Study objective: Many children with asthma go into long-term clinical remission at adolescence, but bronchial hyperresponsiveness (BHR) persists in some of these subjects. The regular use of inhaled corticosteroids improves BHR in patients with symptomatic asthma. The aim of this study was to determine whether BHR in adolescents with asthma remission could be reduced by prolonged treatment with inhaled corticosteroids.
Design: A randomized, double-blind, placebo-controlled, parallel study.
Patients: Thirty-seven adolescents with BHR and long-term remission of their asthma (neither symptoms nor any medication use during the previous 2 years).
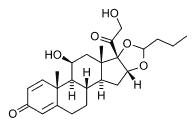
Intervention: Subjects received inhaled budesonide (two 200-[micro]g puffs bid; budesonide group, n = 19) or identical placebo (placebo group, n = 18) for 9 months. A separate group of patients with symptomatic asthma (symptomatic group, n = 19), using the same regimen of budesonide, was also studied.
Measurements and results: The provocative concentration of methacholine producing a 20% fall in [FEV.sub.1] (P[C.sub.20]) was measured before and every 3 months during treatment. There was no significant difference among the three groups for the baseline P[C.sub.20]. In neither the placebo nor the budesonide group did the geometric mean of P[C.sub.20] change significantly over the 9-month period. In contrast, a significant increase in P[C.sub.20] was noted in the symptomatic group as a result of the budesonide treatment.
Conclusion: Our data have shown that budesonide inhaled regularly for 9 months did not cause a significant improvement in the BHR of adolescents with long-term asthma remission. This suggests that the mechanism underlying BHR in this clinical setting may be different from that in symptomatic asthma. (CHEST 2001; 120:1140-1146)
Key words: adolescence; asthma; bronchial hyperresponsiveness; budesonide; clinical remission
Abbreviations: BHR = bronchial hyperresponsiveness; P[C.sub.20] = provocative concentration of methacholine producing a 20% fall in [FEV.sub.1]
Epidemiologic studies (1,2) have demonstrated that many children with asthma go into long-lasting clinical remission at adolescence. Bronchial hyperresponsiveness (BHR), often called "the hallmark of asthma," is known to be an important risk factor for the development of asthma (3) and a marker for the severity of disease as well as a measure of the need for therapy. (4) As the degree of bronchial responsiveness in asthmatic subjects is related to the severity of symptoms, it may be assumed that a clinical remission around the time of adolescence would be associated with normalized bronchial responsiveness. However, several studies (5,6) have shown a high prevalence of BHR in symptom-free and medication-free asthmatic adolescent patients.
Corticosteroids are currently the most effective anti-inflammatory drugs available for the treatment of asthma. (7) When inhaled corticosteroids are administered to symptomatic asthmatic subjects, bronchial responsiveness continues to improve for several months. (8,9) This reduction in BHR by corticosteroid treatment has been proposed (10) to be a consequence of the ability of the drug to control multiple components of airway inflammation. Little is known about the mechanism underlying BHR in adolescents with asthma in remission, and the effects of corticosteroid treatment on BHR in this clinical setting have received little attention.
The aim of this study was to determine whether BHR in patients with asthma remission during adolescence is reduced by prolonged treatment with inhaled corticosteroids. The results of this study may contribute to answering the question as to whether asymptomatic adolescents with persistent BHR would benefit from the use of inhaled corticosteroids, but also may help in the understanding of the mechanism underlying BHR in this setting. In this investigation, we conducted a randomized, double-blind, placebo-controlled study to assess the effects of a 9-month course of budesonide treatment on bronchial responsiveness.
MATERIALS AND METHODS
Subjects with long-term remission of their atopic asthma were recruited from patients between 10 years and 16 years of age who were attending the allergy clinic at Seoul National University Children's Hospital. All subjects had previously received a diagnosis of asthma on the basis of clinical criteria. (11) Thus, this diagnosis was based mainly on the clinical observation of recurrent episodes of bronchial obstruction responsive to bronchodilators and separated by symptom-free intervals of varying duration. Atopy was defined by at least one positive skin prick test result to a panel of 12 common aeroallergens in the presence of positive and negative controls. Most subjects showed a positive skin reaction to house dust mites. Long-term clinical remission was defined as neither asthmatic symptoms nor any asthmatic medication use during the previous 2 years. The complete absence of symptoms was reported despite normal physical activity. Two baseline measurements (spirometry and a methacholine provocation test) separated by an interval of 1 week were performed. To be eligible for the study, subjects needed to have a [FEV.sub.1] [greater than or equal to] 70% of the predicted value (12) and a provocative concentration of methacholine producing a 20% fall in [FEV.sub.1] (P[C.sub.20]) < 8 mg/mL in both measurements. Subjects with an upper or lower respiratory tract infection within 6 weeks of the start of the study were excluded. Subjects were randomly allocated into two treatment groups to receive either budesonide (two 200-[micro]g puffs bid; total dosage, 800 [micro]g/d; budesonide group) or placebo (two 500-[micro]g puffs bid of micronized lactose; placebo group), inhaled using a dry-powder inhaler (Turbuhaler; Astra; Sodertalje, Sweden). Drugs were supplied in identical devices so that patients and doctors were blinded to a particular subject's treatment allocation.
