Aberrant vascular remodeling is a central hallmark for the development and progression of idiopathic pulmonary fibrosis. The mechanisms underlying the pathophysiologic alterations, however, are poorly understood. A recent phase II trial of interferon γ-1b has demonstrated a trend toward a decrease in profibrotic and proangiogenic biologic markers, and upregulation of lung CXCL11 mRNA and bronchoalveolar lavage fluid and plasma protein levels of CXCL11. We hypothesized that net aberrant vascular remodeling seen during the pathogenesis of fibroplasia and deposition of extracellular matrix during bleomycin-induced pulmonary fibrosis can be attenuated by treatment with the angiostatic ELR^sup -^ CXC chemokine, CXCL11. In a preclinical model, systemic administration of CXCL11 reduced pulmonary collagen deposition, procollagen gene expression, and histopathologic fibroplasia and extracellular matrix deposition in the lung of bleomycin-treated mice. CXCL11 treatment significantly reduced bleomycin-induced pulmonary fibrosis without altering specific lung leukocyte populations. CXCR3 is not expressed on fibroblasts and CXCL11 had no direct functional effect on pulmonary fibroblasts. The angiogenic activity in the lung was significantly decreased, however, and CXCL11 treatment reduced the total number of endothelial cells in the lung following bleomycin exposure. The results suggest that CXCL11 inhibits pulmonary fibrosis by altering aberrant vascular remodeling.
Keywords: angiogenesis; chemokines; fibrosis
Idiopathic pulmonary fibrosis (IPF) is a chronic and often fatal pulmonary disorder. A prevalence rate of 27 to 29 cases per 100,000 for the disease has been reported, and it may even be as high as 150 cases per 100,000 in individuals greater than 75 years of age (1). The incidence of IPF seems to be on the rise in certain parts of the world, such as the United Kingdom, New Zealand, and Germany (2). No effective treatment exists for IPF, with a 2- to 3-year median survival of 50%. Patients with IPF treated with interferon (IFN)-γ-1b showed an improvement in lung function, including an increase in total lung capacity and partial pressure of oxygen at rest and exertion (3). A recent phase III clinical trial demonstrated that there was a trend toward survival in the intent-to-treat group of patients with IPF treated with IFN-γ-1b (4). Further subgroup analysis of patients with FVC greater than or equal to 55% and diffusing capacity of lung for carbon monoxide greater than or equal to 35% in this trial demonstrated a significant relative reduction in risk of death (4). The mechanism, however, for the potential survival advantage in the IFN-γ-treated patients remains to be determined. In a phase II study of biomarker expression in IPF-treated patients, patients with IPF treated with IFN-γ-1b had a reduction in the synthesis of profibrotic molecules, such as elastin, procollagen type I and III, and platelet-derived growth factors (PDGF), and a decrease in the proangiogenic factor CXCL5 (5). These findings occurred in the context of a marked upregulation of bronchoalveolar lavage and plasma CXCL11 (IFN-inducible T cell α chemoattractant), but not CXCL9 (monokine induced by IFN-γ), or CXCLlO (IFN-γ-inducible protein) (5). Furthermore, these findings were paralleled by a statistically significant increase in lung gene expression of CXCL11, but not CXCL9 or CXCLlO (5). The mechanism regarding the effects of CXCL11 on the pathogenesis of pulmonary fibrosis remains to be elucidated.
Our laboratory has shown that members of the CXC chemokine family exert disparate effects in regulating angiogenesis, relevant to vascular remodeling (6). CXC chemokines that contain glutamic acid-leucine-arginine (ELR motif) in the NH2-terminus promote angiogenesis, whereas type I and II IFN-inducible CXC chemokines and PF4 inhibit angiogenesis (6, 7). ELR^sup +^ chemokines seem to be involved in the pathogenesis of a variety of disease processes, such as pulmonary fibrosis, rheumatoid arthritis, coronary artery disease, cancer, and acute lung injury, in which aberrant vascular remodeling has been shown to promote the pathogenesis of these disorders (8-17). The IFN-inducible CXC chemokines have been shown to inhibit angiogenesis and endothelial cell chemotaxis by CXCR3 (18, 19). Recently, it has been shown that there are two human isoforms of CXCR3: CXCR3A, which is expressed on T cells, B cells, and natural killer cells; and CXCR3B, which is expressed on endothelial cells, mediating the angiostatic activity of these CXC chemokines (20, 21). The existence of CXCR3 splice variants in mouse has not been found.
After recent reports for the potential of improved survival in patients with IPF treated with IFN-γ-1b (4), and a biomarker study that demonstrated the IFN-γ induces the gene expression and protein production of CXCL11 in the lung and plasma (5), we hypothesized that systemic administration of the IFN-inducible chemokine CXCL11 may have a protective role during bleomycininduced pulmonary fibrosis by decreasing pathologic aberrant vascular remodeling. Mice systemically treated with CXCL11 and exposed to bleomycin demonstrated a significant reduction in total lung collagen and procollagen type I gene expression in the lungs, in comparison with mice exposed to bleomycin alone. CXCL11 had no effect, however, on the functional responses of fibroblasts in vitro. The decrease in fibrosis correlated with a significant decrease in the angiogenic activity of the bleomycin-exposed lung and a reduction in the number of endothelial cells in the lung. The protective effect exerted by CXCL11 treatment was mediated through CXCR3, because blocking this receptor restored the bleomycin-induced increase in lung collagen. These results suggest that the IFN-inducible CXC chemokine, CXCL11, plays a significant role in modulating vascular remodeling during bleomycin-induced pulmonary fibrosis and may be a therapeutic agent to be considered for use in the treatment of patients with pulmonary fibrosis.
