The American College of Chest Physicians (ACCP) recently issued a clinical position statement on outpatient management of community-acquired pneumonia (CAP). "Management of Community-Acquired Pneumonia in the Home" was published in the May 2005 issue of Chest and can be accessed online at http://www.chestjournal. org/cgi/content/full/127/5/1752.
Pneumonia is the most common cause of death from infectious disease, and CAP affects up to 3 million persons in the United States each year. The number of patients being treated in their homes for CAP is increasing because of cost considerations, patient preference, and the availability of effective oral antibiotics.
The ACCP Home Care Network Working Group concluded that the current evidence is insufficient to support an evidence-based practice guideline on outpatient treatment of CAP, but because of the importance of the issue, the working group developed a clinical position statement. The ACCP statement seeks to address the requirements of treating patients with CAP at home while providing the same level of care, recovery, and functional status that is available at an inpatient facility.
Diagnosing CAP in Outpatients
The diagnosis of CAP should be made by a qualified health care professional and based on clinical history and classic symptoms (e.g., new-onset cough, sputum production or shortness of breath, fever, rales). Older or immunocompromised patients should be monitored closely for CAP. Chest radiography should be performed on patients who have a goal of complete recovery (as opposed to patients who are receiving palliative care) to confirm the diagnosis of CAP, assess its severity, and establish a baseline for confirming the resolution of the disease. Physicians also should consider other tests to guide treatment, including a chemistry panel evaluation, hemoglobin/hematocrit determination, and blood cultures.
Choosing the Site of Care
According to the statement, the decision to treat a patient on an outpatient basis as opposed to in the hospital should be based on the severity of the illness, the ability of the patient or caregiver to manage the treatment, and the patient's wishes. Patients who live alone or have abnormal vital signs, mental instability, alcoholism, chronic obstructive pulmonary disease, aspiration, cardiovascular instability, uremia, or malnutrition, and those who have been hospitalized for pneumonia in the past year have a poor prognosis for in-home treatment. A respiratory rate of more than 30 breaths per minute, hypotension, a temperature of more than 38.3[degrees]C (101.0[degrees]F), extrapulmonary infection, confusion, and decreased consciousness are also risk factors for poor outcome of outpatient care. Whether to treat CAP in the home or in a health care facility ultimately must be a joint decision between the physician and patient.
Outpatients who are diagnosed with CAP should be transferred to an acute care facility if they meet at least one of the following criteria: (1) the need for aggressive medical or surgical intervention is urgent, (2) critical diagnostic tests are not available in the home, (3) necessary therapy is not available in the home or is beyond the abilities of the caregiver, (4) patient comfort cannot be ensured in the home, or (5) infection control measures are not possible in the home.
The patient and/or caregiver always should be informed of the risks, benefits, and cost of outpatient care compared with hospitalization.
Treatment Needs of the Outpatient
The ACCP maintains that the physician is responsible for confirming the availability of all aspects of the treatment plan in the patient's home before initiating outpatient treatment. Physicians should evaluate the caregiver's ability to respond to the patient's needs in regard to hydration, nutrition, pain, cough, and shortness of breath. Oral administration of antibiotics is recommended by the ACCP for outpatient treatment, but the choice of antibiotic should be made on a case-by-case basis.
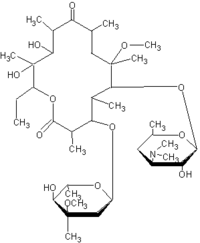
The use of a macrolide antibiotic, doxycycline (Vibramycin), or fluoroquinolone agent may be appropriate empiric outpatient treatment for low-risk patients (i.e., young, otherwise healthy persons). Alternatives to these agents in low-risk patients are amoxicillin-clavulanate (Augmentin) and some second-generation cephalosporins (e.g., cefuroxime [Ceftin], cefpodoxime [Vantin], cefprozil [Cefzil]).
A lack of response to treatment with macrolides and fluoroquinolones has been reported. Some experts prefer to reserve the use of fluoroquinolones for older patients, patients who are allergic to or intolerant of macrolides, patients who have received recent macrolide treatment, patients with comorbidities, patients with documented infections with highly resistant pneumococci, or patients with a lack of response to treatment with another agent. There have been reports of a lack of response to outpatient therapy with azithromycin (Zithromax) and clarithromycin (Biaxin) as the primary treatment for CAP.
Patients who are at high risk because of complicated comorbidities or extensive prior antibiotic use may be a candidate for treatment with a beta lactam-macrolide combination or a antipneumococcal fluoroquinolone. Double therapy with a beta lactam-macrolide combination or a beta lactam-antipneumococcal fluoroquinolone should be considered in patients who normally would be considered for admission to an intensive care unit but have chosen to be treated on an outpatient basis.
Table 1 lists the pathogens and factors that increase a patient's risk of infection. Because of increasing resistance of Streptococcus pneumoniae to antimicrobial drugs, physicians should monitor patients after initiation of antibiotic therapy. The first dose of antibiotics should be administered within four hours of presentation, if possible. Mortality rates have been shown to increase in hospitalized patients with CAP who do not receive antibiotics within eight hours of presentation.
The ACCP recommends that patients who wish to have outpatient care and their physicians and caregivers have a written care plan that outlines the risks and benefits of outpatient care. it should be made clear that hospitalization is not without risk. Hospitalized patients are at increased risk for deconditioning, pressure ulcers, infection by drug-resistant organisms, and translocation trauma. The care plan is not a legal document, but it serves as an educational tool. The care plan should include a plan for transfer to an inpatient facility should the patient fail to respond to outpatient treatment.
Monitoring Outpatients with CAP
After the initial evaluation, all patients with CAP should have a follow-up assessment. Patients who are considered to be high risk should be assessed 24 hours after the initial diagnosis. At every follow-up visit the health care professional should observe vital signs, cardiopulmonary symptoms, mental status, nutrition and hydration status, urinary frequency and output, skin integrity and turgor, lower extremity symptoms, mobility, the use of assistive devices, psychosocial status, and medication compliance. The health care professional should document the patient's achievement of the following goals:
* Understanding of pneumonia
* recognizing worsening symptoms and knowing what to do if they occur
* Making and keeping medical appointments
* Adapting the lifestyle to control and recover from symptoms
* Monitoring body temperature and sputum production
* Understanding and complying with the medication and diet regimens
* Understanding the proper use and care of respiratory equipment
* Following the care plan to maintain vital signs within established parameters
* Maintaining the activity level prescribed by the physician
* Maintaining a smoke-free environment
Resolution of Symptoms
The physician should confirm resolution of symptoms with chest radiography and evaluate the patient's status eight weeks after the diagnosis of CAP. The patient should be made aware of preventive measures for the future, including smoking cessation, influenza vaccination, initial pneumococcal vaccination, and revaccination with the pneumococcal vaccine every five to seven years if appropriate.
COPYRIGHT 2005 American Academy of Family Physicians
COPYRIGHT 2005 Gale Group