. During the second polysomnography, the nCPAP pressure was titrated manually during 1 night. Each patient also underwent nCPAP treatment during polysomnography of at least 8 h.
ECG Analysis
During each polysomnography session, a simultaneous 12-lead ECG was recorded before sleep (ie, between 7:00 PM and 8:00 PM), during sleep (ie, between 19:00 PM and 1:00 AM), and after sleep (ie, between 7:00 AM and 8:00 AM). On the first night of nCPAP therapy, an ECG was recorded after nCPAP treatment was started, during nCPAP treatment, and before nCPAP treatment was stopped. All ECG also was recorded in the morning alter the application of successful nCPAP treatment for 1 month. ECG waves were recorded at a sampling frequency of 4000 Hz, were stored digitally, and were analyzed by computer software (Fukuda Denshi; Tokyo, Japan). Consecutive 60-s cycles were measured. We used the mean RR and QT intervals in all cycles of 12 leads. The QT dispersion was calculated as the mean difference between the maximum and minimum QT intervals across 12 leads in all cycles. The corrected QT interval and QTcD were calculated using the Bazett formula (corrected QT interal = QT/R[R.sup.1/2]).
MIBG Imaging
MIBG cardiac imaging was performed before treatment and on the same day of ECG examination after 1 month of nCPAP treatment, as previously described. (11) The patients with OSAHS underwent the scintigraphic study 4 to 5 h after awakening and were instructed to remain awake. Each subject received 30 mg potassium iodine daily from the day before the examination until the day after the examination to block tracer uptake in the thyroid gland. Planar images were obtained at rest in an anterior view over a 3-min interval. At 15 min after the injection of III MBq MIBG (ie, the early image) and at 3 h after (ie, the delayed image), a gamma camera equipped with a low-energy, parallel-hole, general-purpose collimator was used to make the image.
The regions of interest in the whole heart were set manually on these planar images. The mean heart counts from the early image and from the delayed image were calculated. On the planar images, a region (10 X 10 [mm.sup.2]) in the upper mediastinum was used to calculate the mean mediastinal counts for the early and late images. A previous study (11) has reported that the washout rate (WR) of MIBG in OSAHS patients is faster than the WR of healthy subjects and is normalized by 1 month of nCPAP treatment. Therefore, we used WR as an index of sympathetic tone. WR from the myocardium was determined over 3 h without correction for the physical decay of the [sup.123]I label, according to the formula:
WR (%) = ([He - Me] - [Hd - Md]) x 100/(He - Me)
where He is the mean heart count from the early image, Me is the mean mediastinal count from the early image, Hd is the mean heart count from the delayed image, and Md is the mean mediastinal count from the delayed image.
Statistical Analysis
All statistical analyses were performed using nonparametric tests with statistical software (StatView, version 5.0 for Macintosh; Abacus Concepts: Berkeley, CA). Differences between the two groups were compared with the Mann-Whitney U test. Differences between any two conditions in OSAHS patients were compared with the Wilcoxon signed rank test. When more than two conditions were compared, a significant difference was tested among all of the conditions by the Friedman test. If a significant difference was found by the Friedman test, the difference between every, pair of conditions was retested by the Wilcoxon signed rank test. Correlations between variables were analyzed by the Spearman rank correlation test. A p < 0.05 was considered to be significant. The data are expressed as the mean [+ or -] SD.
RESULTS
Effect of nCPAP Treatment on OSAHS
OSAHS was found to be reversed by 1 night of nCPAP treatment in all patients, as indicated by improvements in AHI, the mean nocturnal Sa[O.sub.2], the lowest nocturnal Sa[O.sub.2], and the percentage of time that Sa[O.sub.2] was below 90% (Sa[O.sub.2] < 90% time) (Table 1). The mean pressure used in nCPAP treatment was 11.6 [+ or -] 3.4 cm [H.sub.2]O. Systolic and diastolic BP after sleep decreased after 1 night of nCPAP treatment, although BP before sleep did not change.
