Key Words: Substance abuse; Opioid dependence; Buprenorphine maintenance
INTRODUCTION
Substance users frequently present to primary-care physicians for care of medical complications related to their drug use as well as for help in initiating substance abuse treatment (1). Although primary-care physicians may feel comfortable addressing medical issues, they are often uncertain how to address patient needs concerning their addiction (2, 3). When physicians are aware of treatment options, they will commonly refer patients to substance abuse treatment programs in their communities. Currently, a standard treatment for opioid (e.g., heroin)-dependent patients is methadone maintenance (4). However, this treatment is often inaccessible due to high demand and limited program availability (1, 4). Furthermore, methadone maintenance is currently restricted to licensed drug treatment programs and is not generally available in primary-care settings (4).
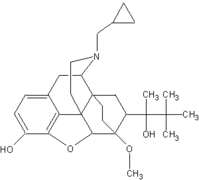
Prior research has identified the primary-care setting as a potential site for treating heroin dependence (5, 6). Although one study suggests that "stable" long-term methadone maintenance patients may be successfully transferred to methadone maintenance provided in a primary-care setting, this approach has not been studied for addicts admitted "off the street" (6). A newer experimental alternative to methadone, buprenorphine, has been demonstrated to be effective for the treatment of opioid dependence when administered daily as an opioid maintenance agent in traditional drug treatment settings (7, 8). Buprenorphine has also been demonstrated to be effective for the treatment of opioid dependence when administered every other day but has not been evaluated in primary-care settings (9). Buprenorphine maintenance may be uniquely suited to primary-care settings given that it is longer acting and easier to withdraw than methadone (9, 10).
Thus, we conducted a pilot study to assess the feasibility of a thrice weekly buprenorphine maintenance for heroin dependence utilizing a protocol administered by primary-care providers in a primary-care setting.
METHODS
Patient Recruitment and Treatment Setting
Heroin-dependent patients were identified for this study through a methadone maintenance waiting list and word-of-mouth referrals. Potential subjects were referred for primary-care-based buprenorphine maintenance to the Central Medical Unit (CMU), a licensed, freestanding primary-care clinic. The vast majority (approximately 90%) of patients seen at the clinic are individuals enrolled in the drug treatment programs affiliated with the Yale University Substance Abuse Treatment Unit (11). The CMU provides a full range of routine primary-care services for patients including health maintenance, chronic disease (e.g., hypertension, diabetes, HIV disease) management, and urgent care. Primary-care physicians and nurse practitioners who staff the CMU were the primary providers of drug treatment services for patients enrolled in this study.
Eligibility Criteria
Subjects were required to meet the following inclusion criteria: current opioid dependence DSM-III-R criteria) (12), opioid-positive urine screen, and ability to comply with the outpatient program (e.g., had a place to live, able to be transported to and from the program). Exclusion criteria included current cocaine use (within past month by history or a positive urine screen for cocaine), current diagnosis of other drug or alcohol dependence (other than tobacco; (DSM-III-R criteria) (12), complex medical "comorbidity" (e.g., major cardiovascular, renal, or gastrointestinal disease), pregnancy, or a major psychiatric disorder (e.g., psychosis, suicidality, schizophrenia, major depression).
Study Design
This was a non-blinded, open-labeled pilot study of buprenorphine maintenance for the treatment of opioid dependence. Enrolled patients were provided 6 months (26 weeks) of primary-care-based buprenorphine maintenance in the CMU. Patients attended the clinic three times per week (Table 1).
Buprenorphine administration occurred in two phases. During the first phase (week 1), "buprenorphine stabilization," buprenorphine was begun at a dose of 2 mg on day 1. On days 2-5 the dose was gradually increased: 4 mg (day 2), 8 mg (day 3), 16 mg (day 4), and 24 mg (day 5). The second phase, "buprenorphine maintenance" (weeks 2-26), buprenorphine was administered initially at a dose of 16 mg on Monday and Wednesday and 24 mg on Friday. Early in the study the Friday dose was empirically increased to 32 mg when patients indicted that 24 mg did not sufficiently control opioid withdrawal symptoms for the full duration between doses.
For this study, buprenorphine was prepared in a sublingual formulation by a study pharmacist. One multidose vial (30 cc) was dispensed to the primary-care clinic and was stored in a double-locked pharmacy cabinet accessible only to the clinicians caring for these patients. Clinicians dispensing buprenorphine observed the patients who were instructed to hold it under their tongue for 5 minutes to assure adequate absorption. All medication dispensing was document on "proof-of-use" sheets, copies of which were returned to the pharmacist along with requests for additional medication.
