The electroneutral Na-K-Cl co-transporter (NKCC) protein transports Na+,_K+ and Cl into cells under physiological conditions with a stoichiometry of 1Na+ : 1K+ : 2Cl-. NKCC is characteristically inhibited by the sulfamoylbenzoic acid 'loop" diuretics, such as bumetanide and furosemide. To date, only two distinct isoforms, NKCC1 and NKCC2, have been identified. NKCC1 has a broad tissue distribution, while the NKCC2 isoform is only found in vertebrate kidney. NKCC serves multiple functions, including ion and fluid movements in secreting or reabsorbing epithelia and cell volume regulation. However, understanding the role of NKCC1 in the central nervous system has just begun. NKCC1 protein is expressed in neurons throughout the brain. Dendritic localization of NKCC1 is found in both pyramidal and non-pyramidal neurons. NKCC1 is important in the maintenance of intracellular CT in neurons and contributes to GABA-mediated depolarization in immature neurons. Thus, NKCC1 may affect neuronal excitability through regulation of intracellular CT concentration. Expression of NKCC1 protein has also been found in astrocytes and oligodendrocytes. In addition to its role in the accumulation of Cl-, NKCC1 may also contribute to K+ clearance and maintenance of intracellular Na+ in glia. Our recent studies suggest that NKCCl activation leads to high [K+]^sub 0^-induced astrocyte swelling and glutamate release, as well as neuronal Na+, and Cl- influx during acute excitotoxicity. Inhibition of NKCC1 activity significantly reduces infarct volume and cerebral edema following cerebral focal ischemia. [Neurol Res 2005; 27: 280-286]
Keywords: Chloride transport; ion homeostasis; edema; Na+ overload; bumetanide; GABA; excitotoxicity
INTRODUCTION
The Na-K-Cl co-transporter (NKCC) belongs to the cation-chloride co-transporter family, which mediates the coupled movement of Na+ and/or K+ with Clacross the plasma membrane of cells1,2. Two isoforms of NKCC (NKCC1 and NKCC2) have been identified as two different gene products1'3. NKCCl and NKCC2 share 50-60% amino acid sequence homology and have distinct tissue distributions. NKCC1, which was first identified on the basolateral membranes of secretory epithelial cells, is referred to as the 'secretory' or 'house-keeping' NKCC1,3. In addition to secretory epithelial cells, NKCC1 is expressed in a wide variety of tissues including epithelial cells and non-epithelial cells2,4. NKCC1 plays a role in salt secretion and absorption, cell volume regulation and maintenance of intracellularCr concentration ([Cl-]/)1,2,4. NKCC1 null mice exhibit multiple tissue phenotype changes and functional disorders, including deafness, decreased blood pressure, intestinal bleeding, infertility and salivary secretion reduction4-6. These findings imply that NKCC1 is important to cellular function in a wide variety of tissues. In contrast to NKCC1, NKCC2 expression is confined to the apical membrane of the epithelial cells of the thick ascending limb of Henle's loop in kidney1. NKCC2 mutation is associated with Bartter syndrome, a renal tubular disorder4.
This review focuses on the role of NKCC1 in the central nervous system (CNS), especially under ischemic pathophysiological conditions. Interested readers are referred to a series of reviews that cover broader aspects of NKCC1,2,4.
NKCC1 TOPOLOGY AND CHARACTERISTICS
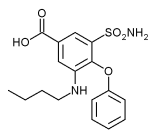
The molecular structure of NKCC1 has been proposed based on cDNA sequence analysis. The sequence analysis of shark rectal gland (sNKCC1) reveals that NKCC1 protein has 12 putative transmembrane domains (TM), flanked by large cytoplasmic amino and carboxyl termini, which contain some phosphorylation sites (Figure 7). There are potential N-linked glycosylation sites predicted on an extracellular loop between putative transmembrane segments 7 and 8s. NKCC1 in different tissues have molecular weights that vary from 120 to 190 kDa2. Using cDNA probes, a sNKCd human homologue has been identified in human colonie carcinoma line T84 cell8. Analysis of human NKCC1 (hNKCC1) found that hNKCC1 is composed of 1212 amino acids with 12 TM segments. The primary structure of hNKCC1 is 74% identical to sNKCC1 and 91% identical to a mouse Na-K-Cl cotransporter (mNKCC1)8. Although they share 74% homologue, sNKCC1 differs markedly from hNKCC1 in its affinities for the co-transported ions and for its inhibitor bumetanide8. The K^sub m^ for Na+, K+ and CP and the K, for bumetanide are 4-6-fold higher in the sNKCCI compared with hNKCC1(8). A chimera approach has revealed that differences in the hydrophobic TM domains contribute to this functional difference9,10. Site-directed mutagenesis studies show that changes in Na+ and Rb+ affinity result from changes in TM2, whereas Cl- affinity was affected by changes in TM4-7(10). The affinity for bumetanide was found to be affected by residues in the TM2-7 region, and also by residues in TM11 and TM12(10). In contrast, the conserved hydrophilic C termini of hNKCC1 and sNKCCI are not involved in the difference in affinities for the co-transported ions9.