METHODS
A more detailed description of the methods is available in the online supplement.
Reagents
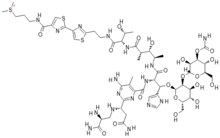
Recombinant CXCL8, CXCL10, CXCL11, PDGF (BB), epidermal growth factor (EOF), and transforming growth factor-β were purchased from R&D Systems (Minneapolis, MN). The antiprolease buffer for tissue homogenization consisted of 1× phosphate-buffered saline with one complete tablet (Bochringer Mannheim, Indianapolis, IN) per 50 ml. The biotinylated antimurine panendothelial cell marker (MECA-32) was purchased from BD Biosciences (San Jose, CA). Murine anti-CXCR3 production and characterization was as previously described (22).
Animal Model of Pulmonary Fibrosis
Bleomycin model of pulmonary fibrosis was performed as previously described (23,24). Bleomycin-treated mice were given daily intramuscular injections of recombinant CXCL11 (2 µg in 0.25% murine serum albumin [MSA]) or MSA (0.25% MSA) until killed. In CXCR3 neutralization experiments, animals received 1 ml of anti-mCXCR3 or normal goat serum on Days 0, 2, 4, 6, 8, and 10 by intraperitoneal injection as previously described (22).
Lung Tissue Preparation for Protein and Corneal Micropocket Angiogenesis Assay Analysis
Bleomycin- or saline (control)-treated lungs were homogenized and sonicated in antiprotease buffer, as previously described (23-26).
Sircol Collagen Assay
The Sircol collagen assay (Biocolor, Belfast, Ireland) was used to measure the soluble forms of collagen present in lung homogenates as previously described (27, 28).
Fibroblast Proliferation
Murine lung fibroblasts were cultured and assessed for proliferation as previously described (23, 24).
Fibroblast Chemotaxis
Murine lung fibroblasts used in chemotaxis assays were cultured as described previously and normal human lung fibroblasts (Cambrex, East Rutherford, NJ) were analyzed for migration using modified 12-well Boyden chambers (Neuroprobe, Gaithersburg, MD) as previously described (6, 27, 29, 30).
Corneal Micropocket Assay of Angiogenesis
Angiogenic activity of lung homogenates was assayed in vivo in the avascular cornea of hooded Long-Evans rat eyes as previously described (11, 23, 24).
Total RNA Isolation and Real-Time Quantitative Polymerase Chain Reaction
Total RNA was isolated with Trizol reagent, according to manufacturer's instructions as previously described (27). Total RNA was determined and 1 µg of total RNA was reverse transcribed into cDNA, and amplified using TaqMan reverse transcription reagents (PE Applied Biosystems, Foster City, CA) as previously described (27). Real-time quantitative polymcrase chain reaction was performed using specific TaqMan primers and probes, the ABI Prism 7,700 sequence detector, and SDS analysis software (PE Applied Biosystems) as previously described (27). Quantitative analysis of gene expression was done using the comparative C^sub T^ (ΔC^sub T^) methods as previously described (27).
Fluorescence-activated Cell Sorter Analysis of Pan-Endothelial Cell Marker and Leukocyte Populations
Single-cell suspensions of lung preparations were made using a method as previously described (23, 24). Single-cell suspensions were stained with the following: primary panendothelial cell Abs (MECA-32) directly conjugated to biotin (PharMingen, San Diego, CA) followed by SA-PE (PharMingen); primary goat anti-murine CXCR3 (Santa Cruz Biotechnology, Santa Cruz, CA) followed by Alexa 488 (FITC anti-goat) (Molecular Probes, Eugene, OR); samples were also stained with tricolor conjugated anti-murine CD45 (Caltag Laboratories, Burlingame, CA) with PE-conjugated CD3, CD4, CD8A, NK1.1, Ly6 (BD Biosciences), or MAC519 (concentration; Serotec, Raleigh, NC). Cells were analyzed on a FACScan flow cytometer (BD Biosciences) using Cellquest software (BD Biosciences).
Histology
Lungs for histology and morphometric analysis were processed and assessed as previously described (27).
Statistical Analysis
Statistical analysis was performed as previously described (27).
