According to the National Center for Health Statistics, nearly 12 million persons with asthma live in the United States. This inflammatory disease of the airways seems to be triggered by a variety of allergic and noxious substances that elicit bronchial hyperresponsiveness. This in turn causes wheezing and shortness of breath, as well as other symptoms. There is a close relationship between the intensity and extent of airway inflammation, bronchial hyperreactivity and the clinical manifestations of asthma. Therefore, anti-inflammatory medication is considered important, usually as first-line therapy.[1,2] Many physicians, however, use bronchodilators as primary treatment in patients with mild asthma and infrequent symptoms, adding anti-inflammatory medications as needed. With proper therapy, the asthmatic patient can maintain a normal activity level during exercise and sleep, achieve and maintain normal to near-normal pulmonary function, prevent chronic asthma symptoms and acute exacerbations, and limit visits to emergency departments and hospitals. Proper asthma management can be achieved through the creation of a partnership with asthma patients and by helping them understand and control their disease through physician-guided self-management.
Long-acting [Beta.sub.2]-Agonist Pharmacology
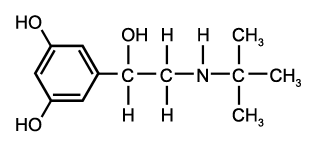
A new generation of beta2-agonist therapies, currently evolving, began with salmeterol (Serevent). Salmeterol has a long carbon side-chain[3,4] (Figure 1), which gives the molecule an extended duration of action -- at least 12 hours -- compared with albuterol (Proventil, Ventolin) or isoproterenol (Isuprel).[4,5]
While albuterol has a very rapid onset of effect, typically five to no more than 15 minutes, salmeterol has a delayed onset of action, nearly 20 minutes; therefore, this drug should not be used as acute therapy or in an emergency setting for the relief of bronchospasm.
[Beta.sub.2] agonists stimulate beta-adrenergic receptors, which are found on nearly every cell type in the lung, including airway epithelium, some mucosal glands, alveolar wall cells, vascular endothelium and the smooth muscle of the bronchi and pulmonary vessels. These receptors are also found on a variety of inflammatory cell membranes. The best understood function of stimulated [beta.sub.2] receptors in the lung is bronchial smooth muscle relaxation.
[BETA.sub.2] RECEPTORS AS ANTI-INFLAMMATORY AGENTS
Because [beta.sub.2] receptors are found on many other cells, some evidence indicates that their stimulation may favorably affect mediator release from immune effector cells, increase water content and secretions from mucous cells, enhance ciliary sweep rate on respiratory epithelial cells and even inhibit the movement of certain cells with pro-inflammatory capabilities through the vascular endothelial junctions. Therefore, when a [beta.sub.2] agonist is used, it is possible that more than bronchodilatation occurs.
It is obvious that salmeterol can be a potent bronchodilator but, since inflammation is so important in the pathophysiology of asthma, it is also necessary to consider the drug's potential anti-inflammatory actions. Salmeterol blocks the early and late asthmatic reactions to Whaled allergen and also subsequent airway hyperreactivity,[6,8] and in vitro studies have revealed that salmeterol can inhibit mast cell activation and degranulation,[9,10] and prevent increased vascular permeability in response to inflammatory mediators.[11]
SIDE EFFECTS
The side effects of salmeterol, which are similar to those of other [beta.sub.2] agonists, include tachycardia, palpitations, tremor, headache and hypokalemia.[12]
Over the past two years, a controversy has arisen over the potential role of [beta.sub.2]-agonist therapy in increasing the risk for asthma instability and death.[13-15 However, no rise in asthma mortality has occurred since salmeterol's introduction in the United Kingdom.[16] Furthermore, in large clinical trials extending from three months to one year, the incidence of asthma exacerbation and the use of rescue albuterol therapy decreased with the regular use of salmeterol.[4,5,17-19] Therefore, excess morbidity and mortality and increased asthma instability have not been identified with the regular use of salmeterol.
Salmeterol should not be used for "rescue" bronchodilatation during an acute asthmatic attack because of its delayed onset of action. Albuterol or another short-acting agent should be the drug of choice in an acute bronchospastic exacerbation.
Salmeterol: Clinical Studies
Oral sustained-release bronchodilators, in the forms of albuterol and theophylline, are being used as second-line therapy for control of asthma. Generally, patients with moderate and severe chronic asthma require multiple therapies for the prevention of asthma attacks.