There are two fundamental characteristics of NKCC function2. First, ion translocation by NKCC1 requires that all three ions (Na+ , K+ , Cl-) are simultaneously present on the same side of the membrane2. Secondly, ion transport mediated by NKCC is electroneutral in most cases, with a stoichiometry of 1 Na+ :1 K+ :2 Cl^sup -2^. In most cells, the driving force for ion influx is in part supplied by the inward Na+ gradient, maintained by Na+/K+-ATPase. However, in Cl- secretory epithelial cells, the Cl- gradient is also an important driving force for ion influx2. Sulfamoybenzoic acid loop diuretics such as bumetanide can compete with CP for the second Cl- binding site and thus inhibits NKCC1 function11. Bumetanide (IC^sub 50^~0.3µm) is the most widely used drug in NKCC1 inhibition and is more potent than other sulfamoybenzoic acid loop diuretics, such as furosemide (IC^sub 50^ ~ 7 µ)12.
NKCC2 REGULATION AND PHOSPHORYLATION
NKCC1 activity is regulated by multiple stimuli such as a decrease in [Cl-]^sub i^, hypertonic stress, an increase in intracellular Ca^sup 2+^ ([Ca^sup 2+^]^sub i^), and β-adrenergic receptor stimulation13,17. CP-mediated regulation of NKCC1 activity has been extensively studied in epithelial cells. Epithelium secrets CP through CP channels located on the apical membrane. A decrease in [CP], will increase the activity of basolateral membrane NKCC1, which will bring CP into the cell, thereby promoting continuous CP secretion across the apical membrane2.
Lytle et al, have demonstrated that a decrease in [Cl]^sub i^ stimulates both NKCC1 activity and NKCCl protein phosphorylation in epithelial cells18,19. The degree of NKCC1 activation is closely related to its phosphorylation and this suggests the CP-mediated regulation of NKCC1 activity is via phosphorylation19. Sequence analysis has revealed that Thr184 , Thr189, Thr202 and Thr1114 of N- and C-termini are the conserved regulatory phosphoracceptor residues in NKCC1(3,14).
Both kinases and phosphatases contribute to the precise regulation of NKCC1 activity through their opposite effects on NKCC1. Recently, several kinases have been proposed to mediate NKCC1 phosphorylation. OSR1 (oxidative stress response kinase) and SPAK (STE20/SPS-1 related, proline-alanine-rich kinase), along with its rat homologue PASK (proline-alaninerich STE20-related kinase), were found to bind to the third conserved domain in the NKCCl N-terminus and co-immunoprecipitated with NKCC1 protein20,21. Overexpression of PASK in HEK cells causes a small, but significant increase in both hNKCC1 and sNKCC1 activity, and the phosphorylation of PASK coincides with that of NKCC1(20).
PASK and SPAK are preferentially expressed in the brain, and in cells that are active in ion transport and rich in Na+ /K+ -ATPase21-23. PASK is suggested as a stress-related kinase due to its putative caspase cleavage site and its ability to activate p38 MAPK pathway23. Neurons, glia and epithelial choroid cells in the CNS have shown PASK expression24. In addition to PASK, other kinases, such as Rho, Janus kinase 2, CamKinase II, have been reported to be involved in NKCC1 regulation; however, there is lack of evidence for a direct interaction between these kinases and NKCC1(13,16,25).
On the other hand, protein phosphatase is responsible for dephosphorylation of NKCC1. The catalytic subunit of protein phosphatase 1 binds to the proteins that contain the consensus motif RVXFXD26. The N-terminus of NKCC1 contains a highly conserved RVNFVD sequence both in sNKCC1 (107-112) and hNKCC1 (140-145)26. The RVXFVD motif mutation produces an activation shift in NKCC1 regulation by Cl-. Dowd et al.20 have shown that dominant negative PASK (DNPASK) decreases the activity of hNKCCI by 80% and sNKCCI by 60%. In addition, protein phosphatase type 1 inhibitor calyculin A nearly completely restores NKCC1 activity in the DNPASK transfected cells20. These findings strongly suggest that an alteration in phosphorylation/dephosphorylation of NKCC1 regulates NKCC1 activity.
NKCC1-MEDIATED REGULATION OF K UPTAKE, INTRACELLULAR CL AND CELL VOLUME IN THE CNS
Immunohistological studies have shown NKCC1 expression in neurons, glia (astrocytes and oligodendrocytes), as well as choroid plexus epithelial cells and blood vessel endothelial cells27-30. Additional functional studies demonstrate that NKCC1 plays an important role in regulation of [CT-]^sub i^, K+ uptake and cell volume of cells in the CNS31-36.