QT Dispersion and QTcD
Figure 1 shows the QT dispersion and QTcD in the OSAHS patients before nCPAP treatment, after 1 night of nCPAP treatment, and after 1 month of nCPAP treatment. QT dispersion and QTcD before sleep did not change between two polysomnographic examinations in OSAHS patients (p = 0.67 and 0.56, respectively). Before treatment, the mean QTcD during sleep in OSAHS patients (65.0 [+ or -] 14.6 ms) was greater than that before sleep (57.0 [+ or -] 1:3.5 ms; p < 0.0001). Following 1 night of nCPAP treatment, the mean QTcD during sleep in OSAHS patients (50.6 [+ or -] 11.4 ms) was significantly decreased from that during sleep be[ore treatment (65.0 [+ or -] 14.6 ms; p < 0.0001). With 1 night of nCPAP treatment, the mean QTcD during sleep in OSAHS patients (50.6 [+ or -] 11.4 ms) was smaller than that before sleep (56.2 [+ or -] 13.3 ms; p = 0.00,3). Each value of the QTcD was not significantly different between subgroups of patients taking antihypertensive agents or those patients having diabetes. The relationships of the QTcD described above did not change in each subgroup of patients who were taking antihypertensive agents or had diabetes.
[FIGURE 1 OMITTED]
Before treatment, the QTcD of OSAHS patients during sleep significantly correlated with the AHI (r = 0.38; p = 0.009) [Fig 2], the mean Sao, (r = -0.43; p = 0.003) and the Sa[O.sub.2] < 90% time (r = 0.34; p = 0.018). The degree of reduction in the QTcD during sleep in OSAHS patients who had undergone 1 night of nCPAP treatment also correlated with the degree of the reduction in AHI (r= 0.35; p = 0.016). QT dispersion and QTcD before and after nCPAP treatment did not correlate with the BMI (p > 0.3).
[FIGURE 2 OMITTED]
The morning QT dispersion and QTcD in OSAHS patients before nCPAP treatment, after 1 night of nCPAP treatment, or after 1 month of nCPAP treatment did not differ from the mean morning QT dispersion (54.4 [+ or -] 14.5 ms) and QTcD (59.6 [+ or -] 16.1 ms) in healthy subjects, respectively.
MIBG Imaging
The mean WR of MIBG in OSAHS patients decreased from 33.7 [+ or -] 10.2% before nCPAP treatment to 27.8 [+ or -] 11.0% after 1 month of nCPAP treatment (p < 0.0001). Each value for the WR was not significantly different between subgroups of patients who were receiving antihypertensive agents and those patients who were not receiving antihypertensive agents. This decrease in WR did not change in the subgroup of patients who were taking antihypertensive agents. Although the WR in 18 patients with diabetes before treatment had a tendency to be greater than the WR in 30 patients without diabetes 637.9 [+ or -] 12.7% vs 31.1 [+ or -] 7.5%, respectively; p = 0.058), the WR in patients with diabetes also significantly decreased to 31.3 [+ or -] 14.7% alter 1 month of nCPAP treatment (p = 0.011), which was sot significantly different from the WR in patients without diabetes (25.6 [+ or -] 7.5%; p = 0.31).
Before treatment, the WR of MIBG in OSAHS patients significantly correlated with the AHI (r = 0.40; p = 0.006) [Fig 3] and the Sa[O.sub.2] < 90% time (r = 0.35; p = 0.016). However, the QTcD during sleep before treatment did not correlate with the WB before treatment (r = 0.17; p = 0.23) [Fig 4]. In 18 OSAHS patients with diabetes, the QTcD during sleep before treatment did not correlate with the WR before treatment (r = 0.14; p = 0.56). In 22 OSAHS patients who neither had diabetes nor received antihypertensive agents, the QTcD during sleep before treatment also did not correlate with the WR before treatment (r = 0.01; p = 0.98). However, in 16 OSAHS patients receiving antihypertensive agents, the QTcD during sleep before treatment was significantly correlated with the WR before treatment (r = 0.51; p = 0.048).
[FIGURES 3-4 OMITTED]
DISCUSSION
The present study suggests that, even in the absence of overt cardiac disease including arrhythmia, OSAHS causes transient nocturnal myocardial electrical instability, which is indicated by an increased QTcD. Previously, the QTcD between 11:00 PM and 1:00 AM was reported to be smaller than the QTcD in either the morning or afternoon. (14) However, in OSAHS patients before treatment, the QTcD during sleep was greater than the QTcD before sleep. Meanwhile, in OSAHS patients with 1 night of nCPAP treatment, the QTcD during sleep was smaller than the QTcD before sleep. Therefore, 1 night of nCPAP treatment normalized the abnormal increase of nocturnal QTcD.