Two controlled trials in more than 500 patients with mild-to-moderate asthma compared salmeterol (in a dosage of 42 [mu]g by inhalation twice daily) with albuterol (in a dosage of 100 [mu]g by inhalation four times daily) and placebo, over a 12-week study period.[3,4,19] Salmeterol was more effective in increasing morning and evening peak expiratory flow rates, improving overall asthma-symptom scores and decreasing the necessity for rescue used of albuterol. Patients also preferred salmeterol over albuterol. In patients regularly using salmeterol over three months' time, asthma deterioration was not evidenced. In the nearly one third of patients who were using inhaled corticosteroids on a regular basis, the addition of salmeterol further improved asthma control.
Studies of longer duration[18] have evaluated the regular use of salmeterol in patients with persistent asthma and found that both daytime and nighttime asthma control persisted without evidence of an increase in asthma deterioration.
Recent studies[20,21] have concentrated on quality of life in patients with asthma using salmeterol. Such factors as emotional well-being and tolerance to environmental stimuli have improved with the use of salmeterol. Patients have preferred the use of salmeterol, administered by inhalation twice daily, to the use of sustained-release theophylline titrated to therapeutic levels.[22]
SALMETEROL PLUS CORTICOSTEROIDS
The addition of salmeterol to inhaled corticosteroid therapy offers certain benefits. Adults and adolescents with asthma that continues to be symptomatic despite treatment with inhaled corticosteroids demonstrate benefit from additional salmeterol therapy.[23,24] Greening and colleagues[23] investigated to see if patients who continued to experience asthma symptoms on a regimen of 400 [mu]g daily of inhaled beclomethasone (Beclovent, Beconase, Vancenase) would do better with either an increased daily dose of inhaled corticosteroid (1,000 [mu]g daily) or the addition of salmeterol to the original steroid regimen. The addition of salmeterol not only caused a greater overall improvement in airflow but also further reduced daytime and nighttime symptoms and "rescue" bronchodilator use.
An Australian group[24] found similar results in an even more severely affected group of asthma patients in which the inhaled beclomethasone dosage reached 2,000 [mu]g daily. This study also showed a favorable effect with the addition of salmeterol therapy. In both of these large clinical trials; only a few adverse effects were recognited with salmeterol use and when this therapy was discontinued, all outcome variables, including airflow and bronchial hyperresponsiveness, returned to prestudy values without asthma deterioration. Most importantly, the asthma exacerbation rate, did not increase with the addition of salmeterol, suggesting that asthma control initially improved and was maintained.
Nocturnal Asthma
Asthma often manifests itself at night. Certain inflammatory and bronchial hyperreactivity changes may occur differently at night. These changes may relate to circadian rhythm alterations in neural and hormonal functions that influence airway inflammation. Nocturnal symptoms often suggest poor asthma control and require optimization of therapy. When nocturnal asthma symptoms persist despite optimization of therapy, the addition of a long-acting bronchodilator could be considered. Nocturnal asthma can be further controlled with a sustained-release form of albuterol and theophylline or inhaled salmeterol. U.S. trials[3,4,19] demonstrated a substantial increase in nights without asthmatic awakenings in patients treated on a regular basis with salmeterol. Fitzpatrick and associates[25] studied salmeterol therapy in patients with asthma and nocturnal symptoms. Airflow through the night improved in these patients, and "rescue" albuterol use in the salmeterol-treated group was reduced compared with the placebo-treated group. Finally, sleep architecture is improved through reduced wakefulness and increased deep-sleep time. Data suggest that salmeterol controls nocturnal asthma as effectively as oral slow-release terbutaline (Brethine, Bricanyl, Brethaire) and theophylline when administered once daily in the evening or twice daily.[26-28]
Exercise-Induced Bronchospasm
Exercise is an important asthma trigger in both children and adults. Exercise-induced bronchospasm is an increase in airflow obstruction that occurs either during or following vigorous exercise.
The use of an inhaled, short-acting [beta.sub.2] agonist or a mast cell stabilizer such as cromolyn (Intal) before exercise generally controls exercise-induced bronchospasm. In most patients with exercise-induced bronchospasm, albuterol, administered by inhalation five to 15 minutes before exercise, effectively controls symptoms. These short-acting agents generally have a duration of protection of about two hours.
Salmeterol can also be used to prevent exercise-induced bronchospasm. Two puffs of salmeterol from a metered-dose inhaler about 30 minutes to one hour before exercise can protect against exercise-induced bronchospasm for as long as six to 12 hours.[29] If repetitive exercise challenges are performed during this period of time, it is likely that the initial salmeterol treatment will provide protection. However, this therapy should be used episodically for the management of exercise-induced bronchospasm, because a recent study[30] suggests that some tolerance to salmeterol can occur in some patients with respect to exercise-induced bronchospasm.