γ-aminobutyric acid (GABA) and glycine are the main inhibitory neurotransmitters in the adult mammalian CNS. Activation of GABA receptors results in Cl- influx and hyperpolarization of the plasma membrane. However, during fetal and postnatal development, the equilibrium potential for CT is more positive than the resting potential and activation of GABA receptors triggers an excitatory response and a CT efflux31,37,38. The excitatory action of GABA in the immature CNS is important for the development of the nervous system39,40. Cells maintain Cl- homeostasis through the fine balance between inwardly-directed CT flux and Cl- extrusion systems. NKCC1 functions as a CT influx system and contributes to the active accumulation of intracellular CT in immature neurons31,32. An emerging hypothesis asserts that the balance between the inwardly-directed NKCC1 and the outwardly-directed neuronal K-Cl co-transporter (KCC2) may be important in the determination of GABA^sub A^ receptor-mediated depolarizing responses. This view is supported by the findings that expression of the inwardly-directed NKCC1 in neurons precedes expression of the outwardly-directed KCC2(41). Additionally, genetic ablation of NKCC1 leads to a decrease in resting [Cl-]^sub i^ and abolishes the GABA-mediated depolarization in mouse dorsal root ganglion cells32. Disruption of KCC2 results in frequent seizures, abolishment of respiration, and early lethality in mice due to anomalous excitatory actions of GABA and glycine42.
We found that opening of the GABA-activated CT channel or depletion of intracellular Cl- significantly stimulates NKCC1 activity in neurons16. This GABA-mediated stimulation could be the result of GABA^sub A^ receptor-mediated CT efflux. However, a loss of intracellular CT is associated with cell shrinkage, membrane depolarization, as well as a rise of [Ca^sup 2+^]^sub i^. The results of our recent study suggest that a GABA-mediated loss of intracellular CT, but not a subsequent membrane depolarization or shrinkage, leads to stimulation of NKCC1(17). This stimulation might be an important positive feedback mechanism to maintain intracellular CT level and GABA function in immature neurons.
The depolarizing effect of GABA is of functional importance during neuronal maturation and differentiation. The depolarizing action of GABA subsequently activates NMDA and voltage-gated Ca^sup 2+^ channels that leads to a rise in intracellular Ca^sup 2+^ and activation of a wide range of intracellular signaling pathways. Importantly, synergistic excitatory actions of GABA^sub A^ and glutamergic NMDA receptor have been found in the neonatal hippocampus39. The interplay between GABA and glutamate-mediated excitatory actions is required for the induction of synaptic plasticity during the development39,43. Interestingly, we found that NKCC1 in immature cortical neurons is stimulated by group-l mGluR and glutamate inotropic receptors NMDA- and AMPA-mediated signal transduction pathways16,17. The effects are dependent on a rise of intracellular Ca^sup 2+^. A synergistic interaction between GABA^sub A^ and NMDA receptors has been reported in formation of synchronous Ca^sup 2+^ oscillations39. Stimulation of NKCC1 by glutamate could increase intracellular Cl- that would reinforce the depolarizing actions of GABA16.
In addition to neurons, GABA also triggers a depolarizing efflux of Cl- in cultured oligodendrocytes44. Re-accumulation of intracellular Cl- after depletion is blocked by removal of extracellular Na+ or inhibition of NKCC1 activity45. Thus, NKCC1 may be important in maintaining high [Cl-]^sub i^ in oligodendrocytes. While the trophic effect of GABA on neurons is now well established46,47, the effect of GABA on oligodendrocyte survival and growth remains uncertain. Recently, we found that NKCC1 is present and active in rat spinal cord oligodendrocytes30. Expression of NKCC1 protein in the rat spinal cord is increased during development. In cultured oligodendrocytes, 39% of the total K+ (^sup 86^Rb+) influx represents NKCC1 activity. Activation of GABA^sub A^ receptors with muscimol produces a reduction in intracellular Cl- content and a stimulation of NKCC1 activity. Muscimol also triggers an increase in [Ca^sup 2+^]^sub i^; this increase depends on NKCC1 activity. Survival of oligodendrocytes following withdrawal of growth factors is enhanced by muscimol; this effect also requires NKCC1 activity30. Our results imply that NKCCl functions in rat oligodendrocytes to maintain [Cl-], above electrochemical equilibrium, and that it is required for GABAergic trophic effects.