RESULTS
CXCL11 Attenuates Bleomycin-induced Pulmonary Fibrosis through CXCR3
Because CXCL11 was found to be the sole IFN-inducible CXC chemokine expressed in patients with IPF treated with IFN-γ (5), we wanted first to determine whether CXCL11 was expressed in the lung during bleomycin-induced pulmonary fibrosis. We found CXCL11 mRNA to be expressed to similar levels as what has been described by Tager and colleagues (31). Next, we determined whether systemically administered CXCL11 mediated an antifibrotic effect in a preclinical model of pulmonary fibrosis. On the basis of the kinetics of collagen deposition in the lung from our previous work, which demonstrated markedly elevated levels of total lung collagen after bleomycin exposure at Days 8 to 16 (23, 24, 27), we next assessed whether treatment of animals exposed to bleomycin with CXCL11, as compared with appropriate controls, inhibited pulmonary fibrosis. CXCL11 (2 µg) or vehicle control was systemically delivered (intramuscularly) every day from 0 to 12 days post-bleomycin exposure. To determine if the potential effect of CXCL11 on bleomycin-induced pulmonary fibrosis was mediated through CXCR3, neutralizing studies were performed where anti-mCXCR3 or control antibodies were administered to mice on Days 0, 2, 4, 6, 8, and 10 after intratracheal bleomycin in the presence or absence of CXCL11 therapy using a modification as previously described (22).
To assess the effect of CXCL11 treatment on pulmonary fibrosis, we first assessed total lung collagen deposition in the lungs of bleomycin-challenged animals in the presence or absence of CXCL11 treatment. Systemic treatment with CXCL11 reduced bleomycin-induced total lung collagen deposition (Figure 1A). This effect was mediated through CXCR3, because blockade of this chemokine receptor inhibited the CXCL11-induced reduction in collagen generation, and reconstituted the expression of procollagen type I mRNA (see Figure 1A; and data not shown). Analysis of lung tissue procollagen type I mRNA by real-time reverse transcriptase-polymerase chain reaction demonstrated a decrease in procollagen type I mRNA in the CXCL11-treated animals, as compared with vehicle controls (Figure 1B). Histopathologic analysis of the lungs from bleomycin-exposed mice demonstrated that the CXCL11-treated animals displayed decreased bleomycin-induced pulmonary fibrosis (Figure 21). This finding was further supported using a quantitative morphometric scoring system of fibrosis (Figure 2II).
Systemic CXCL11 Treatment Does Not Alter the Leukocyte Populations Infiltrating the Lung in Response to Intratracheal Bleomycin
To begin to elucidate a potential mechanism for CXCL11-induced inhibition of bleomycin-mediated pulmonary fibrosis, we next assessed whether systemic CXCL11 treatment affected the elicitation of leukocytes into the lungs of bleomycin-exposed animals. We analyzed single-cell suspensions of lung digests with flow cytometry to determine if the decrease in collagen and histopathologic damage in the CXCL11-treated group was a consequence of altered leukocyte recruitment to the lung. Systemic treatment of animals with CXCL11 during bleomycin-induced pulmonary fibrosis had no significant effect on any of the leukocyte subpopulations infiltrating the lung in response to intratracheal bleomycin (Table 1). There was also no difference in the number of leukocytes expressing the putative CXCL11 receptor, CXCR3, in the lungs of CXCL11 -treated animals when compared with vehicle control (Table 1).
CXCL11 Does Not Affect Pulmonary Fibroblast Proliferation or Procollagen I Gene Expression
One of the hallmarks of pulmonary fibrosis is the proliferation of pulmonary fibroblasts (32, 33). To determine whether CXCL11 attenuated pulmonary fibrosis by a mechanism of inhibition of fibroblast proliferation, we next assessed the effect of CXCL11 on proliferation of primary cultures of murine fibroblasts. Murine pulmonary fibroblasts were isolated from lungs and stimulated in vitro for 72 hours with varying concentrations of CXCL11, or PDGF alone, or CXCL11 combined with PDGF (Figure 3). Stimulation of pulmonary fibroblasts with CXCL11 had no effect on fibroblast proliferation either alone or in the presence of PDGF. Furthermore, CXCL11 did not affect the transforming growth factor-β-induced procollagen I gene expression, 48 hours after in vitro stimulation, as measured by quantitative reverse transcriptase-polymerase chain reaction (data not shown).
CXCL11 Does Not Affect Pulmonary Fibroblast Migration and Fibroblasts Do Not Express CXCR3
Local fibroblast migration from the interstitium into the intraalveolar space is believed to be an important biologic event during the pathogenesis of pulmonary fibrosis (32, 33). To determine whether CXCL11 attenuated pulmonary fibrosis by a mechanism of inhibition of fibroblast migration, we next assessed the effect of CXCL11 on migration of primary cultures of murine and human fibroblasts in a chemotaxis assay in response to PDGF or EGF. Murine pulmonary fibroblasts were isolated from mouse lungs as described previously, or human fibroblasts were used in a chemotaxis assay. Both PDGF (BB; 10 ng/ml) and EGF (1 ng/ml) induced marked chemotactic activity for murine and human fibroblast migration (Figure 4; murine not shown). CXCL11 in a dose response of 1 to 300 ng/ml failed to have an effect alone or in combination with either PDGF or EGF, however, for inhibiting fibroblast migration in the chemotaxis assay (Figure 4; murine not shown). Next we assessed whether CXCL11 (1 to 100 ng/ml) could inhibit murine primary lung fibroblast migration in response to bronchoalveolar lavage fluid from animals exposed to bleomycin at both Days 8 and 16. Although bronchoalveolar lavage fluid from bleomycin-exposed animals induced fibroblast migration, we did not see that CXCL11 inhibited migration (data not shown). To further assess why murine and human fibroblasts did not respond to CXCL11, we next assess expression of CXCR3 mRNA. CXCR3 mRNA from murine and human fibroblasts was processed for analysis by quantitative reverse transcriptase-polymerase chain reaction using TaqMan primer sets. CXCR3 mRNA was not measurable using this strategy (data not shown).