QT dispersion or QTcD is related to sudden death mortality in patients with heart failure (15) and after myocardial infarction. (16) Large prospective studies (7,17) have reported on the relationship between QTcD and mortality. The Rotterdam study (7) demonstrated that in the general elderly population those with a QTcD in the highest tertile (ie, > 60 ms), relative to those in the lowest tertile, had a significantly increased risk for cardiac death, sudden cardiac death, and all-cause death. Since OSAHS patients often have cardiovascular diseases, (10) even at transient nocturnal increase in the QTcD may be a risk factor for cardiovascular mortality. Cardiac arrhythmias during sleep were reported to occur commonly in OSAHS patients. (18) However, other studies have reported (19) that the prevalence of serious arrhythmias and conduction disturbances during sleep is not related to OSAHS. The investigation of nocturnal QTcD in OSAHS patients may contribute to understanding the effect of OSAHS on cardiac arrhythmia and cardiovascular mortality.
In the present study, the AHI and the severity of apnea-hypopnea-related hypoxemia had a significant effect on the QTcD during sleep in OSAHS patients. QTcD is increased not only by acute myocardial ischemia in patients with coronary artery disease, (20) but also by blood gas derangement, including hypoxemia and hypercapnia, in healthy subjects (9) and by respiratory failure from COPD. (8) OSAIIS patients in the present study did not have overt coronary artery disease and did not show ST-T changes throughout the present study. These data suggest that at least one of the mechanisms of decreasing QTcD during sleep may be an improvement in blood gas derangement with nCPAP treatment. Therefore, nCPAP therapy for OSAHS patients is indicated with respect to the QTcD, because an increased QTcD is a strong and independent risk factor for cardiac mortality. (7)
MIBG imaging showed that the WR in OSAHS patients significantly decreased after 1 month of nCPAP treatment, which is consistent with the results of our previous report. (11) This result suggests that nCPAP treatment may reduce the increased cardiac sympathetic activity in OSAHS patients. (11) The activation of sympathetic tone increases QTcD, as shown by studies in healthy subjects using inhaled [beta]-agonist agents, (9) and heart rate variability. (21) In the present study, both the QTcD during sleep and the WR of MIBG were correlated with the indexes of OSAHS severity before treatment, and were improved with nCPAP treatment. However, the correlation coefficients between the QTcD during sleep and the indexes of OSAHS severity, as well as the relationships between the WR of MIBG and the indexes of OSAHS severity, were not robust. In addition, the QTcD did not correlate with the WR of MIBG in all OSAHS patients, in OSAHS patients with diabetes, and in OSAHS patients who neither had diabetes nor received antihypertensive agents. Meanwhile, there was a significant correlation between the QTcD during sleep and the WR of MIBG before treatment in hypertensive OSAHS patients receiving antihypertensive agents. Since hypertension is correlated with sympathetic nerve function, there may be a significant correlation between the QTcD and the WR of MIBG in hypertensive OSAHS patients.
The relationship between QTcD and cardiac sympathetic activity assessed by MIBG cardiac imaging is controversial. Some studies have suggested different mechanisms in patients with hypertrophic cardiomyopathy, (22) or autonomic dysfunction in patients with non-insulin-dependent diabetes mellitus, (23) or insulin-dependent diabetes mellitus. (24) The present study suggests that the QTcD in OSAHS patients may be mediated, not only by hypoxemia-related cardiac sympathetic strain, but also by other factors. We speculate that other factors increasing the QTcD during sleep may be C[O.sub.2] retension, (8) change in parasympathetic nerve activity, (21,22) distention of the right ventricle by an acute increase in pulmonary artery pressure, and fluctuating intrathoracic pressure, which induces myocardial wall stress, cardiac distortion, and changes iii venous return. Some studies have reported that maximum inspiration and maximum expiration decrease QT dispersion or QTcD in healthy subjects," (25) but those investigators have not revealed the mechanism responsible for their results. In the present study, before sleep and after sleep, there was no difference between the QTcD of the untreated OSAHS patients and the QTcD of the OSAHS patients during nCPAP treatment. Consequently, the QTcD of the OSAHS patients during sleep was not influenced by changes in lung volume with nCPAP treatment. Further investigation is needed to elucidate the relationship between our present results and possible factors other than cardiac sympathetic activity and hypoxemia.
Some studies (26) have revealed that OSAHS is independently associated with insulin resistance. In fact, we have previously reported that 1 night of nCPAP treatment improves insulin activity for glucose in OSAHS patients. (27) Because QTcD in healthy subjects is increased by hyperinsulinemia, (28) the diet and medical regimen of diabetic patients was kept uniform for the study period. Therefore, glycemic control was kept the same throughout the study, except for the nCPAP treatment. Consequently, one could speculate that, after the first night of nCPAP treatment, the improvement of insulin resistance during the night might contribute to the decrease in QTcD.