NKCC1 also mediates K+ uptake in astrocytes35,36, which is important under pathophysiological conditions such as cerebral ischemia, when extracellular K+ concentration ([K+]^sub o^) is elevated (see later discussion). NKCC1 activity is important in maintaining cell volume. Inhibition of NKCC1 activity or genetic ablation of NKCC1 impairs regulatory volume increase in astrocytes and neurons following hypertonicity-induced cell shrinkage17,33,34. Finally, the epithelial cells in the choroid plexus are important for cerebrospinal fluid (CSF) production. NKCC1 is constitutively active in choroid plexus epithelial cells and functions to reabsorb K+ from the CSF, therefore, buffering and regulating brain interstitial K+ homeostasis28.
THE ROLE OF NKCC1 IN ISCHEMIC CELL DAMAGE
NKCC1 contributes to neuronal damage during acute excitotoxicity
Acute excitotoxic neurodegeneration after glutamate receptor activation is dependent on Na+ and Clentry48,49. Activation of NMDA and AMPA receptors stimulates NKCC1 activity in neurons16. Thus, NKCC1 may act as another mechanism that contributes to overload of Na+ and Cl- during glutamate-mediated acute excitotoxicity50. Excessive Na+ and Cl- accumulation subsequently induces cell damage though multiple downstream pathways (to be discussed later). We found that activation of NMDA receptors triggers a significant increase in [Na+]^sub i^ and intracellular ^sup 36^Cl content accumulation in cortical neurons. Blocking of NKCC1 activity with bumetanide abolishes the Claccumulation and attenuates the [Na+]^sub i^ rise by 52%50. Bumetanide also inhibits both glutamate and NMDA-mediated cell death50 (Figure 2). It has been established that oxygen-glucose deprivation (OCD)-induced neuronal death in mature neurons is mediated by NMDA ionotropic receptor-triggered excitotoxicity51. Rat cortical neuron cultures exhibit 70% cell death after 3 hours OGD and 21 hours re-oxygenation. OGD-mediated cell death is significantly attenuated by bumetanide, confirming the role of NKCC1 in excitotoxicity50. OGD treatment leads to significant cell swelling. Approximately 80% of neurons exhibit >30% swelling; however, inhibition of NKCC1 activity reduces the number of swollen cells to 43%50. The results imply that blocking of NKCC1 activity prevents neuronal swelling during OGD and thereby may reduce subsequent cell death.
In addition, in neurons with injured axons, Claccumulation is attributable to influx of Cl- mediated by NKCC1 and a decrease in Cl- extrusion by KCC52. This causes a switch of GABA action from inhibitory to excitatory and leads to excitotoxicity52. Blockage of Na+ and Cl- entry by removal of extracellular Na+ and Cl- abolishes excitotoxic dendritic injury and NMDA-mediated neurodeeeneration in retinal ganglion cells53,54.
NKCC1 co-transports Na+, K+, Cl- into cells and maintains the [Na+], in physiological conditions. However, under pathophysiological conditions, NKCC1 contributes to excessive Na+ influx50, which may induce cell damage via several mechanisms. Na+ entry causes cellular edema formation and extracellular space shrinkage55. Persistent Na+ influx also deteriorates neuronal tissue integrity by favoring Ca^sup 2+^ influx55. Na+ accumulation causes Ca^sup 2+^ influx through the reverse action of Na+-Ca^sup 2+^ exchanger (NCX)56. NCX normally extrudes 1 Ca^sup 2+^ in exchange for an influx of 3 Na+, thus transferring 1 postive charge into the cell. During ischemia, depolarization of the membrane may lead to reverse of NCX due to its electrogenic property in addition to the [Na+]^sub i^ increase57. NCX blockers (bepridil, benzamil, dichlorobenzamil) have shown the protection of the optic nerve from anoxic injury56.
During ischemia, total neuronal cell calcium content may increase to 150% of control or more58. It is widely accepted that intracellular Ca^sup 2+^ overloads activate multiple molecular cascades, which contribute to this eventual cell death. These include mitochondrial damage, phospholipase A^sub 2^ activation, stimulation of Ca^sup 2+^-dependent proteases, NO synthase and reactive oxygen species formation58.