CXCL11-induced Inhibition of Angiogenesis Is CXCR3 Dependent
To ascertain the angiostatic ability of CXCL11 in vivo, recombinant CXCL11 was assayed in the cornea micropocket assay of angiogenesis. CXCL8 and bFGF are both potent inducers of angiogenesis in vivo (six of six corneas positive for both proteins; Figure SIA and 5IIA, respectively). CXCL11 inhibited the angiogenic activity of CXCL8, with only one cornea being positive in the CXCL8 group (one of six; Figure 5IB). Furthermore, CXCL11 also inhibited the bFGF-induced angiogenesis (zero of six corneas positive; Figure 5IIB). The in vivo angiostatic function of CXCL11 occurred through CXCR3, because blocking this receptor restored the angiogenic activity of either CXCL8 (five of six corneas positive; Figure 51C) or bFGF (six of six corneas positive; Figure 5IIC).
CXCL11 Treatment Reduces Aberrant Vascular Remodeling during Bleomycin-induced Pulmonary Fibrosis
Pulmonary fibrosis is associated with aberrant vascular remodeling (8, 11, 23, 24, 34). We have previously demonstrated that inhibition of angiogenesis during bleomycin-induced pulmonary fibrosis results in attenuation of fibrosis (11, 23, 24). On this basis, we next assessed whether systemic CXCL11 treatment inhibited aberrant vascular remodeling during bleomycin-induced pulmonary fibrosis. Lung homogenate samples were isolated 12 days following bleomycin from mice that had been treated with either MSA, CXCL11 plus anti-mCXCR3, or CXCL11 plus normal goat serum (CTRL Ab), and assayed in vivo in the cornea micropocket assay. Lungs from mice treated with CXCL11 demonstrated decreased angiogenic activity (one of six corneas positive; Figure 6IB), when compared with lungs from MSA control animals (six of six corneas positive; Figure 6IA), or from CXCL11 plus anti-mCXCR3-treated mice (six of six corneas positive; Figure 6IC). To substantiate further that CXCL11 attenuated aberrant vascular remodeling in vivo, we performed fluorescence-activated cell sorter (FACS) analysis of lung endothelial cells under similar conditions. Systemic CXCL11 treatment during bleomycin-induced pulmonary fibrosis resulted in marked reduction in the number of endothelial cells in the lung (Figure 6II).
DISCUSSION
Our findings have demonstrated that altering the proangiogenic environment in the lung during bleomycin-induced pulmonary fibrosis with the IFN-inducible CXC chemokine, CXCL11, results in the following: (1) a reduction in total lung collagen and gene expression of procollagen type I; (2) amelioration of the histopathologic fibrosis in the lung; (3) no change in intrapulmonary subpopulations of leukocytes or change in pulmonary fibroblast proliferation, fibroblast gene expression of procollagen, or fibroblast migration in response to PDGF and EGF; and (4) attenuated angiogenic activity and aberrant vascular remodeling in the lung during bleomycin-induced pulmonary fibrosis. Studies directed at understanding the pathogenesis of IPF have primarily focused on mechanisms related to fibroplasia and deposition of extracellular matrix. Multiple disorders associated with fibroproliferative changes are also associated, however, with aberrant vascular remodeling (35). In fact, angiogenesis is a pivotal process necessary for the histopathologic changes that characterize most fibroproliferative disorders. For example, aberrant vascular remodeling has been shown to play a role in pathogenesis of fibrosis associated with acute lung injury and sarcoidosis (13, 36, 37). Turner-Warwick (8) demonstrated the existence of morphologic neovascularization in the lungs of patients with widespread IPF. Furthermore, the contribution of aberrant neovascularization to the pathogenesis of fibrosis in IPF has only recently been appreciated (38-40). Other investigators have also demonstrated the importance of neovascularization in a rat model of bleomycin-induced pulmonary fibrosis by using scanning electron microscopy to demonstrate the close association of neovascularization with pulmonary fibrosis, and the formation of systemic-pulmonary anastomoses (34). Taken together, these findings highlight the association between multiple chronic fibroproliferative disorders and aberrant vascular remodeling.
Previous work from this laboratory has demonstrated that the balance between angiogenic and angiostatic factors is central to the pathogenesis of pulmonary fibrosis (11, 23, 24, 41). We have previously shown that in IPF and during bleomycin-induced pulmonary fibrosis, a proangiogenic environment exists in the lung (11, 23, 24). For example, depletion of CXCL8 or CXCL10 resulted in a marked reduction or enhancement of lung IPF tissue-derived angiogenic activity, respectively (11). Moreover, systemic treatment of mice with CXCL10, after intratracheal bleomycin, inhibited bleomycin-induced pulmonary fibrosis by decreasing angiogenesis (24). Recently, we have demonstrated that the ELR^sup +^ chemokine, CXCL5, is also markedly increased in the lungs of patients with IPF, when compared with patients without pulmonary fibrosis. Taken together, these results confirm the importance of the CXC chemokine angiogenic-angiostatic balance in the lung, which is altered in the IPF lung and during the pathogenesis of bleomycin-induced pulmonary fibrosis.