Following an initial 1-hour "new patient" visit on week 1, the protocol called for primary-care providers to meet with each patient weekly for a brief (e.g., 20 minutes) "follow-up visit." The content of these follow-up sessions included a review of the patient's recent drug use, withdrawal symptoms, medication issues, psychosocial issues, and a discussion of strategies to enhance abstinence. In addition, patients met in a weekly, 1-hour semistructured group session utilizing a facilitated "self-help" approach in which patients could learn from each other concerning strategies to promote abstinence. Psychiatric consultation was available if needed.
Patients who completed the study were offered the opportunity to transfer to methadone maintenance or other suitable treatment programs.
Study Outcomes
The primary outcomes of interest for this study were retention in treatment and urine toxicology for opioids. Patients were discharged from this study if they missed medication on two successive occasions or if they failed to attend the weekly visit with their primary-care provider. Urine toxicology screens were performed three times a week for the duration of the study.
RESULTS
Patient Characteristics
Seven heroin-dependent patients were enrolled in this pilot study: six (86%) were male, the mean age was 27 years (range 21-39 years old), five (71 %) were never married, four (57%) completed high school, and four (57%) were employed full-time or part-time. They reported a mean duration of 2.4 years of heroin use.
Treatment Outcomes
Five (71%) patients completed the study and two (29%) were removed from the study (Table 2). Patient 5 was removed in week 9 following a suicidal gesture and patient 6 was removed from the study in week 7 after failing to show up for scheduled appointments.
Urine toxicology results for each of the 6 months that patients were enrolled in treatment are displayed in Table 2. Of the five patients who completed treatment, four (patients 1-4) were noted to have mostly negative urine toxicology screens during the last 3 months of treatment. One patient (patient 7) had continued positive urines for opioids throughout the study. Self-reported opioid use declined significantly from a pretreatment mean of 31.0 bags of heroin per week to an overall mean of 1.3 bags per week while enrolled in the study (ANOVA: F = 10.5, df = 1, p < .01).
Buprenorphine was well tolerated by all patients. No significant adverse effects were reported. Of the five patients who completed the study, four were transferred to a methadone maintenance program and one enrolled in a naltrexone maintenance program.
DISCUSSION
Reasons to evaluate primary-care settings as an alternative to traditional drug maintenance programs for treatment of opioid dependence include 1) expanding the availability of drug treatment through utilization of existing primary-care clinics, 2) improving access to drug treatment services, and 3) integrating drug treatment into the evolving primary-care system, especially in an era of health-care reform. Prior research has suggested that primary-care-based interventions may be effective for managing opioid, alcohol, and nicotine dependence (5, 6, 13, 14).
In the case of heroin dependence, the primary-care setting may decrease some of the potentially "negative" or countertherapeutic aspects of opioid maintenance programs, including opportunities for interaction with patients who continue to use illicit drugs. For some opioid-dependent patients, the primary-care setting may be preferred because it is less stigmatizing and easier to access. In Novick's study of "medical" methadone maintenance, subjects reported that primary-care-based maintenance offered a more professional atmosphere than traditional drug treatment settings (6). Finally, integrating substance abuse treatment and primary care may enhance the access of this population to needed medical services such as preventive health care and the management of medical problems associated with drug use such as HIV (human immunodeficiency virus) infection.
One issue affecting the potential effectiveness of primary-care-based opioid maintenance treatment involves the level of psychosocial services available in this setting. In general, primary-care settings provide only limited psychosocial services and more intensive or specialized drug counseling may not be feasible in this setting. Primary-care-based maintenance programs will only be able to provide brief medically focused counseling to patients. While this level of counseling is within the wide range of variability of psychosocial services offered to patients in methadone maintenance programs (4), more intensive services may be associated with improved outcomes (e.g., reduced illicit drug use, improved functional status) (15). It will be important to determine whether specific subpopulations such as patients without major baseline psychopathology or concurrent dependence on other substances might benefit from the less intensive services offered in a primary-care setting (16).
Concerning limitations, this pilot study was designed primarily to demonstrate feasibility of the protocol described. Thus, the number of subjects is small and there is no "control" (e.g., "usual care") group. Although our primary-care clinic - the Central Medical Unit - is an ideal setting for testing innovative drug treatment strategies, future research will need to include patients cared for in a variety of community-based primary-care settings. Primary-care clinicians would need to develop strategies for managing the behavioral problems (e.g., noncompliance with scheduled visits and continued illicit drug use) often seen with drug dependence. Appropriate medication ordering, storage and dispensing protocols would also need to be developed.