NKCC1 contributes to astrocyte swelling and swelling-mediated EAA release
During ischemia, one significant pathophysiological change in the CNS is an elevation of [K+]^sub o^. A few minutes of anoxia/ischemia raises [K+]^sub o^ to ~60 mM59. Therefore, NKCC1 in astrocytes may play a role in K+ uptake under high [K+]^sub o^ conditions. In 75 mM [K+ NKCC1-mediated K+ influx was stimulated by 79% in astrocytes33. The high-[K+]^sub o^-induced activation of NKCC1 is completely abolished by either removal of extracellular Ca^sup 2+^ or blocking of L-type voltage-dependent Ca^sup 2+^ channels with nifedipine35. These data suggest that the co-transporter activity is stimulated under high [K+]^sub o^ via Ca^sup 2+^-mediated signal transduction pathways35. Intracellular ^sup 36^Cl- and Na+ accumulation is significantly increased in response to 75 mM [K+]^sub o^33,34. This increase is abolished by bumetanide or by genetic ablation of NKCC1(33,34). High [K+]^sub o^-mediated stimulation of NKCC1 can result in cell swelling via a net increase of intracellular Na+, K+, Cland accompanying water. 75 mM [K+]^sub o^ causes cell swelling in NKCC1+/+ astrocyte by 20%33. This high [K+]^sub o^-mediated swelling is abolished by inhibition of NKCC1 activity33,34 (Figure 3). High [K+]^sub o^-induced astrocyte swelling is also observed in the rat optic nerve model60. In enucleated nerves, light transmittance progressively increases in high [K+]^sub o^, which indicates astrocyte swelling. Furosemide and bumetanide can reversibly suppress the high [K+]^sub o^,-induced cell swelling60.
Glutamate release from astrocytes can occur in response to cell swelling via activation of volume-sensitive organic anion channels (VSOACs)61. Cells respond to swelling with a regulatory volume decrease mechanism. The volume decrease is partly mediated by efflux of amino acids through VSOACs61'62. The release of amino acids is blocked by the general anion channel blocker 5-nitro-2-(3-phenylpropylamino) benzoic acid and the non-specific anion transport inhibitor 4,4'-diisothiocyanostilbene-2,2'-disulfonic acid (DIDS)61. High [K+]^sub o^-triggered release of [^sup 14^C]-D-aspartate from astrocytes is abolished by DIDS, suggesting a VSOACs-mediated aspartate release33. Bumetanide or gene ablation of NKCC1 inhibits this high-[K+]^sub o^-induced aspartate release by 30~50%33,34 (Figure 4). The remaining release may be mediated by other mechanisms that activate VSOACs33,34.
Pharmacological inhibition of NKCC1 is neuroprotective in ischemic or traumatic injury
In vitro studies have established that NKCC1 is involved in cell damage under different ischemic conditions. Multiple in vivo studies have shown that NKCC1 plays a role in ischémie cell damage and its inhibition is neuroprotective29,63,64. Administration of bumetanide either prior to ischemia or during ischemia significantly reduces brain edema and infarction after 2 hours middle cerebral artery (MCA) occlusion and 24 hours reperfusion in rats29 (Figure 5). However, no protection is observed if bumetanide is administered only during reoxygenation63. This implies that activation of NKCC1 activity plays a role in the early stage of ischemic damage.
Focal cerebral ischemia leads to increased NKCC1 protein expression in ipsilateral cortex and striatum after 2 hours ischemia and 24 hours reperfusion in rats29. Up-regulation of NKCC1 is also found in hippocampus after 5 minutes global ischemia and 24 hours reperfusion in gerbils65. However, there is a transient downregulation of NKCC1 protein expression at 12 hours reperfusion, which may be a compensatory reaction to protect neurons from excitotoxicity65.
In addition to ischemia, NKCC1 may also contribute to brain swelling during traumatic injury64. Six hours after cold trauma leads to 9.76% swelling in ipsilateral hemisphere in rats64. Post-insult treatment with torasemide, a non-specific NKCC1 inhibitor, which can also block Cl- channels, significantly reduces brain swelling64. Although torasemide can result in a systemic dehydration that could affect brain edema, in these studies plasma osmolarity is not changed, suggesting that torasemide-mediated effects on brain swelling are through NKCC1 inhibition64.
CONCLUSION
NKCC1 has a broad tissue distribution and serves to maintain cellular ion homeostasis. Over the past decade, the function and regulation of NKCC1 have been extensively explored in epithelial cells. The results of these studies have revealed its structure, functional characteristics, and mechanisms underlying its activation, etc. However, the study of the role of NKCC1 in the CNS is relatively new and exciting. NKCC1 protein is expressed in multiple cell types throughout the brain. Through the maintenance of intracellular Cl-, NKCC1 activity is able to affect neuronal excitability and development. However, in vitro and/or in vivo studies show that NKCCl activation contributes to ischemic neuronal damage. Inhibition of NKCC1 protects neurons from ischemic damage in both in vitro and in vivo models. In addition, during high [K+]^sub o^ conditions, NKCC1 contributes to astrocyte swelling and glutamate release. In conclusion, NKCC1 is essential for normal ion homeostasis in the CNS. However, NKCC1 activation during cerebral ischemia results in a disruption of ion homeostasis that plays an important role in subsequent cell damage.
ACKNOWLEDGMENTS
This work was supported in part by an NIH grant (R01NS38118) and an NSF CAREER Award (IBN9981826) to D. Sun. The authors thank Douglas B. Kintner for helpful discussion.