A recent study has raised the potential of a survival advantage for IPF patients treated with IFN-γ-1b (4). In a subsequent study, systemic treatment with IFN-β-1b seems to decrease the expression of profibrotic, proinflammatory, and angiogenic molecules, while markedly increasing the expression of CXCL11, but not CXCL9 or CXCL10 (5). To elucidate further whether the potential beneficial effects of IFN-γ-1b treatment in IPF patients were related to the expression in CXCL11, we studied the effects of systemic CXCL11 administration in a preclinical murine model of pulmonary fibrosis.
Administration of CXCL11 intramuscularly every day from 0 to 12 days led to reduced total lung collagen and procollagen I gene expression, compared with vehicle control-treated mice. Furthermore, histopathologic analysis of lung tissue displayed a decrease in the bleomycin-induced pulmonary fibrosis compared with control animals. Moreover, these effects were dependent on CXCR3, because inhibition of CXCR3 with specific neutralizing antibodies resulted in attenuation of the ability of CXCL11 to reduce pulmonary fibrosis. Based on these findings, we then set forth to determine the potential mechanisms through which CXCL11 mediated this effect. Fibroproliferation is a hallmark of pulmonary fibrosis (33). CXCL11 treatment of pulmonary fibroblasts had no significant effect, however, on the following parameters: their proliferative capacity in response to PDGF, transforming growth factor-β-induced procollagen I gene expression, or chemotaxis of fibroblasts in response to PDGF or EGF. Furthermore, pulmonary fibroblasts do not express the CXCL11 receptor, CXCR3, as measured by real-time quantitative polymerase chain reaction. A recent study has demonstrated that CXCL10 knockout mice developed a more pronounced pulmonary fibrotic response to bleomycin and this was mediated in part by an increased number of pulmonary fibroblasts (31). Although the presumed mechanism for this effect was suggested to be related to the ability of CXCL10 to inhibit fibroblast migration, CXCL10 in physiologically relevant concentrations in this study was found only modestly to inhibit pulmonary fibroblast migration, and fibroblasts were found not to express CXCR3 (31). Our results agree with the study (31), because we did not find expression of CXCR3 on primary cultures of murine or human fibroblasts. In our study, however, we found that CXCL11 in a dose-dependent manner had no effect for inhibiting chemotaxis of primary murine or human fibroblasts in response to PDGF, EGF, or bronchoalveolar lavage fluid from bleomycin-exposed animals. This finding is most consistent with the fact that these cells do not seem to express CXCR3.
CXCL11 is a potent chemoattractant for CXCR3-expressing cells and bleomycin-induced pulmonary fibrosis is associated with T cell infiltration, in which CD4^sup +^ or CD8^sup +^ lymphocytes may modulate production of profibrotic mediators from mononuclear phagocytes (42, 43). The fibrotic response to bleomycin has been shown to be significantly reduced in athymic mice (43). In addition, depletion of CD4^sup +^ and CD8^sup +^ lymphocytes has a greater than additive benefit over depletion of either the CD4^sup +^ or CD8^sup +^ lymphocyte subset alone (42). Further evidence of a role for CXCR3 and leukocyte recruitment in bleomycin-induced pulmonary fibrosis has recently been shown using CXCR3-deficient mice. CXCR3 knockout mice developed a more pronounced pulmonary fibrosis following intratracheal bleomycin, which is in part attributed to reduced intrapulmonary natural killer cells, measured at baseline and following bleomycin (44). Our findings for systemic administration of CXCL11, however, did not alter intrapulmonary populations of leukocytes, or leukocytes expressing CXCR3, including natural killer cells. Taken together, these studies support the notion that CXCL11 decreases bleomycin-induced pulmonary fibrosis by potential alternative biologic mechanisms.
Because previous studies have highlighted the importance of aberrant vascular remodeling in the lungs of IPF patients (11, 38-40) and during bleomycin-induced pulmonary fibrosis (23, 24), the angiogenic activity in the lung of the CXCL11-treated animals was evaluated. Using the cornea micropocket assay, we confirmed that there was decreased angiogenic activity in the lung of the CXCL11-treated bleomycin-exposed mice. This was further confirmed by the finding of a decrease in the number of endothelial cells in the lung. This finding indicates that CXCL11 treatment reduced intrapulmonary vascular remodeling. This is the first study to demonstrate that CXCL11 treatment attenuates angiogenesis in vivo.