The thrice weekly buprenorphine regimen will require more detailed evaluation to determine its efficacy (versus daily buprenorphine) and to determine the most appropriate dosing regimen. For example, the 32-mg dose administered on Friday was arrived at empirically in this study, rather than on the basis of detailed evaluations of the pharmacological effects in individual patients. One study does suggest that higher doses (e.g., 32 mg) of buprenorphine appear to be both well tolerated and long lasting in terms of the subjective and physiologic effects (17). Finally, it will be important to demonstrate that this approach could be extended beyond 6 months as is usually required in this population.
This study suggests that primary-care-based opioid maintenance using buprenorphine may be a feasible approach to treating opioid dependence. Our 6-month retention rate and urine toxicology results compare favorably to retention data from traditional methadone maintenance settings (4). These results need to be verified in large studies that randomly allocate patients to primary care and "traditional drug treatment" settings. Future studies of primary-care-based drug treatment strategies also need to examine the cost effectiveness of this approach if it is to be thoughtfully considered as an alternative to traditional drug treatment programs.
REFERENCES
[1.] O'Connor, P. G., Selwyn, P. A., and Schottenfeld, R. S., Medical care for injection-drug users with human immunodeficiency virus infection, N. Engl. J. Med. 331:450-459 (1994). [2.] Policy Report of the Physician Consortium on Substance Abuse Education, Department of Health and Human Services, Rockville, Maryland, 1991. [3.] Jaffe, J. H., Drug addiction and drug abuse, in Goodman and Gilman's: The Pharmacological Basis of Therapeutics, 8th ed. (A. G. Gilman, T. W. Rall, A. S. Nies, and P. Taylor Eds.), Pergamon Press, New York, 1990, pp. 522-573. [4.] Ball, J. C., and Ross, A., The Effectiveness of Methadone Maintenance Treatment, Springer-Verlag, New York, 1991. [5.] O'connor, P. G., Waugh, M. E., Carroll, K. M., et al., Primary care-based ambulatory opioid detoxification: The results of a clinical trial, J. Gen. Intern. Med. 10(5):255-260 (1995). [6.] Novick, D. M., Pascarelli, E. F., Joseph, H., et al., Methadone maintenance patients in general medical practice: A preliminary report, JAMA 259(22):3299-3302 (1988). [7.] Mello, N. K., and Mendelson, J. H., Buprenorphine suppresses heroin use by heroin addicts, Science 207:657-659 (1980). [8.] Johnson, R. E., and Fudala, P. G., Development of buprenorphine for the treatment of opioid dependence, Buprenorphine: An Alternative Treatment for Opioid Dependence (J. Blaine, Ed.), NIDA Research Monograph Series 121, National Institute on Drug Abuse, Rockville, Maryland, 1992, pp. 120-141. [9.] Amass, L., Bickel, W. K., Higgins, S. T., et al., Alternate-day dosing during buprenorphine treatment of opioid dependence, Life Sci. 54:1215-1228 (1994). [10.] Bickel, W. K., Stitzer, M. L., Bigelow, G. E., et al., Buprenorphine: Dose related blockage of opioid challenge effects in opioid dependent humans, J. Pharmacol. Exp. Ther. 247:47-53 (1988). [11.] O'Connor, P. G., Molde, S., Henry, S., et al., Human immunodeficiency virus infection in intravenous drug users: A model for primary care, Am. J. Med. 93:382-386 (1992). [12.] American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders, 3rd ed., American Psychiatric Association, Washington, D.C., 1987. [13.] Hughes, J. R., Guest, S. W., Keenan, R. M., et al., Nicotine vs. placebo gum in general medicine practice, JAMA 261:1300-1305 (1989). [14.] Fiore, M. C., Jorenby, D. E., Baker, T. B., et al., Tobacco dependence and the nicotine patch: Clinical guidelines for effective use, JAMA 268:2687-2694 (1992). [15.] McLellan, A. T., Arndt, I. O., Metzger, D. S., et al., The effects of psychosocial services in substance abuse treatment, JAMA 269:1953-1959 (1993). [16.] Rounsaville, B. J., Weismann, M. M., Crits-Cristoph, K., et al., Diagnosis and symptoms of depression in opiate addicts: Course and relationship to treatment outcome, Arch. Gen. Psychiatry 39:151-156 (1982). [17.] Walsh, S. L., Preston, L. K., Stitzer, M. L., Cone, E. J., and Bigelow, G. E., Clinical pharmacology of buprenorphine: Ceiling effects at higher doses, Clin. Pharmacol. Ther. 55:569-580 (1994).
COPYRIGHT 1996 Taylor & Francis Ltd.
COPYRIGHT 2004 Gale Group