A separate group of symptomatic adolescents with atopic asthma (symptomatic group) was also recruited. The patients were selected on the basis of a history of episodic dyspnea or wheezing within the previous year, and a positive skin test result. All patients had mild symptoms, which were controlled by an inhaled bronchodilator on an as-needed basis with or without prophylactic medications (inhaled nedocromil sodium or inhaled corticosteroid). Patients who had received oral corticosteroids during the previous year were excluded. Subjects had a run-in period of 6 weeks, during which time any patients using prophylactic medication had it tapered off and discontinued for 4 weeks. Patients who had upper or lower respiratory tract infections or an asthma exacerbation during the run-in period were excluded. At the end of the run-in period, they underwent the two baseline measurements, 1 week apart, and the eligible criteria were the same as those used for subjects with long-term remission. The patients then received inhaled budesonide at the same dosage as the budesonide group, and were allowed to use inhaled [[beta].sub.2]-agonist on an as-needed basis to control their possible symptoms during the course of the study. Theophylline, which may reduce BHR, (13) was not allowed.
Subjects in the three groups were instructed to continue taking their assigned medications for 9 months, and follow-up visits were scheduled every 3 months; spirometry and a methacholine challenge test were performed at every visit. Subjects attended the laboratory at the same time of day on each occasion, having refrained from all the medications for 8 h and caffeine-containing beverages for 4 h. Measurements were made only during periods when the subjects were in clinically stable condition, and not within 4 weeks of viral respiratory illness. For respiratory tract infection with purulent sputum, antibiotics were administered. The Turbuhaler inhalation technique was checked before the start of the study and at every visit. Subjects were advised to rinse their mouth and throat after drug inhalation. Budesonide compliance was checked by examining a red mark in the indicator window of the Turbuhaler. In view of the fact that most of our patients were highly atopic to house dust mites, we decided to perform the study during the months of November to August in order to avoid the autumn season during which symptoms of house dust mite atopy are most prominent. (14)
[FEV.sub.1] was recorded from the best of three attempts using a computerized spirometer (Microspiro HI 298; Chest; Tokyo, Japan), with measurements not varying by > 5% being acceptable. Methacholine bronchial challenges were carried out using a modification of the method described by Chai et al. (15) Methacholine (Sigma Chemical; St. Louis, MO) solutions were prepared at concentrations of 0.075, 0.15, 0.3, 0.625, 1.25, 2.5, 5, 10, and 25 mg/mL in buffered saline solution (pH 7.4). A Rosenthal-French dosimeter (Laboratory for Applied Immunology; Baltimore, MD), triggered by a solenoid valve set to remain open for 0.6 s, was used to deliver the aerosol generated from a nebulizer (model 646; DeVilbiss; Somerset, PA) with pressurized air at 20 pounds per square inch. Each subject inhaled five inspiratory capacity breaths of buffered saline solution, and the study was continued only if the post-saline solution [FEV.sub.1] was at least 70% of the predicted value. Increasing concentrations of methacholine were then inhaled until the [FEV.sub.1] fell by > 20% of its post-saline solution value or the highest concentration was reached. The largest value of triplicate [FEV.sub.1]s at 1.5 min after each inhalation was used for analysis. The percentage fall of [FEV.sub.1] from the post-saline solution value was plotted against the log of the concentration of inhaled methacholine. P[C.sub.20] was then calculated by interpolation between two adjacent data points if the [FEV.sub.1] fell by > 20%.
Parents gave written informed consent for their children to participate in the study. The study protocol was approved by the Hospital Ethics Committee.