Although there is evidence for reduced vascular remodeling in fibroblastic foci in the lung of patients with IPF (39, 40), these studies did not show a reduction of overall vascular remodeling that takes place in the lung of patients with usual interstitial pneumonia (UIP)-IPF. In fact, Turner-Warwick (8) clearly demonstrated marked vascular remodeling in the entire lung of patients who died from IPF. Our laboratory found marked vascular remodeling in areas of fibrosis in UIP of patients with IPF (11). Moreover, Ebina and colleagues (38) found similar findings to our results for vascular remodeling in the lung of patients with UIP-IPF. In fact, these investigators demonstrated a three-dimensional image reconstruction of combined immunolocalization of CD34 and vWF positive endothelial cells in fibrotic areas of UIP-IPF as compared with normal lung (38). There is no doubt that these data demonstrate and support the concept of marked and significant vascular remodeling in UIP-IPF as compared with normal lung (38). Although animal models of pulmonary fibrosis do not demonstrate areas compatible with fibroblastic foci, our strategy of attenuating vascular remodeling in animal models of pulmonary fibrosis is associated with a reduction of pulmonary fibrosis. We would further contend that no one truly knows what a fibroblastic foci represents, and whether having vascular remodeling in this lesion changes the progression of the disease. What we do have are data that come from ultrastructural analyses of UIP and that the fibroblastic foci most likely represents alveoli that have lost their epithelium, endothelium, and basement membrane, and have fused their walls (32, 45-47). This process leads to loss of any remnants of vasculature, and is consistent with the absence of vessel staining in fibroblastic foci.
The findings in this study indicate that systemic treatment with the IFN-inducible CXC chemokine, CXCL11, reduces bleomycin-induced pulmonary fibrosis. This effect was observed as a reduction in total lung collagen, gross histopathologic fibrosis, and aberrant vascular remodeling. The beneficial effects observed with systemic CXCL11 administration were not associated with alterations in infiltrating leukocyte numbers or fibroblast proliferation, or caused by a direct effect on fibroblast procollagen gene expression. Our findings support the hypothesis that CXCL11 inhibits fibroplasia and deposition of extracellular matrix by inhibiting vascular remodeling. Overall, this indicates that IFN-inducible CXC chemokines may provide a novel therapeutic intervention for the treatment of pulmonary fibrosis.
References
1. Coultas DB, Zumwalt RE, Black WC, Sobonya RE. The epidemiology of interstitial lung diseases. Am J Respir Crit Care Med 1994;150:967-972.
2. du Bois RM. Diffuse lung disease: a view for the future. Sarcoidosis Vasc Diffuse Lung Dis 1997;14:23-30.
3. Ziesche R, Hofbauer E, Wittmann K, Petkov V, Block LH. A preliminary study of long-term treatment with interferon gamma-lb and low-close prednisolone in patients with idiopathic pulmonary fibrosis. N Engl J Med 1999;341:1264-1269.
4. Raghu G, Brown KK, Bradford WZ, Starko K, Noble PW, Schwartz DA, King TE Jr. A placebo-controlled trial of interferon gamma-1b in patients with idiopathic pulmonary fibrosis. N Engl J Med 2004; 350:125-133.
5. Strieter RM, Starko KM, Enelow RI, Noth I, Valentine VG. Effects of interferon gamma-1b on biomarker expression in idiopathic pulmonary fibrosis patients. Am J Respir Crit Care Med 2004;170:133-140.
6. Strieter RM, Polverini PJ, Kunkel SL, Arenberg DA, Burdick MD, Kasper J, Dzuiba J, Van Damme J, Walz A, Marriott D, et al. The functional role of the ELR motif in CXC chemokine-mediated angiogenesis. J Biol Chem 1995;270:27348-27357.
7. Keane MP, Strieter RM. The role of CXC chemokines in the regulation of angiogenesis. Chem Immunol 1999;72:86-101.
8. Turner-Warwick M. Precapillary systemic-pulmonary anastomoses. Thorax 1963;18:225.
9. Moore BB, Arenberg DA, Addison CL, Keane MP, Strieter RM. Tumor angiogenesis is regulated by CXC chemokines. J Lab Clin Med 1998; 132:97-103.
10. Belperio JA, Burdick MD, Keane MP, Xue YY, Lynch JP III, Daugherty BL, Kunkel SL, Strieter RM. The role of the CC chemokine, RANTES, in acute lung allograft rejection. J Immunol 2000;165:461-472.
11. Keane MP, Arenberg DA, Lynch JP III, Whyte RI, Iannettoni MD, Burdick MD, Wilke CA, Morris SB, Glass MC, DiGiovine B, et al. The CXC chemokines, IL-8 and IP-10, regulate angiogenic activity in idiopathic pulmonary fibrosis. J Immunol 1997;159:1437-1443.
12. Keane MP, Strieter RM. The importance of balanced pro-inflammatory and anti-inflammatory mechanisms in diffuse lung disease. Respir Res 2002-3:5.
13. Keane MP, Wilke CA, Burdick MD, Morris SB, Glass MC, Strieter RM. CXC chemokines regulate angiogenic activity in acute lung injury. Chest 1999;116:93S-94S.
14. Strieter RM, Polverini PJ, Arenberg DA, Walz A, Opdenakker G, Van Damme J, Kunkel SL. Role of C-X-C chemokines as regulators of angiogenesis in lung cancer. J Leukoc Biol 1995;57:752-762.
