Study objectives: Direct current (DC) shocks to the heart cause morphologic and functional myocardial damage. Previous studies have suggested that acute DC shock injury is free radical mediated and that the administration of antioxidant enzymes superoxide dismutase and catalase can reduce the level of DC shock-induced free radicals. Angiotensin-converting enzyme (ACE) inhibitors are clinically used drugs that may scavenge free radicals or reduce free radical generation. The objective of our study was to determine whether the ACE inhibitor captopril lowers free radicals after DC shocks.
Design: In six open-chest dogs, we administered 100-J DC shocks to the epicardium, before and after administration of captopril, 3 mg/kg. We used electron paramagnetic resonance measurements of arterial and coronary venous ascorbate free radical (AFR) as a real-time marker of free radical generation (total oxidative flux).
Measurements and results: Captopril resulted in a significant lowering of coronary venous AFR concentration: the peak rise in AFR after 100-J shocks was 17.3 [+ or -] 3.4% (mean [+ or -] SEM before captopril vs 3.2 [+ or -] 4.0% after captopril; p [is less than] 0.05).
Conclusions: Captopril lowers coronary venous AFR concentration after high-energy epicardial shocks. (CHEST 1999; 116:484-48 7)
Key words: angiotensin-converting enzyme inhibitors; captopril; cardioversion; defibrillation; free radicals
Abbreviations: ACE = angiotensin-converting enzyme; AFR = ascorbate free radical; DC = direct current; EPR = electron paramagnetic spin resonance
Both transthoracic and epicardial direct current (DC) countershocks have been demonstrated to cause transient and permanent myocardial damage.[1,2] However, the mechanism of this DC shock injury has been uncertain. There is considerable evidence that free radicals play a major role in DC shock-induced myocardial injury. The passage of a current through a physiologic buffer solution has been shown to result in the generation of free radicals.[3] DC countershocks to the heart have been shown to result in the production of free radicals.[4] Caterine et al[5] have shown that free radical generation is primarily dependent on the peak energy delivered and that it is not dependent on the presence or absence of ventricular fibrillation.
In models of myocardial ischemia and reperfusion, in vivo protection against free radical injury is obtained from free radical scavengers such as superoxide dismutase and catalase. However, these endogenous antioxidant enzymes are not used clinically. In contrast, angiotensin-converting enzyme (ACE) inhibitors are a class of drugs that are widely used in the treatment of hypertension and congestive heart failure. Some studies have suggested that ACE inhibitors can act as free radical scavengers.[6,9] For example, Przyklenk and Kloner[8] have shown that administration of ACE inhibitors improved recovery of contractile function in "stunned" canine myocardium, a phenomenon associated with the production of oxygen radicals. Because free radicals are generated by DC shocks to the heart, ACE inhibitors might scavenge such radicals or inhibit their production; this may be a clinically applicable method of reducing defibrillation injury.
Recently we described an electron paramagnetic spin resonance (EPR) method that allows real-time, ex vivo quantification of free radical generation.[10] The method uses the ascorbate free radical (AFR) concentration in coronary venous blood as a real-time marker of myocardial free radical generation. The AFR has a low reduction potential, thereby facilitating the oxidation of ascorbate by almost all oxidizing radicals generated by biological systems.[11-15] For example, free radicals such as lipid peroxyl radicals can be eliminated by vitamin E in the lipid membrane, but this results in the formation of the vitamin E radical. This radical in turn can be repaired by vitamin C in the aqueous phase resulting in AFR production.[11] The AFR is a resonance-stabilized radical that is easily detectable by EPR.
In this study, we used this new method in a series of experiments undertaken to test the hypothesis that the ACE inhibitor captopril can act as a free radical inhibitor or scavenger after epicardial DC shocks, thereby lowering the postshock coronary venous concentration of AFR.