Although various pharmacologic agents can affect the QTcD29 and the WR of MIBG, (30,31) the OSAHS patients in this study received the same medical regimen, including antihypertensive agents (16 patients) and oral drugs for diabetes (3 patients), beginning > 1 month before the start of this study and throughout the study. Therefore, we assert that receiving these drugs did not affect the changes in the results of the QTcD during sleep and the WR in this study. Diabetes plays a role in cardiac sympathetic activity. (32) Indeed, the WR in the 18 patients with diabetes before treatment in this study had a tendency to be greater than the WR in the 30 patients without diabetes. However, the WR in patients with diabetes significantly decreased after 1 month of nCPAP treatment. Therefore, diabetes might not have a significant effect on the overall results in the present study.
In this study, there were no significant differences in QT dispersion and QTcD between OSAHS and the healthy control subjects before and after sleep. The OSAHS patients in this study had no overt cardiac disease and no apnea or hypoxemia during the waking periods. Therefore, there would be no significant differences in the QT dispersion and QTcD in the morning between OSAHS patients and healthy control subjects in this study. However, further study is necessary to ascertain whether, in OSAHS patients whose conditions were complicated by cardiac diseases, nCPAP treatment changes the QTcD during waking periods. One of the limitations in the present study was the significant difference in the BMI between the OSAHS patients and the control subjects. However, there was not significant correlation between the BMI and the QTcD in either the treated patients or the control subjects. Therefore, the BMI would not have significant effects on the morning QTcD.
In conclusion, OSAHS results in an increased nocturnal QTcD, which is a strong risk factor for cardiac mortality. The increased nocturnal QTcD may be improved with nCPAP therapy, independently of cardiac sympathetic function.
ACKNOWLEDGMENT: We thank Kouichi Shimizu, MD, PhD, for patient management. We thank Tomoko Toki and Yoko Kuroki for preparation of the report.
REFERENCES
(1) Partinen M, Jamieson A, Guilleminault C. Long-term outcome for obstructive sleep apnea syndrome patients: morality. Chest 1988; 94:1200-1204
(2) He J, Kryger MH, Zorick FJ, et al. Mortality and apnea index in obstructive sleep apnea: experience in 385 male patients. Chest 1988; 94:9-14
(3) Nieto FJ, Young TB, Lind BK, et al. Association of sleep-disordered breathing, sleep apnea, and hypertension in a large community-based study: Sleep Heart Health Study. JAMA 2000; 283:1829-1836
(4) Peppard PE, Young T, Palta M, et al. Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med 2000; 342:1378-1384
(5) Shahar E, Whitney CW, Redline S, et al. Sleep-disordered breathing and cardiovascular disease: cross-sectional results of the Sleep Heart Health Study. Am J Respir Crit Care Med 2001; 16,3:19-25
(6) Malik M, Batchvarov VN. Measurement, interpretation and clinical potential of QT dispersion. J Am Coll Cardiol 2000; 36:1749-1766
(7) de Bruyne MC, Hoes AW, Kors JA, et al. QTc dispersion predicts cardiac mortality in the elderly: the Rotterdam Study. Circulation 1998; 97:467-472
(8) Sarubbi B, Esposito V, Ducceschi V, et al. Effect of blood gas derangement on QTc dispersion in severe chronic obstructive pulmonary disease: evidence of an electropathy? Int J Cardiol 1997; 58:287-292
(9) Kiely DG, Cargill RI, Grove A, et al. Abnormal myocardial repolarisation in response to hypoxemia and fenoterol. Thorax 1995; 50:1062-1066
(10) Strohl KP, Redline S. Recognition of obstructive sleep apnea. Am J Respir Crit Care Med 1996; 154:279-289
(11) Otsuka N, Ohi M, Chin K, et al. Assessment of cardiac sympathetic function with iodine-123-MIBG imaging in obstructive sleep apnea syndrome. J Nucl Med 1997; 38:567-572
(12) Noguchi T, Chin K, Ohi M, et al. Heat shock protein 72 level decreases during sleep in patients with obstructive sleep apnea syndrome. Am J Respir Crit Carc Med 1997; 155: 1316-1322
(13) Rechtschaffen A, Kales A, eds. A manual of standardized terminology, techniques and scoring system for sleep stages of human subjects. Washington, DC: National Institutes of Health, 1968