REFERENCES
1 Haas M, Forbush B, III. The Na-K-Cl co-transporter of secretory epithelia. Ann Rev Physiol 2000; 62: 515-534
2 Russell JM. Sodium-potassium-chloride co-transport. Physiol Rev 2000; 80: 211-276
3 Xu JC, Lytle C, Zhu TT, et al. Molecular cloning and functional expression of the bumetanide-sensitive Na-K-Cl co-transporter. Proc Nat Acad Sci USA 1994; 91: 2201-2205
4 Delpire E, Mount DB. Human and murine phenotypes associated with defects in cation-chloride co-transport. Ann Rev Physiol 2002; 64: 803-843
5 Flagella M, Clarke LL, Miller ML, et al. Mice lacking the basolateral Na-K-2Cl co-transporter have impaired epithelial chloride secretion and are profoundly deaf. J Biol Chem 1999; 274: 26946-26955
6 Meyer JW, Flagella M, Sutliff RL, et al. Decreased blood pressure and vascular smooth muscle tone in mice lacking basolateral Na+K+-2Cl- co-transporter. Am J Physiol Heart Circ Physiol 2002; 283: H1846-H1855
7 Payne JA, Forbush B, III. Molecular characterization of the epithelial Na-K-Cl co-transporter isoforms. Curr Opin Cell Biol 1995; 7: 493-503
8 Payne JA, Xu JC, Haas M, et al. Primary structure, functional expression, and chromosomal localization of the bumetanide-sensitive Na-K-Cl co-transporter in human colon. J Biol Chem 1995; 270: 17977-17985
9 Isenring P, Forbush B, III. Ion and bumetanide binding by the Na-K-Cl co-transporter. Importance of transmembrane domains. J Biol Chem 1997; 272: 24556-24562
10 Isenring P, Jacoby SC, Chang J, et al. Mutagenic mapping of the Na-K-Cl co-transporter for domains involved in ion transport and bumetanide binding. J Gen Physiol 1998; 112: 549-558
11 Forbush B, III, Palfrey HC. [^sup 3^H]bumetanide binding to membranes isolated from dog kidney outer medulla. Relationship to the Na, K, Cl co-transport system. J Biol Chem 1983; 258: 11787-11792
12 O'Grady SM, Palfrey HC, Field M. Characteristics and functions of Na-K-Cl co-transport in epithelial tissues. Am J Physiol 1987; 253: C177-C192
13 Ciano-Oliveira C, Sirokmany G, Szaszi K, et al. Hyperosmotic stress activates Rho: differential involvement in Rho kinase-dependent MLC phosphorylation and NKCC activation. Am J Physiol Cell Physiol 2003; 285: C555-C566
14 Darman RB, Forbush B. A regulatory locus of phosphorylation in the N terminus of the Na-K-Cl co-transporter, NKCC1. J Biol Chem 2002; 277: 37542-37550
15 Kurihara K, Moore-Hoon ML, Saitoh M, et al. Characterization of a phosphorylation event resulting in upregulation of the salivary Na+-K+-2Cl- co-transporter. Am J Physiol 1999; 277: C1184-C1193
16 Schomberg SL, Su G, Haworth RA, et al. Stimulation of Na-K-2Cl co-transporter in neurons by activation of Non-NMDA ionotropic receptor and group-I mGluRs. J Neurophysiol 2001; 85: 2563-2575
17 Schomberg SL, Bauer J, Kintner DB, et al. Cross talk between the GABA^sub A^ receptor and the Na-K-Cl co-transporter is mediated by intracellular Cl-. J Neurophysiol 2003; 89: 159-167
18 Lytle C, Forbush B, III. Regulatory phosphorylation of the secretory Na-K-Cl co-transporter: modulation by cytoplasmic Cl. Am J Physiol 1996; 270: C437-C448
19 Haas M, McBrayer D, Lytle C. [Cl-],-dependent phosphorylation of the Na-K-Cl co-transport protein of dog tracheal epithelial cells. J Biol Chem 1995; 270: 28955-28961
20 Dowd BF, Forbush B. PASK (proline-alanine-rich STE20-related kinase), a regulatory kinase of the Na-K-Cl co-transporter (NKCC1). J Biol Chem 2003; 278: 27347-27353
21 Piechotta K, Lu J, Delpire E. Cation chloride co-transporters interact with the stress-related kinases Ste20-related proline-alanine-rich kinase (SPAK) and oxidative stress response 1 (OSR1). J Biol Chem 2002; 277: 50812-50819
22 Ushiro H, Tsutsumi T, Suzuki K, et al. Molecular cloning and characterization of a novel Ste20-related protein kinase enriched in neurons and transporting epithelia. Arch Biochem Biophys 1998; 355: 233-240
