A 63-year-old black man with a history of essential hypertension, diabetes mellitus type II, atherosclerotic heart disease, and osteoarthritis presented to the emergency department with generalized edema and orthopnea. He had been examined periodically in recent months because of progressive congestive heart failure (CHF) and peripheral edema. Increasing doses of diuretics and a sodium-restricted diet failed to be effective. Current treatment consisted of furosemide 60 mg 2 times a day, potassium supplements, digoxin 0.25 mg daily, enalapril 10 mg daily, slow-release metformin 1000 mg daily, and a low-sodium, low-carbohydrate, cholesterol-poor diet. In addition, the patient had been taking ibuprofen for chronic osteoarthritis. Despite compliance with his medications, he noticed progressive weakness, fluid retention, frequent attacks of paroxysmal nocturnal dyspnea, and an inability to perform minor tasks around the house. He denied having any chest pains or palpitations.
Physical examination revealed a dyspneic patient with anasarca and prominent jugular venous distention at 60[degrees]. His weight was 74 kg (165 lbs), height 1.65 m (5 ft 5 in), blood pressure 150/70 mm Hg, and heart rate 110 beats/minute and regular. There was a widely displaced point of maximal impulse, an [S.sub.3], [S.sub.4] summation gallop and a II/VI regurgitant mitral murmur. Dullness to percussion, decreased breath sounds, and late inspiratory rales were present in both lower lung fields. Laboratory work revealed the following: sodium 135 mmol/L, potassium 3.0 mmol/L, blood glucose 10 mmol/L (180 mg/dL), serum urea nitrogen 25.0 mmol/L (70 mg/dL), creatinine 212 [micro]mol/L (2.4 mg/dL), P[O.sub.2] 58 mm Hg, and PC[O.sub.2] 2.3 mm Hg. Urine was negative for sugar and acetone. Chest radio graphs confirmed global cardiomegaly and bilateral pleural effusions. An electrocardiogram revealed low voltage, sinus tachycardia, and left bundle branch block. The digoxin level was 2.4 nmol/L (1.9 ng/mL).
Following the physical examination, further questioning revealed that the patient had not adhered to a strict salt-poor diet.
QUESTIONS
1. Which of the following would you expect to be the most effective therapeutic intervention for severe CHF with anasarca?
a. water restriction
b. intravenous nitroglycerin for its unloading effect
c. combination diuretics (ie, loop diuretic and metolazone)
d. angiotensin-converting enzyme inhibitor (ACEI)
e. spironolactone
2. Cardiac output (CO) is determined by which of the following?
a. contractility
b. capillary function
c. afterload
d. preload
e. cardiac rhythm
3. The goals in heart failure (HF) management include which of the following?
a. improve left ventricular (LV) function
b. prevent premature death
c. increase contractile force of LV with an intrope
4. Diuretic therapy can reduce heart size and increase LV efficiency by which of the following?
a. reducing circulating volume
b. reducing cardiac filling pressures
c. decreasing neurohormonal activation
d. stabilizing electrolytes
5. The types of diuretics routinely used in HF are which of the following?
a. loop diuretics
b. thiazide diuretic
c. potassium-sparing diuretic
d. ACEI
6. The adaptive neurohormonal activity that occurs early in HF includes which of the following?
a. the renin-angiotensin-aldosterone system (RAAS)
b. the sympathetic nervous system
c. the endothelial system
d. the natriuretic peptides
e. the hypothalamic system
f. all of the above
ANSWERS
1. c. combination diuretics (ie, loop diuretic and metolazone)
d. ACEI
e. spironolactone
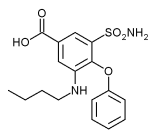
The use of drugs that influence function in different segments of the nephron and act synergistically to promote water and sodium diuresis has proved to be one of the most effective therapeutic measures for severe CHF. The combination of a loop diuretic (eg, ethacrynic acid, furosemide, or bumetanide) and metolazone is a powerful diuretic combination. Metolazone is similar to a thiazide diuretic, but has longer action. Intravenous loop diuretics are preferred and more effective. The gastric passive congestion in advanced HF limits absorption of orally administered diuretics. Reports have demonstrated the superiority of ACEI combined with diuretics over other forms of therapy (vasodilators and inotropic agents). Captopril (the first oral ACEI) and enalapril (a long-acting ACEI) are effective venous and arterial vasodilators that are mediated by suppression of angiotensin-II formation. In addition, they attenuate the release of antidiuretic hormones and circulating catecholamines and stimulate the formation of vasodilatory prostaglandins in the kidneys, all of which are beneficial in CHF. An ACEI has a weak diuretic effect; the addition of diuretics is necessary for effective diuresis. During states of ineffective arterial volume, local production of vasodilatory prostanoids and kinins in the kidney offsets the decrease in renal blood flow and helps maintain the glomerular filtration rate. ACEIs have been shown to stimulate the production of these vasoactive substances, thus contributing to the amelioration of intrarenal hemodynamics. Improvement of hyponatremia is usually seen within 48 hours of initiation of combined therapy and reaches a peak after approximately 2 weeks. This correlates with significant improvement in cardiac and renal function and weight loss related to brisk diuresis without accompanying hypokalemia. These effects are sustained during chronic therapy.