(14) Yetkin E, Yanik A, Kutlu M, et al. Changes in QT dispersion magnitude during respiratory phases: role of maximum inspiration and expiration. Angiology 1999; 50:91-917
(15) Anastasiou-Nana MI, Nauas JN, Karagounis LA, et al. Relation of dispersion of QRS and QT in patients with advanced congestive heart failure to cardiac and sudden death mortality. Am J Cardiol 2000; 85:1212-1217
(16) Glancy JM, Garratt CJ, Woods KL, et al. QT dispersion and mortality after myocardial infarction. Lancet 1995; 345:945-948
(17) Okin PM, Devereux RB, Howard BV, et al. Assessment of QT interval and QT dispersion for prediction of all-cause and cardiovascular mortality in American Indians: the Strong Heart Study. Circulation 2000; 101:61-66
(18) Guilleminanlt C, Connolly SJ, Winkle RA. Cardiac arrhythmia and conduction disturbances during sleep in 400 patients with sleep apnea syndrome. Am J Cardiol 1983; 52:490-494
(19) Flemons WW, Remmers JE, Gillis AM. Sleep apnea and cardiac arrhythmias: is there a relationship? Am Rev Respir Dis 1993; 148:618-621
(20) Sporton SC, Taggart P, Sutton PM, et al. Acute ischaemia: a dynamic influence on QT dispersion. Lancet 1997; 349:306-309
(21) Ishida S, Nakagawa M, Fujino T, et nl. Circadian variation of QT interval dispersion: correlation with heart rate variability. J Electrocardiol 1997; 30:205-210
(22) Shimizu M, Ino H, Okeie K, et al. Increased QT dispersion does not reflect the increased regional variation of cardiac sympathetic nervous activity in hypertrophic cardiomyopathy. Am Heart J 200i; 142:358-362
(23) Wei K, Dorian P, Newman D, et al. Association between QT dispersion and autonomic dysfunction in patients with diabetes mellitus. J Am Coll Cardiol 1995; 26:859-863
(24) Langen KJ, Ziegler D, Weise E, et al. Evaluation of QT interval length, QT dispersion and myocardial m-iodobenzylguanidine uptake in insulin-dependent diabetic patients with and without autonomic neuropathy. Clin Sci (Lond) 1997; 93:325-333
(25) Krupienicz A, Czarnecki R, Adamus J. QT dispersion magnitude is related to the respiratory phase in healthy subjects. Am J Cardiol 1997; 80:1232-1234
(26) Ip MSM, Lain B, Ng MMT, et al. Obstructive sleep apnea is independently associated with insulin resistance. Am J Respir Crit Care Med 2002; 165:670-676
(27) Shimizu K, Chin K, Nakamura T, et al. Plasma leptin levels and cardiac sympathetic: function in patients with obstructive sleep apnea-hypopnea syndrome. Thorax 2002; 57:429-434
(28) Watanabe T. Association of insulin with QTc dispersion. Lancet 1997; 350:1821-1822
(29) Bonnar CE, Davie AP, Caruana L, et al. QT dispersion in patients with chronic heart failure: beta blockers are associated with a reduction in QT dispersion. Heart 1999; 81:297-302
(30) Sakata K, Shirotani M, Yoshida H, et al. Effects of amlodipine and cilnidipine on cardiac sympathetic nervous system and neurohormonal status in essential hypertension. Hypertension 1999; 33:1447-1452
(31) Takeishi Y, Atsumi H, Fujiwara S, et al. ACE inhibition reduces cardiac iodine-123-MIBG release in heart failure. J Nucl Med 1997; 38:1085-1089
(32) Schnell O, Hammer K, Muhr-Becker D, et al. Cardiac sympathetic dysinnervation in type 2 diabetes mellitus with and without ECG-based cardiac autonomic neuropathy. J Diabetes Complications 2002; 16:220-227
* From the Departments of Respiratory Medicine (Drs. Nakamura, Takahashi, Sumi, and Mishima) and Cardiovascular Medicine (Dr. Hosokawa), Graduate School of Medicine, and the Department of Physical Therapeutics (Dr. Chin), Kyoto University Hospital, Kyoto University, Kyoto, Japan; and Osaka Kaisei Hospital (Dr. Ohi), Osaka, Japan.
This work was supported in part by grants from the Japanese Ministry of Education, Culture, Sports, Science and Technology; the Japanese Ministry of Health, Labor and Welfare; and the Kato Memorial Trust for Nambyo Research.
Manuscript received July 30, 2003; revision accepted January 9, 2004.
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (e-mail: permissions@chestnet.org).
Correspondence to: Kazuo Chin, MD, PhD, Department of Physical Therapeutics, Kyoto University Hospital, 54 Shogoin Kawahara-cho, Sakyo-ku, Kyoto 606-8507, Japan; e-mail: chink@kuhp.kyoto-u.ac.jp
COPYRIGHT 2004 American College of Chest Physicians
COPYRIGHT 2004 Gale Group