Dosage
Salmeterol is available for use in a metered-dose inhaler, costing about $53.00 (one month's supply). Two puffs (42 [mu]g total from the mouthpiece) can be inhaled every 12 hours in patients 12 years of age or older. Well-controlled trials of salmeterol in pregnant women are inadequate. Dosages as high as four puffs every 12 hours can be used in adult patients with more serious chronic symptoms if they are not responsive to optimized inhaled anti-inflammatory therapy. However, this dosage level is more likely to result in adverse effects.
Salmeterol should generally be used in combination with inhaled anti-inflammatory agents. However, it can also be administered before exercise for prolonged protection against exercise-induced bronchospasm. Finally, salmeterol can also be used every 12 hours for the control of nocturnal asthma.
A metered-dose inhaler dispenses salmeterol without the need for a spacer delivery system. Although there is no information to_crate on the use of a spacer device with salmeterol therapy, we believe the drug can be used with a spacer device in patients who require such devices to enhance medication delivery to the lungs.
REFERENCES
[1.] National Heart, Lung"land Blood Institute. National Asthma Education Program. Expert Panel on the Management of Asthma. Guidelines for the diagnosis and management of asthma: Expert Panel Report. Bethesda, Md.: Dept of Health and Human Services, 1991; publication no. 91-3042.
[2.] Global initiative for asthma: global strategy for asthma management and prevention NHLBI/ WHO workshop report based on a March 1993 meeting). Bethesda, Md.: National Institutes of Health, National Heart, Lung and Blood Institute, 1995; NIH publication no. 95-3659.
[3.] Johnson M, Butchers PR, Coleman RA, Nials AT, Strong P, Sumner MJ, et al. The pharmacology of salmeterol. Life Sci 1993;52:2131-43.
[4.] Pearlman DS, Chervinsky P, LaForce C, Seltzer JM, Southern DL, Kemp JP, et al. A comparison of salmeterol with albuterol in the treatment of mild-to-moderate asthma. N Engl J Med 1992;327:1420-5.
[5.] D'Alonzo GE, Nathan RA, Henochowicz S, Morris RJ, Ratner P, Rennard SI. Salmeterol xinafoate as maintenance therapy compared with albuterol in patients with asthma. JAMA 1994;271:1412-6.
[6.] Twentyman OP, Finnerty JP, Harris A, Palmer J, Holgate ST. Protection against allergen-induced asthma by salmeterol. Lancet 1990;336:1338-42.
[7.] Pedersen B, Dahl R, Larsen BB, Venge P. The effect of salmeterol on the early- and late-phase reaction to bronchial allergen and postchallenge variation in bronchial reactivity, blood eosinophils, serum eosinophil cationic protein, and serum eosinophil protein X. Allergy 1993;48:377-82.
[8.] Taylor IK, O'Shaughnessy KM, Choudry NB, Adachi M, Palmer JB, Fuller RW. A comparative study in atopic subjects with asthma of the effects of salmeterol and salbutamol on allergen-induced bronchoconstriction, increase in airway reactivity, and increase in urinary leukotriene [E.sub.4] excretion. J Allergy Clin Immunol 1992;89:575-83.
[9.] Lau HY, Wong PL, Lai CK, Ho JK. Effects of long-acting [beta.sub.2]-adrenoreceptor agonists on mast cells of rat, guinea pig, and human. Int Arch Allergy Immunol 1994;105:177-80.
[10.] Butchers PR, Vardey CJ, Johnson M. Salmeterol: a potent and long-acting inhibitor of inflammatory mediator release from human lung. Br J Pharmacol 1991;104:672-6.
[11.] Whelan CJ, Johnson M, Vardey CJ. Comparison of the anti-inflammatory properties of formoterol, salbutamol and salmeterol in guinea-pig skin and lung. Br J Pharmacol 1993;110:613-8.
[17.] Ullman A, Hedner J, Svedmyr N. Inhaled salmeterol and salbutamol in asthmatic patients. An evaluation of asthma symptoms and the possible development of tachyphylaxis. Am Rev Respir Dis 1990;142:571-5.
[12.] Nathan RA, Seltzer JM, Kemp JP, Chervinsky P, Alexander WJ, Liddle R, et al. Safety of salmeterol in the maintenance treatment of asthma. Ann Allergy Asthma Immunol 1995;75:243-8.
[13.] Taylor DR, Sears MR, Herbison GP, Flannery EM, Print CG, Lake DC, et al. Regular inhaled beta agonist in asthma: effects on exacerbations and lung function. Thorax 1993;48:134-8.
[14.] Spitzer WO, Suissa S, Ernst P, Horwitz RI, Habbick B, Cockcroft D, et al. The use of [beta.sub.2]-agonists and the risk of death and near death from asthma. N Engl J Med 1992;326:501-6.
