Bromazepam
Bromazepam (marketed under brand names Compendium®, Creosedin®, Durazanil®, Lectopam®, Lexaurin®, Lexomil®, Lexotan®, Lexotanil®, Normoc®, Somalium®) is a drug which is a benzodiazepine derivative. It has sedative, hypnotic, anxiolytic and skeletal muscle relaxant properties. more...
Pharmacology
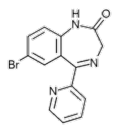
Its molecular structure is composed of a diazepine connected to two benzene rings, one of which has a bromine atom attached to it. It is a 1,4-benzodiazepine, which means that the nitrogens on the seven-sided diazepine ring are in the 1 and 4 positions.
Bromazepam binds to the GABA receptor GABAA, causing a conformational change and increasing inhibitory effects of GABA. Other neurotransmitters are not influenced. It does not possess any antidepressant qualities. Bromazepam shares with other benzodiazepines the risk of abuse, misuse, psychological and/or physical dependence. According to many psychiatric experts Bromazepam has a greater abuse potential than other benzodiazepines because of fast resorption and rapid onset of action. Due to its relatively short halflife and duration of action (8 to 12 hours), withdrawal symptoms may be more severe and more frequently encountered than with long acting benzodiazepines.
Bromazepam is reported to be metabolized by a hepatic enzyme belonging to the Cytochrome P450 family of enzymes. In 2003, a team led by Dr. Oda Manami at Oita Medical University reported that CYP3A4 was not the responsible enzyme, seeing as itraconazole, a known inhibitor of CYP3A4, did not effect its metabolism. In 1995, J. van Harten at Solvay Duphar B.V.'s Department of Clinical Pharmacology in Weesp reported that fluvoxamine, which is a potent inhibitor of CYP1A2, a less potent CYP3A4 inhibitor, and a negligible inhibitor of CYP2D6, does inhibit its metabolism.
The active metabolite of bromazepam is hydroxybromazepam.
Indications
- Short-term treatment of insomnia
- Short-term treatment of anxiety or panic attacks, if a benzodiazepine is required
- Alleviation of the symptoms of alcohol- and opiate-withdrawal, under close clinical supervision
Availability
Bromazepam is available as a generic in Canada, Germany, Italy, France, Portugal, Switzerland, It is also available in the United Arab Emirates, Venezuela and Columbia in the form of Lexotanil and in Brazil and Portugal in the form of Lexotan.
Dosage
Usually, 3mg to 6mg at bedtime, with additional 1.5mg to 3mg during the next day if needed. Malnourished patients, patients with compromised cardiovascular, liver or renal function, and elderly patients should receive lower doses. In hospitalized patients with severe agitation and/or anxiety, daily doses of up to 24mg have been given and tolerated for a limited period of time. A 3mg dose of bromazepam is equivalent to a 5mg dose of diazepam.
Read more at Wikipedia.org