Spironolactone, an aldosterone antagonist, has been reestablished as having a significant role in the management of HF. Spironolactone is a potassium-sparing diuretic that acts on the distal nephron and collecting duct. Spironolactone reduces heart rate, increases heart rate variability, and decreases cardiac mortality in patients with CHF. This mineralocorticoid receptor was first identified in the kidney, but now it is known to be present in the heart, brain, and blood vessels as well. Aldosterone can act as a paracrine hormone in many organs.
Oxygen supplementation, salt restriction, upright positions in bed, and preferably bedside chair care are standard adjunctive therapeutic measures. Water restriction has a minor clinical impact in this setting and may cause significant discomfort. Finally, a beta blocker should be added to the therapy of CHF when the failure has been controlled and stabilized. [beta]-Blockers are started at low doses and progressively increased to therapeutic levels over a 3- to 4-week period. Digitalis, primarily an inotrope, is no longer considered essential in the management of a failing weak ventricle. (1)
2. a. contractility
c. afterload
d. preload
e. cardiac rhythm
CHF is an enormous health, social, and economic problem. More than 5 million persons in the United States are affected with HF, and about 50% are estimated to have asymptomatic LV dysfunction that therefore remains undiagnosed. Early identification and intervention are critical in controlling CHF and halting its progression. CHF is a clinical syndrome with symptoms and signs due to the inability of the heart to pump an adequate volume of blood to meet the body's metabolic needs, with the proviso that there is an adequate return of blood volume to the right side of the heart. Cardiac function is governed by any 1 or more of 4 hemodynamic factors: contractility, preload, afterload, and cardiac rhythm. Alteration in any one of these factors can critically reduce CO to a level that no longer meets the circulatory demands of the body, thus precipitating HF.
Cardiac muscle dysfunction in HF may be attributed to either impaired ventricular contraction (systolic dysfunction) or impaired ventricular relaxation (diastolic dysfunction) or both. In systolic failure, ventricular end-diastolic pressure and volume increase, whereas in diastolic failure only ventricular end-diastolic pressure increases (end-diastolic volume is normal). Hypertensive heart disease and obstructive cardiomyopathy characteristically have impaired ventricular relaxation and exemplify diastolic dysfunction.
3. a. improve LV function
b. prevent premature death
Since CO is governed by afterload, preload, contractility, and heart rate, therapy in HF requires stabilization of all 4 of these determinants. In general, the aim of both pharmacological and nonpharmacological interventions is to relieve symptoms, improve LV function, and extend life span. Advances in cardiovascular disease have helped elucidate the basis of many disease processes, and as a result, reversal of diseases and curing CHF have been possible. The cornerstone of HF therapy is the control of sodium and water retention. Although polypharmacy is routine, therapy can never succeed without primary attention to the role of sodium elimination in HF. Dietary salt restriction and diuretics are mandatory if compensation is to be achieved. Early in the fourth decade of the 20th century, HF therapy was largely symptomatic in nature and consisted of restricting physical activity and reducing sodium and water retention so as to lower the circulating volume and thereby reduce cardiac overload. In the 1950s, treatments for HF included sedation, bed rest, sodium-restricted diet, digitalis, and thiazide diuretics. The thiazides act by inhibiting sodium transport in the distal tubule. In acute LV failure with pulmonary edema, phlebotomy, rotating tourniquets, and parenteral mercurial diuretics were effective. Not infrequently 3 to 5 mg of intravenous morphine sulfate dramatically reversed the marked apprehension and dyspnea in patients with acute pulmonary edema who were virtually "drowning" in their own pulmonary fluids. In refractory HF with anasarca, hyperchloremic acidosis was induced to potentiate the effect of intravenous mercurials. Acetazolamide (carbonic anhydrase inhibitor) and ammonium chloride tablets were given to produce a state of hyperchloremic acidosis. In pursuant years, loop diuretics (ethacrynic acid, furosemide), which act on the thick ascending loop of Henle, were introduced to block renal absorption of sodium and water. New loop diuretics (bumetanide, torsemide) have been added and, alone or in combination with thiazides, were added to the arsenal in the management of all classes of HF, but especially of class IV failures. A most effective diuretic combination is the use of a loop diuretic and metazolone, a thiazide that also acts on the proximal tubule, but has a longer duration of action. In the 1970s and 1980s, powerful oral and parenteral inotropic agents were developed to increase CO, but their use was associated with greater and earlier cardiac mortality, primarily due to sudden arrhythmic death. In the last decade of the 20th century, the role of neurohormonal system activation in HF became apparent. Activation of these systems serves to maintain arterial pressure in order to preserve coronary and cerebral perfusion. This process occurs at the cost of increasing ventricular afterload, heart rate, and myocardial energy expenditure. To prevent this cycle, ACEIs were subsequently added to HF management. The roles of nitric oxide and atrial natriuretic peptide in HF have also been observed and are under investigation. Recent molecular and genetic breakthroughs have elucidated the cellular role in cardiovascular disease. Genetic mapping and typing of specific HF and atherosclerotic risk types are also underway. Reduction of the cardiovascular risk factors hypertension, obesity, hyperlipidemia, homocysteine level, and tobacco use are critical in prevention and treatment of HF. Other measures include prevention of infection (prophylactic vaccination against influenza and pneumococcosis) and treatment of underlying sleep apnea.