MATERIALS AND METHODS
Animal Preparation
An open-chest model previously described was used for this study.[10] Adult mongrel dogs of either gender were used. Body weights ranged from 20 to 30 kg. Sedation and anesthesia were induced with IV fentanyl/droperidol, 1.2 mg/60 mg, and sodium pentobarbital, 400 mg. The animals underwent endotracheal intubation and were placed on a volume-cycled respirator. Routine monitoring of blood gases was performed to maintain physiologic conditions. Intravascular access was obtained bilaterally via the internal jugular veins, femoral arteries, and femoral veins. Both arterial BPs and ECGs were monitored throughout the experiments. A left lateral thoracotomy was performed in the fifth intercostal space, and the heart was suspended in a pericardial cradle. The left atrial appendage was retracted to allow for adequate exposure of the coronary sinus. A catheter was advanced from the left internal jugular vein into the coronary sinus and secured with a ligature in the distal great cardiac vein. A venous-venous shunt was fashioned between the great cardiac vein and the right femoral vein. Heparin was administered in the IV fluid and the indwelling cannulas and tubing to prevent clotting.
EPR Methods
The measurement of AFRs has been previously described and validated as a measure of total oxidative stress.[15 Our method of AFR measurement has previously been described in detail.[10] Briefly, the EPR spectra of the AFR were obtained using a spectrometer (Varian E4 spectrometer; Varian Associates; Palo Alto, CA) with a transverse mode110 cavity and an aqueous flat cell. Scans were collected serially on blood being continuously withdrawn from either the great cardiac vein or the femoral artery. An infusion pump was used to circulate the sample through the spectrometer and return it to the animal. In this fashion, blood could be scanned for AFRs within 7 s of leaving the animal. The following instrument settings were used for all studies because they provide the largest AFR signal: nominal power, 40 mW; modulation amplitude, 0.63 gauss; time constant, 1 s; and scan rate, 1 G/24 s. To amplify the endogenous AFR signal, which normally is too low in canine blood for detection by EPR, a 1-g bolus of ascorbate was given followed by an IV infusion of ascorbate (8 to 30 mg/min). The AFR EPR signal is partially saturated at 40 mW nominal power. Appropriate corrections in ascorbate infusion rates were made to achieve steady-state AFR concentrations in the femoral artery and coronary venous blood. The femoral artery AFR signal is higher than the coronary venous signal and must be stable to allow meaningful interpretation of rises in the coronary venous signal, which indicates increased myocardial radical generation.[10]
The concentration of the AFR was determined from the signal height of the AFR EPR spectrum after calibration using double-integration techniques and 3-carboxy peroxyl as the standard. All signal heights were normalized to the full gain of the instrument, [10.sup.5]. In our experimental conditions, after accounting for saturation effects, 1 mm of signal height corresponds to 0.0734 nmol/L AFR.[16]
Protocol
In six dogs, the effect of DC shocks on the generation of AFR was studied. After obtaining baseline (steady-state) AFR measurements from the femoral artery and great cardiac vein, an initial 100-J DC shock was delivered to the epicardium of the beating heart. All shocks were administered using a damped sine waveform defibrillator (Datascope MD2-J; Datascope Corp; Paramus, NJ). All shocks were administered via hand-held electrode paddles cradling the heart.
After the shock, we monitored AFR signals for 10 min. Typically, the coronary venous AFR signal briefly fell during the first 1 to 2 min after shocks, probably reflecting the expected transient postshock hypotension and bradycardia.[17] Because this coronary venous AFR fall is artifactual, we have omitted AFR data from the first 2 min after each shock.
After the postshock monitoring was completed, we prepared for the second shock. We first verified that the arterial AFR signal was unchanged. If necessary, we adjusted the ascorbate infusion rate and monitored the arterial AFR signal further until a steady-state arterial signal was regained before administering the second shock.
Once the AFR monitoring was completed after the first 100-J shock and a steady-state was reestablished, an IV infusion of the ACE inhibitor captopril, 3 mg/kg, was started 15 min before delivering the second 100-J DC shock. The second shock was administered after one half of the total captopril dose had been infused, and the infusion was continued through the 10-min postshock monitoring period. The ACE inhibitor dose was based on studies of the cardioprotective effects of ACE inhibitors by other investigators, in settings of postischemic stunned myocardium.[18-21] After the second 100-J shock, the AFR level was again measured.