23 Johnston AM, Naselli G, Gonez LJ, et al. SPAK, a STE20/SPS1-related kinase that activates the p38 pathway. Oncogene 2000; 19: 4290-4297
24 Piechotta K, Garbarini NJ, England R, et al. Characterization of the interaction of the stress kinase SPAK with the Na+-K+-2Cl- co-transporter in the nervous system: evidence for a scaffolding role of the kinase. J Biol Chem 2003; 278: 52848-52856
25 Selvaraj NG, Omi E, Gibori G, et al. Janus kinase 2 (JAK2) regulates prolactin-mediated chloride transport in mouse mammary epithelial cells through tyrosine phosphorylation of Na+K+-2Cl- co-transporter. Mol Endocrinol 2000; 14: 2054-2065
26 Darman RB, Flemmer A, Forbush B. Modulation of ion transport by direct targeting of protein phosphatase type 1 to the Na-K-Cl co-transporter. J Biol Chem 2001; 276: 34359-34362
27 Sun D, Lytle C, O'Donnell ME. Astroglial cell-induced expression of Na-K-Cl co-transporter in brain microvascular endothelial cells. Am J Physiol 1995; 269: C1506-C1512
28 Wu Q, Delpire E, Hebert SC, et al. Functional demonstration of Na+-K+-2Cl co-transporter activity in isolated, polarized choroid plexus cells. Am J Physiol 1998; 275: C1565-C1572
29 Yan YP, Dempsey RJ, Sun D. Na+-K+-Cl- co-transporter in rat focal cerebral ischemia. J Cereb Blood Flow Metab 2001; 21: 711-721
30 Wang H, Yan Y, Kintner DB, et al. GABA-mediated trophic effect on oligodendrocytes requires Na-K-2Cl co-transport activity. J Neurophysiol 2003; 90: 1257-1265
31 Alvarez-Leefmans FJ. Intracellular chloride regulation. In: N. Sperelakis, ed., Cell Physiology Sourcebook: a molecular approach, San Diego: Academic Press, 2001, p. 301-318.
32 Sung KW, Kirby M, McDonald MP, et al. Abnormal GABA^sub A^ receptor-mediated currents in dorsal root ganglion neurons isolated from Na-K-2Cl co-transporter null mice. J Neurosci 2000; 20: 7531-7538
33 Su G, Kintner DB, Sun D. Contribution of Na+-K+-Cl- co-transporter to high [K+]^sub o^-induced swelling and EAA release in astrocytes. Am J Physiol Cell Physiol 2002; 282: C1136-C1146
34 Su G, Kintner DB, Flagella M, et al. Astrocytes from Na+-K+-Clco-transporter-null mice exhibit absence of swelling and decrease in EAA release. Am J Physiol Cell Physiol 2002; 282: C1147-C1160
35 Su G, Haworth RA, Dempsey RJ, Sun D. Regulation of Na+-K+CP co-transporter in primary astrocytes by dibutyryl cAMP and high [K+]^sub o^. Am J Physiol Cell Physiol 2000; 279: C1710-C1721
36 Walz W. Role of Na/K/Cl co-transport in astrocytes. Can J Physiol Pharmacol 1992; 70 Suppl: S260-S262
37 Misgeld U, Deisz RA, Dodt HU, et al. The role of chloride transport in postsynaptic inhibition of hippocampal neurons. Science 1986; 232: 1413-1415
38 Cherubini E, Gaiarsa JL, Ben Ari Y. GABA: an excitatory transmitter in early postnatal life. Trends Neurosci 1991; 14: 515-519
39 Ben Ari Y, Khazipov R, Leinekugel X, et al. GABA^sub A^, NMDA and AMPA receptors: a developmentally regulated 'menage a trois'. Trends Neurosci 1997; 20: 523-529
40 LoTurco JJ, Owens DF, Heath MJ, et al. GABA and glutamate depolarize cortical progenitor cells and inhibit DNA synthesis. Neuron 1995; 15: 1287-1298
41 Payne JA, Rivera C, Voipio J, et al. Cation-chloride co-transporters in neuronal communication, development and trauma. Trends Neurosci 2003; 26: 199-206
42 Hubner CA, Stein V, Hermans-Borgmeyer I, et al. Disruption of KCC2 reveals an essential role of K-Cl co-transport already in early synaptic inhibition. Neuron 2001; 30: 515-524
43 Belhage B, Hansen GH, Elster L, et al. Effects of gamma-aminobutyric acid (GABA) on synaptogenesis and synaptic function. Perspect Dev Neurobiol 1998; 5: 235-246
44 Kettenmann H, Blankenfeld GV, Trotter J. Physiological properties of oligodendrocytes during development. Annl NY Acad Sci 1991; 633: 64-77
45 Hoppe D, Kettenmann H. GABA triggers a Cl- efflux from cultured mouse oligodendrocytes . Neurosci Lett 1989; 97: 334-339