Statistical Analysis
For those subjects who did not achieve a 20% fall in [FEV.sub.1] with the highest concentration of methacholine (25 mg/mL) at follow-up, a P[C.sub.20] value of 25 mg/mL was assigned. Values for P[C.sub.20] were logarithmically transformed before analysis and were expressed as a geometric mean (range of 1 SD). Other values were presented as mean [+ or -] i SD. The mean of the two pretreatment [FEV.sub.1]s or P[C.sub.20]s was adopted as the baseline value. Changes in P[C.sub.20] after the treatment with respect to the pretreatment value were expressed as dose shift (in doubling doses) as defined by the following formula: [DELTA] [log.sub.10]P[C.sub.20][[log.sub.10](P[C.sub.20] after the treatment) - [log.sub.10](P[C.sub.20] before the treatment)]/[log.sub.10]2. (16) Student's t test for the paired data was used to analyze changes in [FEV.sub.1] or P[C.sub.20] with respect to the baseline value. Student's t test for the unpaired data was used for comparisons between the two groups. Prevalences between the two groups were compared with the [chi square] test. In each case, statistical significance was accepted when two-sided p values were < 0.05.
RESULTS
Sixty-three subjects (21 in each group) entered the study, but 7 subjects could not complete the study protocol: 3 subjects (1 subject in each group) were unable to perform the tests within 4 weeks of a scheduled visit because of viral respiratory tract infection, 2 subjects (1 subject in the budesonide group and 1 subject in the symptomatic group) had poor compliance with inhaled budesonide, and 2 subjects in the placebo group were unavailable for follow-up. Clinical characteristics of the subjects who completed the study are summarized in Table 1. There were no differences among the three groups in terms of age, sex ratio, atopic status as assessed by total serum IgE and the pattern of positive skin responses, and the baseline [FEV.sub.1] or P[C.sub.20].
Table 2 summarizes the mean [FEV.sub.1] levels before and after the treatment in the three groups. No increases in [FEV.sub.1] were detected over the 9-month period in the budesonide and placebo groups, while in the symptomatic group, a small but significant improvement was noted during the first 3 months, but no further improvement was observed during the following 6 months.
Figure 1 shows individual values of P[C.sub.20] before and after the treatment for the three groups. In neither the budesonide group nor the placebo group were there significant differences in P[C.sub.20] when the posttreatment values were compared with the baseline values: budesonide group geometric mean, 3.80 mg/mL (range of 1 SD, 1.51 to 9.55 mg/mL), 4.57 mg/mL (1.66 to 12.59 mg/mL), and 5.01 mg/mL (2.04 to 12.30 mg/mL); and placebo group geometric mean, 3.98 mg/mL (1.82 to 8.71 mg/mL), 4.27 mg/mL (1.91 to 9.55 mg/mL), and 5.01 mg/mL (2.04 to 12.30 mg/mL) at 3, 6, and 9 months of treatment, respectively. An increase or decrease in P[C.sub.20] by a twofold magnitude was observed on 19 occasions in the budesonide group and 18 occasions in the placebo group, and the distribution of frequency in either direction was not different between the budesonide group (increase, 15; decrease, 4) and placebo group (increase, 11; decrease, 7). Asthma symptoms redeveloped in two subjects in the placebo group at 4 months and 8 months after treatment, respectively. These subjects had a relatively lower baseline P[C.sub.20] (3.10 mg/mL and 2.07 mg/mL), and their P[C.sub.20] decreased to 0.88 mg/mL and 0.73 mg/mL, respectively, after asthma symptoms had recurred. In the symptomatic group, inhaled budesonide markedly increased the P[C.sub.20] to 9.55 mg/mL (4.57 to 19.95 mg/mL), 12.59 mg/mL (6.76 to 23.44 mg/mL), and 14.13 mg/mL (7.08 to 28.18 mg/mL) after 3, 6, and 9 months of treatment, respectively. All these values were significantly (p < 0.01) different from the baseline value. Use of [[beta].sub.2]-agonist during the previous 4 weeks was reported in 12 patients and 4 patients at baseline and 3 months, respectively (average weekly use, 6.1 puffs, 3.5 puffs). There was no report of use at 6 months and 9 months. An increase in P[C.sub.20] by a twofold magnitude was noted in 12, 13, and 16 subjects in the symptomatic group after 3, 6, and 9 months of treatment, respectively. A P[C.sub.20] of > 25 mg/mL, which is considered normal, (17) was observed after 9 months of treatment in two subjects (11%) in the budesonide group and none in the placebo group, compared with eight subjects (42%) in the symptomatic group.
