Definition
A bacterial infection of the skin which causes red to bluish-black colored spots.
Description
Pinta is a skin infection caused by the bacterium Treponema carateum, a relative of the bacterium which causes syphilis. The word "pinta" comes from the Spanish and means "painted." Pinta is also known as "azula" (blue), and "mal de pinto" (pinto sickness). It is one of several infections caused by different Treponema bacteria, which are called "endemic" or "non-venereal" treponematoses.
Pinta is primarily found in rural, poverty-stricken areas of northern South America, Mexico, and the Caribbean. The disease is usually acquired during childhood and is spread from one person to another by direct skin-to-skin contact. The bacteria enter the skin through a small cut, scratch, or other skin damage. Once inside the skin, the warmth and moisture allow the bacteria to multiply. The bacterial infection causes red, scaly lesions on the skin.
Causes & symptoms
Pinta is caused by an infection with the bacterium Treponema carateum. Persons at risk for pinta are those who live in rural, poverty-stricken, overcrowded regions of South America, Mexico, and the Caribbean. Symptoms of pinta occur within two to four weeks after exposure to the bacteria. The first sign of infection is a red, scaly, slowly enlarging bump on the skin. This is called the "primary lesion." The primary lesion usually appears at the site where the bacteria entered the skin. This is often on the arms, legs, or face. The smaller lesions which form around the primary lesion are called "satellite lesions." Lymph nodes located near the infected area will become enlarged, but are painless.
The second stage of pinta occurs between one and 12 months after the primary lesion stage. Many flat, red, scaly, itchy lesions called "pintids" occur either near the primary lesion, or scattered around the body. Pintid lesions progress through a range of color changes, from red to bluish-black. The skin of older lesions will become depigmented (loss of normal color).
Diagnosis
Pinta can be diagnosed by dermatologists (doctors who specialize in skin diseases) and infectious disease specialists. The appearance of the lesions helps in the diagnosis. A blood sample will be taken from the patient's arm to test for antibodies to Treponema carateum. A scraping of a lesion will be examined under the microscope to look for Treponema bacteria. The results of these tests should be available within one to two days.
Treatment
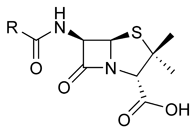
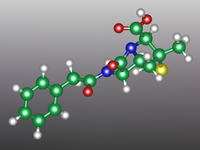
Pinta is treated with benzathine penicillin G (Bicillin), given as a single injection.
Prognosis
Treatment will result in a complete cure but will not undo any skin damage caused by the late stages of disease. Spread of pinta to the eyes can cause eyelid deformities.
Prevention
Good personal hygiene and general health may help prevent infections. In general, avoid physical contact with persons who have skin lesions.
Key Terms
- Lesion
- An abnormal change in skin due to disease.
Further Reading
For Your Information
Other
- Mayo Health Oasis. 1998. http://www.mayohealth.org (5 March 1998).
Gale Encyclopedia of Medicine. Gale Research, 1999.