G Ramsaransing, C Zwanikken, J De Keyser, Department of Neurology, Academisch Ziekenhuis Groningen, Hanzeplein 1,9700 RB Groningen, Netherlands Correspondence to: J De Keyser j.h.a.de.keyser@neuro.azg.nl
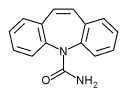
Carbamazepine is widely used to treat paroxysmal neurological symptoms and pain. We report on five patients with multiple sclerosis in whom disability was seriously enhanced by treatment with carbamazepine at comparatively low dosages. It is possible to misinterpret worsening of symptoms as an exacerbation of multiple sclerosis.
Case 1
A 48 year old man had had symptoms of multiple sclerosis for three years, at first intermittent but eventually progressive, with mainly ataxia and spastic weakness of the legs. He also had disabling oscillopsia due to a multidirectional nystagmus. Two days after starting carbamazepine (100 mg three times daily) he was unable to walk because of increased weakness, but two days after stopping it he could walk unassisted. Carbamazepine (50 mg three times daily) was restarted one week later without any change in symptoms. When the dose was increased to 100 mg three times daily he developed a profound weakness of the legs, which disappeared two days after stopping treatment.
Case 2
A 67 year old woman with secondary progressive multiple sclerosis had a recurrence of right sided trigeminal neuralgia. Although she was severely disabled (ataxia of all limbs and spastic weakness of her legs), she could walk with a frame. Carbamazepine 100 mg three times daily was started. Two days later she could not stand owing to weakness of her legs. The sudden worsening was interpreted as an exacerbation, and she was treated with intravenous methylprednisolone 500 mg daily for five days, without benefit. Two weeks after discharge she was seen at the clinic. Carbamazepine was stopped, and two days later she could walk with a frame. She recalled a less severe effect from carbamazepine during the previous episode of trigeminal neuralgia.
Over the past year three further women with secondary progressive multiple sclerosis showed worsening of symptoms with carbamazepine, prescribed for trigeminal neuralgia. Each patient received comparatively low doses of carbamazepine (300-600 mg daily). Two had profound weakness of the legs and increased difficulties with micturition, whereas one, who was bedridden, lost the use of her upper limbs. Symptoms worsened within the first three days of starting carbamazepine and disappeared within two days of stopping it.
In multiple sclerosis there is a remodelling of the demyelinated axonal membrane so that it acquires more sodium channels than normal, which permits conduction of action potentials despite the loss of myelin.[1] Carbamazepine may counteract this compensatory mechanism by blocking sodium channels.
Funding: GR was supported by Multiple Sclerosis International.
[1] Sedgwick EM. Pathophysiology of the demyelinated nerve fibre. In Raine CS, McFarland HF, Tourtellotte WW, eds. Multiple sclerosis. Clinical and pathogenetic basis. London: Chapman and Hall, 1997:195-204.
COPYRIGHT 2000 British Medical Association
COPYRIGHT 2000 Gale Group