4. a. reducing circulating volume
b. reducing cardiac filling pressures
c. decreasing neurohormonal activation
a. loop diuretic
b. thiazide diuretic
c. potassium-sparing diuretic
Throughout the history of HF therapy, only diuretics and salt reduction have remained key elements in management. An increase in LV end-diastolic volume is the hemodynamic abnormality resulting from HF that directly affects symptoms and is highly predictive of the risks, degree of decompensation, arrhythmia, and mortality. (2) Effective diuretic therapy reduces circulating volume and cardiac filling pressures through fluid elimination. By reducing venous return to the right side of the heart, the pulmonary artery, and the left ventricle, both preload and afterload are attenuated. The reduction in intracardiac volume reduces heart size and improves contractile force. (3) Diuretics differ in their mode of action and their pharmacodynamic and pharmacokinetic properties. Loop diuretics (furosemide, bumetanide, torasemide) inhibit sodium and chloride reabsorption in the thick ascending loop of Henle. Peak effects occur within 1 to 2 hours and last 6 to 8 hours (a rebound sodium retention occurs after 12-24 hours). Newer loop diuretics have greater bioavailability and longer half-life. Thiazide and thiazide-like agents (chlorothiazide, hydrochlorothiazide, metolazone) act on the distal convoluted tubule. Thiazides have a gradual onset of action, peaking at 2 to 4 hours and lasting 12 to 48 hours. Thiazides are suited for long-term therapy in mild HF, but they lose their efficacy when glomerular filtration rates are less than 30 mL/min. Metolazone is a thiazide with a long-lasting effect, 24 hours. Spironolactone, an aldosterone-receptor blocker, helps to increase diuresis in patients resistant to combined loop diuretics and ACEI therapy. These potassium-sparing diuretics (spironolactone, amiloride, triamterene) act on the distal nephron and collecting duct. These are prescribed in combination with loop or thiazide agents to increase diuresis in patients resistant to the other diuretics and also to prevent electrolyte disturbances.
To avoid adverse effects of diuretics, large doses should be avoided once compensation has been achieved. Also, regular examinations should be done to assess fluid loss, morning weights should be noted daily at home, and electrolyte levels, renal function, and acid-base balance should be monitored. Prolonged use of diuretics may at times affect blood lipid and glucose levels in diabetic patients and may precipitate gout. These effects occur infrequently and can be managed without compromising HF therapy.
It is noteworthy that although CHF cannot be managed properly without strict attention to salt intake and fluid elimination with diuretics, very little is reported in the recent literature regarding the use and critical role of diuretics in HF therapy.
6. f. all of the above
The early adaptive neurohormonal activity that initially improves cardiac function soon becomes maladaptive when cardiac demands are not reduced. With the onset of HF, sodium and water retention occur in response to a diminished perfusion pressure sensed by receptors in the kidney. Numerous endogenous neurohormonal "rescue" systems, including the RAAS, cardiac and endothelial natriuretic peptides, and the sympathetic and the hypothalamic systems, are activated early in HF. This is followed by the release of vasoactive substances, namely, norepinephrine and the natriuretic peptides: A type from the atria, B type from the ventricles, and C type from vascular endothelium. Initially these are adaptive neurohormones that support a reduced CO. The natriuretic peptides are released in response to the increase in LV filling pressure and volume and cause a decrease in peripheral vascular resistance and suppression of the RAAS and release of endothelin. The short-term effect of these support systems serves to minimize and reverse the pathologic hemodynamic changes of HF. When cardiac demands are not reduced and intrinsic myocardial cell function is not improved or reversed, these support systems become maladaptive and HF progresses.