Statistical Analysis
Analysis of the AFR concentration generated by the shocks in the absence or presence of captopril was done by repeated measures of the analysis of variance with both the intervention and time as repeated factors. Post hoc comparisons of intervention (captopril) vs no intervention (no captopril) at each point were done by using Bonferroni's method (p [is less than] 0.05). BP comparisons before and after captopril were done by using the Student's paired t test. All results are reported as mean [+ or -] SEM.
RESULTS
After the initial 100-J shock, the mean AFR concentration in coronary venous blood rose from 7.8 [+ or -] 0.2 nmol/L at baseline to a peak of 9.1 [+ or -] 0.3 nmol/L (17.3 [+ or -] 3.4% rise). After the administration of captopril and a second 100-J shock, the AFR concentration rose minimally, from 7.6 [+ or -] 0.4 nmol/L to 7.8 [+ or -] 0.4 nmol/L (3.2 [+ or -] 4.0% rise; p [is less than] 0.05 compared with the AFR rise induced by the initial precaptopril shock). The rise in AFR generation was significantly higher after the first 100-J shock compared with the second 100-J shock that followed captopril (Fig 1).
[Figure 1 ILLUSTRATION OMITTED]
After the first 100-J shock (given before the administration of captopril), mean arterial pressure fell from 90 [+ or -] 10 mm Hg to 76 [+ or -] 10 mm Hg (p [is less than] 0.05). After the administration of captopril and the second shock, the arterial pressure fell from 69 [+ or -] 8 mm Hg to 66 [+ or -] 8 mm Hg (not significant).
DISCUSSION
In this study, we have shown that the shock-induced increase in coronary venous AFR concentration was virtually abolished by the administration of captopril before delivering high-energy epicardial shocks.
Myocardial injury from DC shocks (defibrillation injury) is a well-established phenomenon, resulting from both transthoracic and epicardial shocks.[1,2] The nature of the morphologic injury is patchy and seems to be related to the amount of current that traverses the myocardium.[22] Functional injury (contraction abnormalities, atrioventricular block) has been reported.[1,23] Transesophageal echocardiographic studies show atrial dysfunction ("atrial stunning") after elective cardioversion for atrial fibrillation.[24]
Trouton et al[4] have postulated that this damage may be related to the observed mitochondrial dysfunction. Mitochondria are sources of oxygen radicals via leakage from the electron transport chain. Any damage to mitochondria may result in additional seepage of electrons from the chain, resulting in superoxide and hydrogen peroxide production.[25]
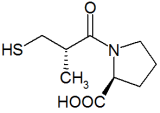
Previous work in our laboratory has shown that the increase of AFR after epicardial shocks is energy dependent, and it can be attenuated by the administration of superoxide dismutase and catalase.[5] Snperoxide dismutase and catalase are not used clinically, whereas ACE inhibitors are used clinically and may also have free radical scavenging or inhibitory effects. Przyklenk and Kloner[8] noted that ACE inhibitors improved contractile function in stunned myocardium, a phenomenon in which free radicals have been implicated,[26-29] by as much as five to seven times. Studies by Westlin and Mullane[21] have demonstrated, both in vitro and in vivo, that captopril scavenges superoxide radicals and improves myocardial dysfunction. Chopra et al[7] found that the ACE inhibitors captopril, epicaptopril, and zofenopril significantly scavenged free radicals. Although some studies have suggested that the sulfhydryl portion of the ACE inhibitors is required for the optimal free radical scavenging effect,[7,21,30] other studies[6,9,31] have found that ACE inhibitors both with and without the sulfhydryl moiety act as effective free radical scavengers. The ACE inhibitor we used, captopril, contains a sulfhydryl group.
We have previously shown that in the absence of antioxidant enzymes, repeated shocks at the same energy generate equivalent amounts of AFRs.[26] Thus, the fall in ascorbate generation we observed after administration of captopril and a second 100-J shock cannot simply be ascribed to a nonspecific effect of repeated shocks, but must be caused by the scavenging or inhibiting effects of captopril.
The dose of captopril we chose was based on the work of previous investigators who have studied the cardioprotective effects of ACE inhibitors.[8,18-21] The captopril dose we used, 3 mg/kg IV, is much higher than doses typically used in patients. Whether or not lower doses more analogous to clinical usage would have the same radical-lowering effect is not established by this study.
