INTRODUCTION
Human opiate withdrawal was systematically described early in the twentieth century (1). More recent research, conducted primarily in rodents, identified several neurobiological mechanisms subserving opiate dependence and withdrawal (2). Yet, the spectrum of behaviors observed during opiate withdrawal are quite different in rodents and primates (3-6). These differences across species highlight the need for investigation of brain mechanisms involved with opiate dependence and withdrawal in humans. Currently, little is known of regional brain contributions to opiate dependence and withdrawal states in humans.
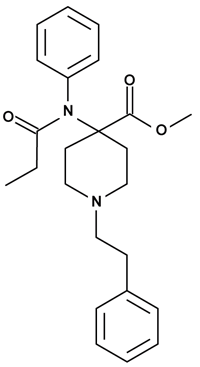
To date, regional brain mechanisms associated with opiate dependence and withdrawal have not been studied using single photon emission computerized tomography (SPECT) in humans. Regional effects of acute morphine administration have been studied using positron emission tomography (PET). A PET study employing [sup.18]F]fluorodeoxyglucose (FDG) reported that morphine administration reduced glucose metabolism in the whole brain and a large number of cortical and subcortical regions (7). A preliminary study using FDG-PET found evidence of regional alterations in brain function in two heroin-dependent men as compared to with three subjects who had histories of opiate abuse but not current physical dependence upon opiates (8). Furthermore, PET studies using [sup.11]C]carfentanil have identified regional variations in human [mu] opiate receptor binding (9, 10). Alterations in opiate receptor number of affinity have not yet been described in humans undergoing opiate dependence or withdrawal using PET opiate receptor binding techniques.
The [sup.99]mTc]d,l-hexamethylpropyleneamine oxime (HMPAO) SPECT technique provides a functional index related to regional brain perfusion. HMPAO is taken up by the brain in proportion to cerebral perfusion, and it diffuses passively into neuronal tissues where it is metabolically trapped within approximately 2 minutes after injection (11-14). Once plateau levels of HMPAO are reached in the brain, within 10 minutes of injection, there is a negligible loss of tracer due to backdiffusion, approximately 0.4% per hour (15). These properties permit one to inject HMPAO during opiate withdrawal, to image the subject later when withdrawal symptoms have subsided, and to collect data upon later brain imaging reflecting the initial withdrawal state.
This preliminary study employed HMPAO-SPECT to study regional brain function in healthy subjects and opiate-dependent patients after saline or naloxone infusion. In doing so, this study provided an initial assessment of the capacity of this technique to evaluate regional changes in brain function associated with opiate dependence and withdrawal.
METHODS
Opiate-Dependent Patients
Ten right-handed methadone-maintained patients (6 male, 4 female; mean age: 35.6 [+ or -] 4.2 (SD) yr; mean weight: 68.9 [+ or -] 17.6 kg; mean methadone dose: 29 [+ or -] 10 mg) with greater than a 6-month history of opiate dependence participated in the study. Patients were recruited from the methadone treatment programs of the Yale Substance Abuse Treatment Units. Prior to initiating methadone maintenance in these programs, each individual underwent a naloxone test comparable to that employed in this study (0.8 mg., s.c.) in order to document their physical dependence on opiates (16). Patients participating in this study were maintained on a stable dose of methadone for at least 2 weeks prior to testing. Upon entering the study, a research psychiatrist completed a medical history, a semistructured psychiatric interview to determine DSM-III-R Axis I diagnoses (17), and conducted a physical examination. In addition, patients completed a battery of medical laboratory tests including liver function tests, thyroid function tests, electrolytes, BUN, creatinine, HIV antibody, and electrocardiogram. Patients were excluded if they suffered from medical illness, were HIV positive, or met criteria for schizophrenia or other psychotic disorder. Besides substance abuse, no other DSM-III-R Axis I diagnoses were found in the prospective patient sample. With one exception, all patients had histories of polysubstance abuse. All but one subject were free of illicit substance abuse based on history and weekly supervised toxicology screens during the 2-week evaluation period. One subject reported a single incidence of cocaine use in the 2 weeks prior to testing confirmed by a single positive urine toxicology test. Urine toxicology testing on test days was negative in this subject. Data from this subject did not differ from the remainder of the patient group on any outcome measure. As a result, this individual was included in this presentation.
John H. Krystal, M.D. To whom correspondence should be addressed at Psychiatry Service, West Haven VA Medical Center, West Haven, Connecticut 06516.
Healthy Subjects
Ten right-handed healthy subjects (6 male, 4 female; mean age: 29.3 [+ or -] 6.1 yr; mean weight: 75.0 [+ or -] 14.9 kg) completed testing after giving informed consent. Each subject completed psychiatric and physical screening comparable to the patient sample. Healthy subjects were free of lifetime criteria for a psychiatric illness or substance abuse disorder. Absence of substance abuse history was supported by a urine toxicology screen at the time of recruitment. In addition, none of the subjects had first degree relatives who met criteria for a psychiatric illness. Healthy subjects were matched by gender and weight, but were younger than patients (t = 2.7, df = 18, p = .02).
