Calcitriol
Vitamin D is a fat-soluble steroid hormone precursor that contributes to the maintenance of normal levels of calcium and phosphorus in the bloodstream. Strictly speaking, it is not a vitamin since human skin can manufacture it, but it is referred to as one for historical reasons. It is often known as calciferol. more...
Forms of Vitamin D
- Vitamin D1: molecular compound of ergocalciferol with lumisterol, 1:1
- Vitamin D2: ergocalciferol or calciferol (made from ergosterol) also called
- Vitamin D3: cholecalciferol (made from 7-dehydrocholesterol)
- Vitamin D4: 22,23-dihydroergocalciferol
- Vitamin D5: sitocalciferol (made from 7-dehydrositosterol)
Overview
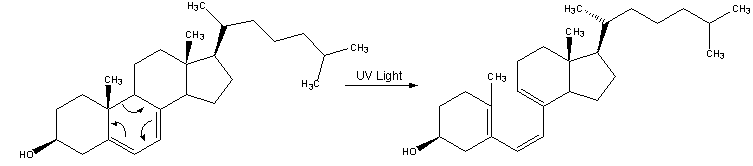
Vitamin D3, also known as cholecalciferol, is the natural human form of vitamin D. It is made in the skin when cholesterol via 7-dehydrocholesterol reacts with ultraviolet light in the skin. Ultraviolet light (UVB, which is wavelengths 290 to 315 nm), found in sunlight when the sun is high enough above the horizon for UVB to penetrate the atmosphere, is responsible for the production of cholecalciferol. Up to 20,000 IU can be made in the skin after one minimal erythemal dose of exposure, or until the skin just begins to turn pink. Vitamin D2 is derived by irradiating fungi to produce ergocalciferol. Ergocalciferol does not naturally occur in the human body unless it is added by supplementation.
In certain parts of the world, particularly at higher latitudes, total vitamin D input is usually not sufficient, especially in the winter, thus the recent concern about widespread vitamin D deficiency. To help prevent this possibility, foods such as milk may be fortified with vitamin D2 or vitamin D3, but milk only contains 100 IU per glass, 1/200 as much as is made after 15 minutes of sunbathing at solar noon in the summer. A severe deficiency of vitamin D leads to rickets in children, which is a softening of the bones owing to faulty mineralization, and a similar condition in adults, osteomalacia. Recent medical studies also associate vitamin D deficiency with everything from most forms of cancer, to heart disease, depression, diabetes, hypertension, autoimmune diseases, periodontal disease, and even obesity.
Cholecalciferol is transported to the liver where it is hydroxylated to calcidiol or 25-hydroxy-vitamin D, the storage form of the vitamin. A blood calcidiol level is the only way to determine vitamin D deficiency; levels should be between 40 and 60 ng/ml (100 to 150 nMol/L) for optimum health.
The most active form of the vitamin is calcitriol, a potent steroid hormone. Calcitriol is synthesized from calcidiol in the kidneys to perform its endocrine function of maintaining the calcium economy. Calcitriol binds to a transcription factor which then regulates gene expression. The outcome is the maintenance of calcium and phosphorus levels in the bone and blood with the assistance of parathyroid hormone and calcitonin.
Read more at Wikipedia.org