[FIGURE 1 OMITTED]
Figure 2 shows the mean changes in P[C.sub.20] from the baseline values, expressed as doubling doses, during the 9-month treatment period in the three groups studied. The P[C.sub.20] increased by 0.08 [+ or -] 0.96, 0.35 [+ or -] 1.16, and 0.47 [+ or -] 0.90 doubling doses in the budesonide group after 3, 6, and 9 months of treatment, respectively, compared with 0.11 [+ or -] 0.83, 0.22 [+ or -] 0.93, and 0.45 [+ or -] 0.90 doubling doses in the placebo group. The difference between the two groups was not significant at any time point. In the symptomatic group, however, the P[C.sub.20] increased by 1.43 [+ or -] 0.95, 1.83 [+ or -] 0.92, and 1.97 [+ or -] 1.00 doubling doses after 3, 6, and 9 months of budesonide treatment, respectively. These values were significantly different from the corresponding values in the budesonide group (all p < 0.01).
[FIGURE 2 OMITTED]
DISCUSSION
This study shows that budesonide inhaled regularly for 9 months did not cause a significant improvement in the BHR of adolescent asthma patients with clinical remission. In contrast, the same treatment regimen markedly reduced BHR in adolescents with symptomatic asthma. These findings indicate distinctive patterns of response to corticosteroids in the BHR of remitted and symptomatic asthma, and may suggest that the mechanisms underlying BHR are not identical.
[FIGURE 1 OMITTED]
To our knowledge, this is the first study on the effects of inhaled corticosteroids on the BHR of adolescent patients with asthma in a long-term clinical remission. A randomized placebo-controlled study design enabled us to examine the longitudinal changes in BHR during adolescence. Although some fluctuations occurred in individual subjects, a small but nonsignificant improvement in P[C.sub.20] was observed in the placebo group. This is in agreement with the results of a previous study, (18) showing that former asthmatic patients had persistence of BHR over time. A similar trend in P[C.sub.20] was observed in the budesonide group, and there was no significant difference in the P[C.sub.20] changes between the budesonide and placebo groups. It is unlikely that the potential for improvement in BHR has been limited by confounding factors such as exposure to allergen, (19) or viral respiratory tract infections, (20) since the methacholine challenge tests were timed to avoid the peak house dust mite season and were not performed within 4 weeks of viral respiratory tract infection. Furthermore, no significant changes in P[C.sub.20] were found in the placebo group that was studied in parallel. The lack of an effect of the cortieosteroid treatment might be attributable to inadequate budesonide dosing or duration. However, this is also unlikely, since BHR in patients with symptomatic asthma was reduced significantly by the same treatment regimen. Other studies have demonstrated a marked effect with a dose of inhaled budesonide of 600 [micro]g/d (8) and over a treatment period as short as 2 months. (21) It should be mentioned that due to inadequate sample size, we may have failed to detect a small treatment effect. However, our sample size gave sufficient statistical power (> 80%) to detect such a degree of improvement in BHR as observed in previous studies, ie, on the order of one or two doubling doses, (22) if it is. From clinical practice, we expected relatively strongly hyperresponsive patients to show a greater response to inhaled corticosteroids than less hyperresponsive patients. To circumvent this potential problem, we selected subjects with mild asthma for the symptomatic group so that the baseline P[C.sub.20] in this group was comparable to that in the remitted groups. Therefore, the budesonide response discrepancy between the budesonide and symptomatic groups could not be accounted for by the baseline effect.
Although the mechanisms by which the regular use of inhaled corticosteroids reduces BHR in symptomatic asthma are not completely understood, corticosteroid-induced improvement in various measures of airway inflammation may be important. (10,23) The reason why BHR in clinical remission during adolescence fails to improve is not clear. It might be due to a distinctive type of airway inflammation that is not affected by current inhaled corticosteroid therapy. Because of the lack of data available on inflammatory changes in BHR in this clinical setting, we cannot answer the question. Although many studies (24) have found evidence of inflammation in the airways of asthmatic patients, several studies (25) have indicated that BHR and inflammatory cell infiltration are not necessarily linked. It has been shown that BHR may be the result of a chronic inflammatory process, with increased airway wall thickness and hypertrophy of the airway smooth muscle. (26,27) BHR caused by such an airway remodeling would not be influenced by corticosteroids. Genetic factors could offer another possible explanation. The importance of a familial predisposition and therefore a possible genetic transmission of BHR has been shown by several studies. (28,29) Inasmuch as this genetic factor exists in patients, it might be difficult for them to reach a normal level of bronchial responsiveness, even after the resolution of airway inflammation. It may be hypothesized that persistent BHR in clinical remission around adolescence may be related to hereditary factors, and is thus insensitive to the effects of corticosteroids.