15. Belperio JA, Keane MP, Burdick MD, Londhe V, Xue YY, Li K, Phillips RJ, Strieter RM. Critical role for CXCR2 and CXCR2 ligands during the pathogenesis of ventilator-induced lung injury. J Clin Invest 2002; 110:1703-1716.
16. Strieter RM, Belperio JA, Keane MP. CXC chemokines in angiogenesis related to pulmonary fibrosis. Chest 2002;122:298S-301S.
17. Koch AE, Volin MV, Woods JM, Kunkel SL, Connors MA, Harlow LA, Woodruff DC, Burdick MD, Strieter RM. Regulation of angiogenesis by the C-X-C chemokines interleukin-8 and epithelial neutrophil activating peptide 78 in the rheumatoid joint. Arthritis Rheum 2001;44: 31-40.
18. Romagnani P, Annunziato F, Lasagni L, Lazzeri E, Beltrame C, Francalanci M, Uguccioni M, Galli G, Cosmi L, Maurenzig L, et al. Cell cycle-dependent expression of CXC chemokine receptor 3 by endothelial cells mediates angiostatic activity. J Clin Invest 2001;107: 53-63.
19. Yang J, Richmond A. The angiostatic activity of interferon-inducible prolein-10/CXCL10 in human melanoma depends on binding to CXCR3 but not to glycosaminoglycan. Mol Ther 2004;9:846-855.
20. Murphy PM, Baggiolini M, Charo IF, Hebert CA, Horuk R, Matsushima K, Miller LH, Oppenheim JJ, Power CA. International union of pharmacology. XXII. Nomenclature for chemokine receptors. Pharmacol Rev 2000;52:145-176.
21. Lasagni L, Francalanci M, Annunziato F, Lazzeri E, Giannini S, Cosmi L, Sagrinati C, Mazzinghi B, Orlando C, Maggi E, et al. An alternatively spliced variant of CXCR3 mediates the inhibition of endothelial cell growth induced by IP-10, Mig, and I-TAC, and acts as functional receptor for platelet factor 4. J Exp Med 2003;197:1537-1549.
22. Belperio JA, Keane MP, Burdick MD, Lynch JP III, Xue YY, Li K, Ross DJ, Strieter RM. Critical role for CXCR3 chemokine biology in the pathogenesis of bronchiolitis obliterans syndrome. J Immunol 2002;169:1037-1049.
23. Keane MP, Belperio JA, Moore TA, Moore BB, Arenberg DA, Smith RE, Burdick MD, Kunkel SL, Strieter RM. Neutralization of the CXC chemokine, macrophage inflammatory protein-2, attenuates bleomycin-induced pulmonary fibrosis. J Immunol 1999;162:5511-5518.
24. Keane MP, Belperio JA, Arenberg DA, Burdick MD, Xu ZJ, Xue YY, Strieter RM. IFN-gamma-inducible protein-10 attenuates bleomycin-induced pulmonary fibrosis via inhibition of angiogenesis. J Immunol 1999;163:5686-5692.
25. Arenberg DA, Kunkel SL, Polverini PJ, Morris SB, Burdick MD, Glass MC, Taub DT, Iannettoni MD, Whyte RI, Strieter RM. Interferon-gamma-inducible protein 10 (IP-10) is an angiostatic factor that inhibits human non-small cell lung cancer (NSCLC) tumorigenesis and spontaneous metastases. J Exp Med 1996;184:981-992.
26. Smith RE, Strieter RM, Phan SH, Lukacs NW, Huffnagle GB, Wilke CA, Burdick MD, Lincoln P, Evanoff H, Kunkel SL. Production and function of murine macrophage inflammatory protein-1 alpha in bleomycin-induced lung injury. J Immunol 1994;153:4704-4712.
27. Phillips RJ, Burdick MD, Hong K, Lutz MA, Murray LA, Xue YY, Belperio JA, Keane MP, Stricter RM. Circulating fibrocytes traffic to the lungs in response to CXCL12 and mediate fibrosis. J Clin Invest 2004;114:438-446.
28. Blease K, Schuh JM, Jakubzick C, Lukacs NW, Kunkel SL, Joshi BH, Puri RK, Kaplan MH, Hogaboam CM. Stat6-deficient mice develop airway hyperresponsiveness and peribronchial fibrosis during chronic fungal asthma. Am J Pathol 2002;160:481-490.
29. Iwabu A, Smith K, Allen FD, Lauffenburger DA, Wells A. Epidermal growth factor induces fibroblast contractility and motility via a protein kinase C delta-dependent pathway. J Biol Chem 2004;279:14551-14560.
30. Li W, Fan J, Chen M, Guan S, Sawcer D, Bokoch GM, Woodley DT. Mechanism of human dermal fibroblast migration driven by type Γ collagen and platelet-derived growth factor-BB. Mol Biol Cell 2004; 15:294-309.
31. Tager AM, Kradin RL, LaCamera P, Bercury SD, Campanella GS, Leary CP, Polosukhin V, Zhao LH, Sakamoto H, Blackwell TS, et al. Inhibition of pulmonary fibrosis by the chemokinc IP-10/CXCL10. Am J Respir Cell Mol Biol 2004;31:395-404.