One limitation of this study is that we did not attempt to measure the functional consequences of free radical generation; we did not demonstrate that the reduction of the shock-induced rise in free radicals, which occurred because of the administration of captopril, was accompanied by a preservation of, for example, myocardial contractility. Whether or not captopril is functionally cardioprotective in the setting of DC shocks remains to be established.
ACE inhibitors are already shown to be useful drugs in the treatment of congestive heart failure and hypertension. The present results cannot be directly extrapolated to the clinical setting, but they do suggest that lowering of free radical concentration may already be clinically possible by use of captopril. Further studies are needed to determine whether captopril may be used preemptively in the clinical setting of defibrillation or cardioversion to prevent free radical damage.
ACKNOWLEDGMENT: We acknowledge the technical assistance of Robin Smith and the statistical expertise of Bridget Zimmerman, PhD. IV captopril was generously donated by Bristol-Myers Squibb Co.
REFERENCES
[1] Kerber RE, Martins JB, Gascho JA, et al. Ether of direct-current countershocks on regional myocardial contractility and perfusion. Circulation 1981; 63:323-332
[2] Dahl CF, Ewy GA, Warner ED, et al. Myocardial necrosis from direct current countershock: effect of paddle electrode size and time interval between discharges. Circulation 1974; 50:956-961
[3] Jackson CV, Mickelson JK, Stinger K, et al. Electrolysis-induced myocardial dysfunction: a novel method for the study of free radical mediated tissue injury. J Pharmacol Methods 1986; 15:305-320
[4] Trouton TG, Allen JD, Yong LK, et al. Metabolic changes and mitochondrial dysfunction early following transthoracic countershocks in dogs. Pacing Clin Electrophysiol 1989; 12:1827-1834
[5] Caterine MR, Spencer KT, Pagan-Carlo LA, et al. Direct current countershocks generate free radicals: an electron paramagnetic resonance study. J Am Coll Cardiol 1996; 28:1598-1609
[6] Sharma MK, Buettner GR, Kerber RE. Angiotensin converting enzyme inhibitors reduce free radical generation during post-ischemic reperfusion of canine myocardium: a real time study by electron spin resonance spectroscopy [abstract]. J Am Coll Cardiol 1993; 21:410A
[7] Chopra M, McMurray J, Stewart J, et al. Free radical scavenging: a potentially beneficial action of thiol-containing angiotensin converting enzyme inhibitors. Biochem Soc Trans 1990; 18:1184-1185
[8] Przyklenk K, Kloner RA. Angiotensin converting enzyme inhibitors improve contractile function of stunned myocardium by different mechanisms of action. Am Heart J 1991; 121:1319-1330
[9] Mehta JL, Nicolini FA, Dawson DL. Sulfhydryl group in angiotensin converting enzyme inhibitors and superoxide radical formation. J Cardiovasc Pharmacol 1990; 16:847-849
[10] Sharma MK, Buettner GR, Spencer KT, et al. Ascorbyl free radical as a real-time marker of free radical generation in briefly ischemic and reperfused hearts: an electron paramagnetic resonance study. Circ Res 1994; 74:650-658
[11] Bielski BH. Chemistry of ascorbic acid radicals. In: Seib PA, Tolbert BM, eds. Ascorbic acid: chemistry, metabolism and uses, advances in chemistry series 200. Washington, DC: American Chemical Society, 1982; 81
[12] Buettner GR. The pecking order of free radicals and antioxidants: lipid peroxidation, [Alpha]-tocopherol, and ascorbate. Arch Biochem Biophys 1993; 300:535-543
[13] Frei B, Stocker R, Ames BN. Antioxidant defenses and lipid peroxidation in human blood plasma. Proc Natl Acad Sci USA 1988; 85:9748-9752
[14] Frei B, England L, Ames BN. Ascorbate is an outstanding antioxidant in human plasma. Proc Natl Acad Sci USA 1989; 86:6377-6381
