Definition
Leptospirosis is a febrile disease (fever) caused by infection with the bacteria Leptospira interrogans. The disease can range from very mild and symptomless to a more serious, even life threatening form, that may be associated with kidney (renal) failure.
Description
An infection by the bacterium Leptospira interrogans goes by different names in different regions. Alternate names for leptospirosis include mud fever, swamp fever, sugar cane fever, and Fort Bragg fever. More severe cases of leptospirosis are called Weil's syndrome or icterohemorrhagic fever. This disease is commonly found in tropical and subtropical climates but occurs worldwide.
As of the mid 1980s, there were 35-60 cases of leptospirosis reported in the United States each year. Most cases occur in Hawaii, followed by the south Atlantic, Gulf, and Pacific coastal states. However, because of the nonspecific symptoms of leptospirosis, it is believed that the occurrence in the United States is actually much higher. Leptospirosis occurs year-round in the United States, but about half of the cases occur between July and October.
Leptospirosis is a disease of animals and can be a very serious problem in the livestock industry. Leptospira bacteria have been found in dogs, rats, livestock, mice, voles, rabbits, hedgehogs, skunks, possums, frogs, fish, snakes, and certain birds and insects. Infected animals will pass the bacteria in their urine for months, or even years. In the United States, rats and dogs are more commonly linked with human leptospirosis than other animals.
Humans are considered "accidental hosts" and become infected with Leptospira interrogans by coming into contact with urine from infected animals. This is either through direct contact with urine, or through contact with soil, water, or plants that have been contaminated by animal urine. Leptospira interrogans can survive for as long as six months outdoors under favorable conditions. Leptospira bacteria can enter the body through cuts or other skin damage or through mucous membranes (such as the inside of the mouth and nose). It is believed that the bacteria may be able to pass through intact skin, but this is not known.
Once past the skin barrier, the bacteria enter the blood stream and rapidly spread throughout the body. The infection causes damage to the inner lining of blood vessels. The liver, kidneys, heart, lungs, central nervous system, and eyes may be affected.
There are two stages in the disease process. The first stage is during the active Leptospira infection and is called the "bacteremic," or "septicemic," phase. The bacteremic phase lasts from three to seven days and presents as typical flu-like symptoms. During this phase, bacteria can be found in the patient's blood and cerebrospinal fluid. The second stage, or "immune phase," occurs either immediately after the bacteremic stage or after a 1-3 day symptom-free period. The immune phase can last up to one month. During the immune phase, symptoms are milder but meningitis (inflammation of spinal cord and brain tissues) is common. Bacteria can be isolated only from the urine during this second phase.
Causes & symptoms
Leptospirosis is caused by an infection with the bacterium Leptospira interrogans. The bacteria are spread through contact with urine from infected animals. Persons at an increased risk for leptospirosis include farmers, miners, animal health care workers, fish farmers and processors, sewage and canal workers, cane harvesters, and soldiers. High risk activities include care of pets, hunting, trail biking, freshwater swimming, rafting, canoeing, kayaking, and participating in sports in muddy fields.
Symptoms of Leptospira infection occur within 7-12 days following exposure to the bacteria. Because the symptoms can be nonspecific, most people who have antibodies to Leptospira do not remember having had an illness. Eighty-five to 90% of the cases are not serious and clear up on their own. Symptoms of the first stage of leptospirosis last three to seven days and are: fever (100-105°F [37.8-40.6°C]), severe headache, muscle pain, stomach pain, chills, nausea, vomiting, back pain, joint pain, neck stiffness, and extreme exhaustion. Cough and body rash sometimes occur.
Following the first stage of disease, a brief symptom-free period occurs for most patients. The symptoms of the second stage vary in each patient. Most patients have a low grade fever, headache, vomiting, and rash. Aseptic meningitis is common in the second stage, symptoms of which include headache and photosensitivity (sensitivity of the eye to light). Leptospira can affect the eyes and make them cloudy and yellow to orange colored. Vision may be blurred.