32. Kuhn C III, Boldt J, King TE Jr, Crouch E, Vartio T, McDonald JA. An immunohistochemical study of architectural remodeling and connective tissue synthesis in pulmonary fibrosis. Am Rev Respir Dis 1989;140:1693-1703.
33. Kuhn C, McDonald JA. The roles of the myofibroblast in idiopathic pulmonary fibrosis: ultrastructural and immunohistochemical features of sites of active extracellular matrix synthesis. Am J Pathol 1991; 138:1257-1265.
34. Peao MN, Aguas AP, de Sa CM, Grande NR. Neoformation of blood vessels in association with rat lung fibrosis induced by bleomycin. Anal Rec 1994;238:57-67.
35. Folkman J. Angiogenesis in cancer, vascular, rheumatoid and other disease. Nat Med 1995;1:27-31.
36. Henke C, Fiegel V, Peterson M, Wick M, Knighton D, McCarthy J, Bitterman P. Identification and partial characterization of angiogenesis bioactivity in the lower respiratory tract after acute lung injury. J Clin Invest 1991;88:1386-1395.
37. Marinelli WA, Henke CA, Harmon KR, Hertz MI, Bitterman PB. Mechanisms of alveolar fibrosis after acute lung injury. Clin Chest Med 1990;11:657-672.
38. Ebina M, Shimizukawa M, Shibata N, Kimura Y, Suzuki T, Endo M, Sasano H, Kondo T, Nukiwa T. Heterogeneous increase in CD34-positive alveolar capillaries in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med 2004;169:1203-1208.
39. Cosgrove GP, Brown KK, Schiemann WP, Serls AE, Parr JE, Geraci MW, Schwarz MI, Cool CD, Worthen GS. Pigment epithelium-derived factor in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med 2004;170:242-251.
40. Renzoni EA, Walsh DA, Salmon M, Wells AU, Sestini P, Nicholson AG, Veeraraghavan S, Bishop AE, Romanska HM, Panlelidis P, et al. Interstitial vascularity in fibrosing alveolitis. Am J Respir Crit Care Med 2003;167:438-43.
41. Keane MP, Belperio JA, Burdick MD, Lynch JP, Fishbein MC, Strieter RM. ENA-78 is an important angiogenic factor in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med 2001;164:2239-2242.
42. Piguet PF, Collart MA, Grau GE, Kapanci Y, Vassalli P. Tumor necrosis factor/cachectin plays a key role in bleomycin-induced pneumopathy and fibrosis. J Exp Med 1989;170:655-663.
43. Schrier DJ, Phan SH, McGarry BM. The effects of the nude (nu/nu) mutation on bleomycin-induced pulmonary fibrosis: a biochemical evaluation. Am Rev Respir Dis 1983;127:614-617.
44. Jiang D, Liang J, Hodge J, Lu B, Zhu Z, Yu S, Fan J, Gao Y, Yin Z, Homer R, et al. Regulation of pulmonary fibrosis by chemokine receptor CXCR3. J Clin Invest 2004;114:291-299.
45. Basset F, Ferrans VJ, Soler P, Takemura T, Fukuda Y, Crystal RG. Intraluminal fibrosis in interstitial lung disorders. Am J Pathol 1986; 122:443-461.
46. Corrin B, Dewar A, Rodriguez-Roisin R, Turner-Warwick M. Fine structural changes in cryptogenic fibrosing alvcolitis and asbestosis. J Pathol 1985;147:107-119.
47. McDonald JA. Idiopathic pulmonary fibrosis: a paradigm for lung injury and repair. Chest 1991;99:87S-93S.
Marie D. Burdick*, Lynne A. Murray*, Michael P. Keane, Ying Ying Xue, David A. Zisman, John A. Belperio, and Robert M. Strieter
Division of Pulmonary and Critical Care Medicine, Department of Medicine, and Departments of Pediatrics and Pathology and Laboratory Medicine, UCLA School of Medicine, Los Angeles, California
(Received in original form September 3, 2004; accepted in final form October 20, 2004)
Supported in part by National Institutes of Health grants NIH/NCI P50HL67665 (R.M.S. and M.P.K.), HL66027 (R.M.S.), CA87879 (R.M.S.), and P50CA90388 (R.M.S.).
* These two authors contributed equally to the manuscript.
Correspondence and requests for reprints should be addressed to Robert M. Strieter, M.D., Division of Pulmonary and Critical Care Medicine, Department of Medicine, David Geffen School of Medicine at UCLA, 14-154 Warren Hall, 900 Veteran Avenue, Los Angeles, CA 90095-1786. E-mail: rstrieter@mednet.ucla.edu
This article has an online supplement, which is accessible from this issue's table of contents at www.atsjournals.org
Am J Respir Crit Care Med Vol 171. pp 261-268, 2005
Originally Published in Press as DOI: 10.1164/rccm.200409-1164OC on October 22, 2004
Internet address: www.atsjournals.org
Conflict of Interest Statement: M.D.B. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; L.A.M. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; M.P.K. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; Y.Y.X. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; D.A.Z. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; J.A.B. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; R.S. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript.
Copyright American Thoracic Society Feb 1, 2005
Provided by ProQuest Information and Learning Company. All rights Reserved