Although bronchial responsiveness did not change in adolescents with clinical remission as a group, it should be noted that two subjects in the budesonide group showed an improvement up to normal levels of bronchial responsiveness and then appeared to reach a plateau. These patients had a relatively higher level of IgE (2,557 IU/mL and 809 IU/mL, respectively). This is in line with a previous study (30) that showed that a higher initial IgE level predicts a more favorable course of BHR in subjects with asthma who are treated with an inhaled corticosteroid. Another interesting finding was that two patients in the placebo group redeveloped asthmatic symptoms during the study period. Their levels of P[C.sub.20] seemed to be relatively lower at both initial and follow-up visits. Whether the degree of BHR has a prognostic significance in these patients remains to be determined by future studies.
What do our findings imply for clinical practice? Some studies (1,31) have asserted that the normalization of bronchial responsiveness should be an aim of treatment, as this is one of the known risk factors for symptomatic asthma in adulthood. Our findings suggest that this strategy does not apply to BHR in clinical remission during adolescence; we propose that treatment should be aimed at a symptomatic remission, ie, the normalization of symptoms, without need of additional bronchodilator. This is in agreement with a consensus report (32) on the treatment of asthma, in which a normalization of bronchial responsiveness was not stated as an aim to achieve.
In conclusion, BHR in clinical remission during adolescence was not improved significantly by inhaled corticosteroid therapy. This distinct pattern of response to corticosteroids compared to that of BHR in symptomatic asthma suggests that the mechanisms underlying BHR in the two clinical settings are not identical.
REFERENCES
(1) Gerritsen J, Koeter GH, Postma DS, et al. Prognosis of asthma from childhood to adulthood. Am Rev Respir Dis 1989; 140:1325-1330
(2) Sears MR. Evolution of asthma through childhood. Clin Exp Allergy 1998; 28(suppl 5):82-89
(3) Hopp RJ, Townley RG, Biven RE, et al. The presence of airway reactivity before the development of asthma. Am Rev Respir Dis 1990; 141:2-8
(4) Murray AB, Ferguson AC, Morrison B. Airway responsiveness to histamine as a test for overall severity of asthma in children. J Allergy Clin Immunol 1981; 68:119-124
(5) Boulet L-P, Turcotte H, Brochu A. Persistence of airway obstruction and hyperresponsiveness in subjects with asthma remission. Chest 1994; 105:1024-1031
(6) Gruber W, Eber E, Steinbrugger B, et al. Atopy, lung function and bronchial responsiveness in symptom-free paediatric asthma patients. Eur Respir J 1997; 1.0:1041-1045
(7) Barnes PJ, Pedersen S. Efficacy and safety of inhaled corticosteroids in asthma: report of a workshop held in Eze, France, October 1992. Am Rev Respir Dis 1993; 148:S1-S26
(8) Kerrebijn KF, van Essen-Zandvliet EE, Neijens HJ. Effect of long-term treatment with inhaled corticosteroids and [[beta]-agonists on the bronchial responsiveness in children with asthma. J Allergy Clin Immunol 1987; 79:653-659
(9) Juniper EF, Kline PA, Vanzieleghem MA, et al. Effect of long-term treatment with an inhaled corticosteroid (budesonide) on airway hyperresponsiveness and clinical asthma in nonsteroid-dependent asthmatics. Am Rev Respir Dis 1990; 142:832-836
(10) Djukanovic R, Wilson JW, Britten KM, et al. Effect of an inhaled corticosteroid on airway inflammation and symptoms in asthma. Am Rev Respir Dis 1992; 145:669-674
(11) American Thoracic Society. Standards for the diagnosis and care of patients with chronic obstructive pulmonary disease (COPD) and asthma. Am Rev Respir Dis 1987; 136:225-244
(12) Yoon KA, Lim HS, Koh YY, et al. Normal predicted values of puhnonary function tests in Korean school-aged children. J Korean Pediatr Assoc 1993; 36:25-37
(13) Page CP, Cotter T, Kilfeather S, et al. Effect of chronic theophylline treatment on the methacholine dose-response curve in allergic asthmatic subjects. Eur Respir J 1998; 12:24-29