Ten percent of the persons infected with Leptospira develop a serious disease called Weil's syndrome. The symptoms of Weil's syndrome are more severe than those described above and there is no distinction between the first and second stages of disease. The hallmark of Weil's syndrome is liver, kidney, and blood vessel disease. The signs of severe disease are apparent after 3-7 days of illness. In addition to those listed above, symptoms of Weil's syndrome include jaundice (yellow skin and eyes), decreased or no urine output, hypotension (low blood pressure), rash, anemia (decreased number of red blood cells), shock, and severe mental status changes. Red spots on the skin, "blood shot" eyes, and bloody sputum signal that blood vessel damage and hemorrhage have occurred.
Diagnosis
Leptospirosis can be diagnosed and treated by doctors who specialize in infectious diseases. During the bacteremic phase of the disease, the symptoms are relatively nonspecific. This often causes an initial misdiagnosis because many diseases have similar symptoms to leptospirosis. The later symptoms of jaundice and kidney failure together with the bacteremic phase symptoms suggest leptospirosis. Blood samples will be tested to look for antibodies to Leptospira interrogans. Blood samples taken over a period of a few days would show an increase in the number of antibodies. Isolating Leptospira bacteria from blood, cerebrospinal fluid (performed by spinal tap), and urine samples is diagnostic of leptospirosis. It make take six weeks for Leptospira to grow in laboratory media. Most insurance companies would cover the diagnosis and treatment of this infection.
Treatment
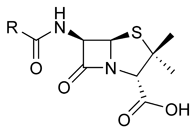
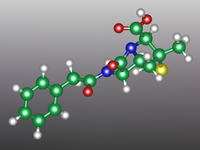
Leptospirosis is treated with antibiotics, penicillin (Bicillin, Wycillin), doxycycline (Monodox), ibramycin, or erythromycin (E-mycin, Ery-Tab). As of early 1998, the timing of antibiotic treatment is controversial. It is generally agreed that antibiotic treatment during the first few days of illness is helpful. However, leptospirosis is often not diagnosed until the later stages of illness. The benefit of antibiotic treatment in the later stages of disease is controversial. A rare complication of antibiotic therapy for leptospirosis is the occurrence of the Jarisch-Herxheimer reaction, which is characterized by fever, chills, headache, and muscle pain.
Patients with severe illness will require hospitalization for treatment and monitoring. Medication or other treatment for pain, fever, vomiting, fluid loss, bleeding, mental changes, and low blood pressure may be provided. Patients with kidney failure will require hemodialysis to remove waste products from the blood.
Prognosis
The majority of patients infected with Leptospira interrogans experience a complete recovery. Ten percent of the patients will develop eye inflammation (uveitis) up to one year after the illness. In the United States, about one out of every 100 patients will die from leptospirosis. Death is usually caused by kidney failure, but has also been caused by myocarditis (inflammation of heart tissue), septic shock (reduced blood flow to the organs because of the bacterial infection), organ failure, and/or poorly functioning lungs.
Prevention
Persons who are at an extremely high risk (such as soldiers who are training in wetlands) can be pretreated with 200 mg of doxycycline once a week. As of early 1998, there were no vaccines available to prevent leptospirosis.
There are many ways to decrease the chances of being infected by Leptospira. These include:
- Avoid swimming or wading in freshwater ponds and slowly moving streams, especially those located near farms.
- Do not conduct canoe or kayak capsizing drills in freshwater ponds. Use a swimming pool instead.
- Boil or chemically treat pond or stream water before drinking it or cooking with it.
- Control rats and mice around the home.
- Have pets and farm animals vaccinated against Leptospira.
- Wear protective clothing (gloves, boots, long pants, and long-sleeved shirts) when working with wet soil or plants.
Key Terms
- Hemodialysis
- The removal of waste products from the blood stream in patients with kidney failure. Blood is removed from a vein, passed through a dialysis machine, and then put back into a vein.
- Jarisch-Herxheimer reaction
- A rare reaction to the dead bacteria in the blood stream following antibiotic treatment.
- Meningitis
- Inflammation of tissues in the brain and spinal cord. Aseptic meningitis refers to meningitis with no bacteria present in the cerebral spinal fluid.
Gale Encyclopedia of Medicine. Gale Research, 1999.