[15.] McFadden ER Jr. Perspectives in [beta.sub.2]-agonist therapy: vox clamantis in deserto vel lux in tenebris? J Allergy Clin Immunol 1995;95:641-51.
[16.] Devoy MA, Fuller RW, Palmer JB. Are there any detrimental effects of the use of inhaled long-acting [beta.sub.2]-agonists in the treatment of asthma? Chest 1995;107:1116-24.
[18.] Britton MG, Earnshaw JS, Palmer JB. A twelve month comparison of salmeterol with salbutamol in asthmatic patients. European Study Group. Eur Respir J 1992;5:1062-7 [Published erratum appears in Eur Respir J 1993;6:150].
[19.] D'Alonzo GE. Efficacy of inhaled salmeterol in the treatment of asthma. Eur Respir Rev 1995;5:128-32.
[20.] Rutten-van Molken MP, Custers F, van Doorslaer EK, Jansen CC, Heurman L, Maesen FP, et al. Comparison of performance of four instruments in evaluating the effects of salmeterol on asthma quality of life. Eur Res J 1995;8:888-98.
[21.] Juniper EF, Johnston PR, Borkhoff CM, Guyatt GH, Boulet LP, Haukioja A. Quality of life in asthma clinical trials: comparison of salmeterol and salbutamol. Am J Respir Crit Care Med 1995;151:66-70.
[22.] Fjellbirkeland L, Gulsvik A, Palmer JB. The efficacy and tolerability of inhaled salmeterol and individually dose-titrated, sustained-release theophylline in patients with reversible airways disease. Respir Med 1994;88:599-607.
[23.] Greening AP, Ind PW, Northfield M, Shaw G. Added salmeterol versus higher-dose corticosteroid in asthma patients with symptoms on existing inhaled corticosteroid. Allen & Hanburys Limited UK Study Group. Lancet 1994; 344:219-24.
[24.] Woolcock A, Lundback B, Ringdal N, Jacques LA. Comparison of addition of salmeterol to inhaled steroids with doubling of the dose of inhaled steroids. Am J Respir Crit Care Med 1996;153:1481-8.
[25.] Fitzpatrick MF, Mackay T, Driver H, Douglas NJ. Salmeterol in nocturnal asthma: a double-blind, placebo controlled trial of a long-acting inhaled [beta.sub.2]-agonist. BMJ 1990;301:1365-8.
[26.] Brambilla C, Chastang C, Georges D, Bertin L. Salmeterol compared with slow-release terbutaline in nocturnal asthma. A multicenter, randomized, double-blind, double-dummy, sequential clinical trial. French Multicenter Study Group. Allergy 1994;49:421-6.
[27.] Braun H, Koper I, Ukena D, Sybrecht GW. Salmeterol compared with theophylline in the treatment of nocturnal asthma. Eur Respir J 1993;6 (Suppl 17):383S.
[28.] Muir JF, Bertin L, Georges D. Salmeterol versus slow-release theophylline combined with ketotifen in nocturnal asthma: a multicentre trial. French Multicentre Study Group. Eur Respir J 1992;5:1197-200.
[29.] Kemp JP, Dockhorn RJ, Busse WW, Bleecker ER, Van As A. Prolonged effect of inhaled salmeterol against exercise-induced bronchospasm. Am J Respir Crit Care Med 1994;150:1612-5.
[30.] Ramage L, Lipworth BJ, Ingram CG, Cree IA, Dhillon DR Reduced protection against exercise-induced bronchoconstriction after chronic dosing with salmeterol. Respir Med 1094;88:363-8.
The Authors
GILBERT E. D'ALONZO, D.O. is professor of medicine and director of the Airways Disease Center at Temple University Health Sciences Center, Philadelphia. Dr. D'Alonzo graduated from the Philadelphia College of Osteopathic Medicine and completed a residency at Detroit Osteopathic Hospital. He also completed a fellowship at the University of Michigan Medical School, Ann Arbor.
KENNETH A. TOLEP, M.D. is assistant professor of medicine and director of the Pulmonary Rehabilitation Program at Temple University Health Sciences Center. Dr. Tolep graduated from State University of New York Health Science Center at Syracuse College of Medicine and completed a residency at Jefferson Medical College of Thomas Jefferson University, Philadelphia, and a fellowship at Temple University Health Sciences Center.
Address correspondence to Gilbert E. D'Alonzo, D.O., Airways Disease Center, Division of Pulmonary and Critical Care Medicine, 925 Parkinson Pavillion, Temple University Health Sciences Center, 3401 N. Broad St., Philadelphia, PA 19140.
COPYRIGHT 1997 American Academy of Family Physicians
COPYRIGHT 2004 Gale Group