[15] Buettner GR, Jurkiewicz BA. Ascorbate free radical as a marker of oxidative stress: an EPR study. Free Radic Biol Med 1993; 14:49-55
[16] Buettner GR, Kiminyo KP. Optimal EPR detection of weak nitroxide spin adduct and ascorbyl free radical signals. J Biochem Biophys Methods 1992; 24:147-151
[17] Pansegrau DG, Abboud FM. Hemodynamic effects of ventricular defibrillation. J Clin Invest 1970; 49:282-297
[18] Przyklenk K, Kloner RA. Acute effects of hydralazine and enalapril on contractile function of post ischemic "stunned" myocardium. Am J Cardiol 1987; 60:934-936
[19] Sweet CS. Pharmacologic properties of the converting enzyme inhibitor, enalapril maleate (MK-421). Fed Proc 1983; 42:167-170
[20] Koerner JE, Anderson BA, Dage RC. Protection against post ischemic myocardial dysfunction in anesthetized rabbits with scavengers of oxygen-derived free radicals: superoxide dismutase plus catalase, N-2-mercaptopropionyl glycine and captopril. J Cardiovasc Pharmacol 1991; 17:185-191
[21] Westlin W, Mullane K. Does captopril attenuate reperfusion-induced myocardial dysfunction by scavenging free radicals? Circulation 1988; 77:130-139
[22] Van Vleet JF, Tacker WA. Cardiac damage from transchest and ICD defibrillator shocks. In: Tacker WA Jr, ed. Defibrillation of the heart ICDs, AEDS, and manuals. St. Louis, MO: Mosby, 1994; 259-298
[23] Weaver WD, Cobb LA, Copass MK, et al. Ventricular defibrillation: a comparative trial using 175-J and 320-J shocks. N Engl J Med 1982; 307:1101-1106
[24] Fatkin D, Kuchar DL, Thorburn CW, et al. Transesophageal echocardiography before and during direct current cardioversion of atrial fibrillation: evidence for atrial stunning as a mechanism of thromboembolic complications. J Am Coll Cardiol 1994; 23:307-316
[25] Loesser KE, Kukreja RC, Kazziha SY, et al. Oxidative damage to the myocardium: a fundamental mechanism of myocardial injury. Cardioscience 1991; 2:199-216
[26] Myers ML, Bolli R, Lekich RF, et al. Enhancement of recovery of myocardial function by oxygen free radical scavengers after reversible regional ischemia. Circulation 1985; 72:915-921
[27] Bolli R, Jeroudi MO, Patel BS, et al. Direct evidence that oxygen-derived free radicals contribute to post-ischemic myocardial dysfunction in the intact dog. Proc Natl Acad Sci USA 1989; 86:4695-4699
[28] Jolly SR, Kane WJ, Bailie MB, et al. Canine myocardial reperfusion injury: its reduction by the combined administration of superoxide dismutase and catalase. Circ Res 1984; 54:277-285
[29] Bolli R, Patel BS, Jeroudi MO, et al. Demonstration of free radical generation in "stunned" myocardium of intact dogs with the use of the spin trap [Alpha]-phenyl N-tert-butyl nitrone. J Clin Invest 1988; 82:476-485
[30] Bagchi D, Prasad R, Das DK. Direct scavenging of free radicals by captopril, an angiotensin converting enzyme inhibitor. Biochem Biophys Res Comm 1982; 158:52-57
[31] Mira ML, Silva MM, Manso CF. The scavenging of oxygen free radicals by angiotensin converting enzyme inhibitors: the importance of the sulfhydryl group in the chemical structure of the compounds. Ann NY Acad Sci 1994; 723:439-441
(*) From the Cardiovascular Center, University of Iowa, Iowa City, IA.
Supported in part by National Heart, Lung, and Blood Institute grants HL-07121 (Drs. Pagan-Carlo and Garcia) and HL53284-02 (Dr. Kerber), in part by grant 94-GS-46 from the American Heart Association, Iowa Affiliate, and in part by a grant from the Laerdal Foundation for Acute Medical Care.
Manuscript received November 3, 1998; revision accepted February 25, 1999.
Correspondence to: Richard E. Kerber, MD, Department of Medicine, University of Iowa Hospital, 200 Hawkins Dr, Iowa City, IA 52242; e-mail: richard-kerber@uiowa.edu
COPYRIGHT 1999 American College of Chest Physicians
COPYRIGHT 2000 Gale Group