(14) Paik YH, Cho YJ, You TH, et al. The seasonal variation of house dust mite allergen and the incidence of bronchial asthma among children. J Korean Med Assoc 1991; 34:69-77
(15) Chai H, Farr RS, Froelich LA, et al. Standardization of bronchial inhalation challenge procedures. J Allergy Clin Immunol 1975; 56:323-327
(16) Cockcroft DW, McParland CP, Britto SA, et al. Regular inhaled salbutamol and airway responsiveness to allergen. Lancet 1993; 342:833-837
(17) Shapiro GG, Furukawa CT, Pierson WE, et al. Methacholine bronchial challenge in children. J Allergy Clin Immunol 1982; 69:365-369
(18) Radford PJ, Hopp RJ, Biven RE, et al. Longitudinal changes in bronchial hyperresponsiveness in asthmatic and previously asthmatic children. Chest 1992; 101:624-629
(19) Cartier A, Thomson NC, Frith PA, et al. Allergen-induced increase in bronchial responsiveness to histamine: relationship to the late asthmatic response and change in airway caliber. J Allergy Clin Immunol 1982; 70:170-177
(20) Empey DW, Laitinen LA, Jacobs L, et al. Mechanisms of bronchial hyperreactivity in normal subjects after upper respiratory tract infection. Am Rev Respir Dis 1976; 113:131-139
(21) De Baets FM, Goeteyn M, Kerrebijn KF. The effect of two months of treatment with inhaled budesonide on bronchial responsiveness to histamine and house-dust mite antigen in asthmatic children. Am Rev Respir Dis 1990; 142:581-586
(22) van Grunsven PM, van Schayck CP, Molema J, et al. Effect of inhaled corticosteroids on bronchial responsiveness in patients with "corticosteroid naive" mild asthma: a meta-analysis. Thorax 1999; 54:316-322
(23) Lundgren R, Soderberg M, Horstedt P, et al. Morphological studies of bronchial mucosal biopsies from asthmatics before and after ten years of treatment with inhaled steroids. Eur Respir J 1988; 1:883-889
(24) Kirby JG, Hargreave FE, Gleich GJ, et al. Bronchoalveolar cell profiles of asthmatic and non-asthmatic subjects. Am Rev Respir Dis 1987; 136:379-383
(25) Crimi E, Spanevello A, Neri M, et al. Dissociation between airway inflammation and airway hyperresponsiveness in allergic asthma. Am J Respir Crit Care Med 1998; 157:4-9
(26) Fish JE, Peters SP. Airway remodeling and persistent airway obstruction in asthma. J Allergy Clin Immunol 1999; 104: 509-516
(27) Boulet L-P, Laviolette M, Turcotte H, et al. Bronchial subepithelial fibrosis correlates with airway responsiveness to methacholine. Chest 1997; 112:45-54
(28) Longo G, Strinati R, Poli F, et al. Genetic factors in nonspecific bronchial hyperreactivity: an epidemiologic study. Am J Dis Child 1987; 141:331-334
(29) Peat JK, Salome CM, Woolcock AJ. Factors associated with bronchial hyperresponsiveness in Australian adults and children. Eur Respir J 1992; 5:921-929
(30) Kerstjens HA, Schouten JP, Brand PL, et al. Importance of total serum IgE for improvement in airways hyperresponsiveness with inhaled corticosteroids in asthma and chronic obstructive puhnonary disease. Am J Respir Crit Care Med 1995; 151:360-368
(31) Kawasaki A, Mizushima Y, Hoshino K, et al. Bronchial hypersensitivity in asthmatics in long-term symptom-free state. Chest 1993; 103:370-375
(32) National Asthma Education and Prevention Program. Expert panel report 2: guidelines for the diagnosis and management of asthma. Bethesda, MD: National Institutes of Health, 1997; publication No. 97-4051
* From the Department of Pediatrics and Clinical Research Institute (Drs. Koh, Sun, and Lim), Seoul National University Hospital, Seoul; Department of Pediatrics (Dr. Kim), Inje University Sanggye Paik Hospital, Seoul; and Department of Pediatrics (Dr. Hong), Ulsan University College of Medicine, Seoul, Korea.
This study was supported in part by grant No. 04-98-029, from the Seoul National University Hospital Research Fund, and by year 1999 BK 21 Project For Medicine, Dentistry and Pharmacy. Manuscript received November 6, 2000; revision accepted March 21, 2001.
Correspondence to: Young Yull Koh, MD, Department of Pediatrics, Seoul National University Hospital, 28 yongon-dong, Chongno-gu, Seoul 110-744, Korea; e-mail: kohyy@plaza.snu.ac.kr
COPYRIGHT 2001 American College of Chest Physicians
COPYRIGHT 2001 Gale Group