Activation of the adrenergic system triggers the release of catecholamines, which stimulate contractility, heart rate, and blood pressure and promote myocyte hypertrophy. Cardiac performance is initially improved; however, myocardial deterioration follows when HF persists. Persistent adrenergic activation becomes deleterious because it promotes ischemia, tachyarrhythmias, and myoctye damage and increases myocardial energy expenditure.
Activation of the RAAS releases renin from the juxtaglomerular cells of the kidney. Renin triggers renal retention of sodium and water, which in turn increases plasma volume and preload. Renin also triggers conversion of angiotensin I to angiotensin II--a powerful vasoconstrictor that increases ventricular afterload, myoctye hypertrophy, remodeling, apoptosis, and secretion of aldosterone.
Activation of the hypothalamic-neurohypophyseal system promotes vasoconstriction (due to the release of vasopressin) and increases sodium and water retention is addition to the expanded intravascular volume due to RAAS activation. The results are that a greater venous return loads an inefficient cardiac pump, and the increase in preload augments the stroke volume. The ejection fraction, which measures the contractile behavior of the heart during systole, is sensitive to the afterload. Therefore the low ejection fraction of the failing left ventricle's initial preload when augmented by a greater venous volume is then the ejection fraction of a larger end-diastolic volume, which as a result temporarily provides an adequate output (even though the ejection fraction is low).
The early use of diuretics and sodium restriction reduce peripheral volume and preload, which lowers cardiac work and thus improves cardiac function. Neurohormonal activity is reduced as a result. (4)
Summary
Dietary sodium restriction and diuretics are basic requirements in the treatment of CHF. The reduction in pulmonary venous congestion following the use of diuretics leads to a rapid improvement in dyspnea, promotes natriuresis without direct positive inotropic effects, and does not reflexively activate the neuro-endocrine system. The recent literature has been replete with reports on the treatment of HF. However, very little has been said about the importance and the methods of use of diuretics in HF. Treatment of HF cannot succeed without regard for the role of the sodium ion in HF.
There are nearly 5 million cases of HF in the United States. More than 500 000 new cases are diagnosed each year. Hospital discharges and deaths due to HF have increased more than 100% in the past 2 decades with a 5-year mortality rate close to 50%. (5) Since the leading cause of HF in Western countries is ischemic heart disease, aggressive therapy to halt progression of coronary atherosclerosis can have a major impact on controlling and often curing HF.
ACKNOWLEDGMENT
Supported in part by a grant from the Applebaum Foundation in loving memory of Joseph Applebaum.
REFERENCES
(1.) Lemberg L. Digitalis in congestive heart failure: fact or fancy. Arch Intern Med. 1978;128:451-452.
(2.) Fonarow GC. Phamacologic therapies for acutely decompensated heart failure. Rev Cardiovasc Med. 2002;3[suppl 4]:18-27.
(3.) Johnson W, Omland T, Hal C, Lucas C, et al. Neurohormonal activation rapidly decreases after intravenous therapy with diuretics and vasodilators for class IV heart failure. J Am Coll Cardiol. 2002;39:1623-1629.
(4.) Reyes AJ. Diuretics in the treatment of patients who present congestive heart failure and hypertension. J Hum Hypertens. March 2002;16[suppl 1]:104-113.
(5.) American Heart Association. 2002 Heart and Stroke Statistical Update. Dallas, Tex: American Heart Association; 2001.
SELECTED REFERENCES
Dormans TP, Gerlag PG, Russel FG, Smits P. Combination diuretic therapy in severe congestive heart failure. Drugs. 1998;55(2):165-172.
Follath F. Do diuretics differ in terms of clinical outcome in congestive heart failure? Euro Heart J. 1998;19(suppl P):5-8.
Futterman LG, Lemberg L. Heart failure: update on treatment and prognosis. Am J Crit Care. 2001;10(4):285-293.
Lemberg L. The management of congestive heart failure: a perspective. Mercy Med. 1984;3(1):10-18.
Pavia SV, Galbraith AJ. Therapy for cardiac failure: treatments old and new. Med J Austr. 1999;171:265-271.
Ravnan SL, Ravnan MC, Deedwania PC. Pharmacotherapy in congestive heart failure: diuretic resistance and strategies to overcome resistance in patients with congestive heart failure. Congest Heart Fail. 2002;8(2):80-85.
Reprint requests: Louis Lemberg, MD, University of Miami School of Medicine, Division of Cardiology (1)-39), P. O. Box 016960, Miami, FL 33101.
COPYRIGHT 2003 American Association of Critical-Care Nurses
COPYRIGHT 2003 Gale Group