46 Marty S, Berninger B, Carroll P, et al. GABAergic stimulation regulates the phenotype of hippocampal interneurons through the regulation of brain-derived neurotrophic factor. Neuron 1996; 16: 565-570
47 Fukuda A, Muramatsu K, Okabe A, et al. Changes in intracellular Ca^sup 2+^ induced by GABA^sub A^ receptor activation and reduction in Clgradient in neonatal rat neocortex. J Neurophysiol 1998; 79: 439-446
48 Rothman SM. The neurotoxicity of excitatory amino acids is produced by passive chloride influx. J Neurosci 1985; 5: 1483-1489
49 Choi DW, Maulucci-Gedde M, Kriegstein AR. Glutamate neurotoxicity in cortical cell culture. J Neurosci 1987; 7: 357-368
50 Beck J, Lenart B, Kintner DB, et al. Na-K-Cl co-transporter contributes to glutamate-mediated excitotoxicity. J Neurosci 2003; 23: 5061-5068
51 Gwag BJ, Koh JY, DeMaro JA, et al. Slowly triggered excitotoxicity occurs by necrosis in cortical cultures. Neuroscience 1997; 77: 393-401
52 Nabekura J, Ueno T, Okabe A, et al. Reduction of KCC2 expression and GABA^sub A^ receptor-mediated excitation after in vivo axonal injury. J Neurosci 2002; 22: 4412-4417
53 Hasbani MJ, Hyrc KL, Faddis BT, et al. Distinct roles for sodium, chloride, and calcium in excitotoxic dendritic injury and recovery. Exp Neurol 1998; 154: 241-258
54 Chen Q, Olney JW, Lukasiewicz PD, et al. Ca^sup 2+^-independent excitotoxic neurodegeneration in isolated retina, an intact neural net: a role for Cl- and inhibitory transmitters. Mol Pharmacol 1998; 53: 564-572
55 Xie Y, Dengler K, Zacharias E, et al. Effects of the sodium channel blocker tetrodotoxin (TTX) on cellular ion homeostasis in rat brain subjected to complete ischemia. Brain Res 1994; 652: 216-224
56 Stys PK, Waxman SG, Ransom BR. Ionic mechanisms of anoxic injury in mammalian CNS white matter: role of Na+ channels and Na+-Ca^sup 2+^ exchanger. J Neurosci 1992; 12: 430-439
57 Leppanen L, Stys PK. Ion transport and membrane potential in CNS myelinated axons. II. Effects of metabolic inhibition. J Neurophysiol 1997; 78: 2095-2107
58 Kristian T, Siesjo BK. Calcium in ischemic cell death. Stroke 1998; 29: 705-718
59 Siesjo BK. Pathophysiology and treatment of focal cerebral ischemia. Part I: pathophysiology. J Neurosurg 1992; 77: 169-184
60 MacVicar BA, Feighan D, Brown A, et al. Intrinsic optical signals in the rat optic nerve: role for K+ uptake via NKCC1 and swelling of astrocytes. Glia 2002; 37: 114-123
61 Rutledge EM, Aschner M, Kimelberg HK. Pharmacological characterization of swelling-induced D-[^sup 3^H]aspartate release from primary astrocyte cultures. Am J Physiol 1998; 274: 1-20
62 Kimelberg HK, Mongin AA. Swelling-activated release of excitatory amino acids in the brain: relevance for pathophysiology. Contrib Nephrol 1998; 123: 240-257
63 Yan Y, Dempsey RJ, Flemmer A, et al. Inhibition of Na+-K+-Clco-transporter during focal cerebral ischemia decreases edema and neuronal damage. Brain Res 2003; 961: 22-31
64 Staub F, Stoffel M, Berger S, et al. Treatment of vasogenic brain edema with the novel Cl- transport inhibitor torasemide. J Neurotrauma 1994; 11: 679-690
65 Kang TC, An SJ, Park SK, et al. Changes in Na+-K+-Cl- co-transporter immunoreactivity in the gerbil hippocampus following transient ischemia. Neurosci Res 2002; 44: 249-254
Mai Chen1,2 and Dandan Sun2,3
1 Neuroscience Training Program, Departments of 2 Neurosurgery and 3 Physiology, University of Wisconsin Medical School, Madison, WI 53792, USA
Correspondence and reprint requests to: Dandan Sun, Department of Neurological Surgery, University of Wisconsin Medical School, H4/332 Clinical Sciences Center, 600 Highland Ave, Madison, WI 53792, USA. [sun@neurosurg.wisc.edu] Accepted for publication December 2004.
Copyright Maney Publishing Apr 2005
Provided by ProQuest Information and Learning Company. All rights Reserved