Test Sessions
After given written informed consent, each patient or healthy subject participated in 2 test days, separated by a day, during which they received naloxone (0.8 mg, s.c.) or saline under double-blind conditions in a randomized order. Patients arrived at the Clinical Neuroscience Research Unit of the Connecticut Mental Health Center on the day prior to testing. Methadone doses were administered daily in the afternoon, so as not to interfere with testing. All study participants took nothing by mouth except water after midnight on the evening prior to testing.
At approximately 8 A.M. an intravenous line was placed and baseline ratings of vital signs and opiate withdrawal were obtained. At approximately 9 A.M. ambient light and sound levels were reduced and participants received naloxone or saline injections. They were then fitted with a sleep mask, asked to close their eyes, and to wear a sound-attenuating headset. When marked opiate withdrawal symptoms emerged, up to 10 minutes following injection, 740 MBq (20 mCi) [sup. 99m]Tc-HMPAO was injected intravenously as a bolus. Injectate lipophilicity was determined to be greater than 80% in all cases by paper chromatography. Approximately 15 minutes later, patients and healthy subjects completed assessments of opiate withdrawal severity and vital signs.
If significant withdrawal symptoms persisted for more than 45 minutes, subjects were administered morphine (2 mg, i.v.). All patients and no healthy subjects received morphine, and this drug suppressed residual withdrawal symptoms rapidly. At this point, patients and healthy subjects were escorted to the Nuclear Medicine Suite at Yale-New Haven Hospital where they underwent SPECT scanning using a multicrystal head-dedicated camera (Strichman 810X, Strichman Medical Equipment, Inc., Medfield, Massachusetts). Laser lights were used to align the head so that the orbitocanthalauditory meatal (OCM) line was parallel bilaterally to the plane of the first slice. The head was fixed to the scanner bed using a thermoplastic mask (Precision Splint, Polymed Co., Baltimore, Maryland) and rested in an individually molded vacuum bean bag (Olympic Vac-Pac, Seattle, Washington) to minimize head movement. Ten to 16 transaxial slices, each 5-10 mm apart, were obtained using the Strichman camera (X-Y plane resolution 8 mm in periphery, 10 mm at center, Z axis resolution of 13 mm). Scan lengths varied between 50 and 80 minutes. A computerized X-ray tomographic scan was obtained on 1 of the 2 study days, with the mask in place, to facilitate generating anatomical CT slides in the same orientation as the SPECT studies.
Behavioral and Physiologic Assessments
Opiate withdrawal was assessed using the Ribicoff Abstinence Rating Scale for opiate withdrawal that has been used in previous studies (18). Patients and healthy subjects completed a self-rating version of the scale, and staff completed an observer-rated version of the scale. Self-ratings were quite consistent with observer ratings and will be reported here. Abstinence levels were assessed before and 10 minutes following naloxone or saline infusion. Vital signs were assessed at the 0- (before drug administration), 5-, and 15-minute timepoints.
Image Analysis
Images were reconstructed using the SME Neuro900 program v.2.7 (Strichman Medical Equipment, Medfield, Massachusetts) for the MacIntosh IICX computer. Images were reconstructed with a fixed filter to eliminate variability associated with the software program's automatic selection of different filters based upon the total counts in each slice. Total counts per pixel per minute for whole brain and for six bilateral regions of interest (frontal, parietal, temporal, and cingulate cortices; basal ganglia; and thalamus) were determined by a trained technician blind to subject and test day information. CT scans and a brain atlas of brain slices cut parallel to the OCM line guided the regional analyses. This study will report adjusted ratios of the counts per pixel per minute in the region of interest (ROI) divided by the counts per pixel per minute for the whole brain. ROI's appearing in more than one slice were delineated in each relevant slice and then averaged across slices weighted by area. The weighted average of the whole slices minus the cerebellum was taken as the supratentorial whole brain, called "whole brain" for purposes of convenience in this presentation.
Statistical Analyses
Behavioral and physiologic responses were initially assessed using repeated measures analysis of variance including within subjects factors of naloxone (naloxone vs placebo) and time and the between subject factor of diagnosis (patients vs healthy subjects).
Counts per region or whole brain were corrected for variations in the dose, lipophilicity of the HMPAO injected, and technetium decay. Attenuation correction was performed using an ellipse drawn around the brain assuming uniform attenuation equal to water. Initial image analyses were performed on whole brain count density defined as counts/pixel/min for the whole brain. Regional brain activity ratios were defined as the {corrected regional counts/pixel/minute [divided by]. corrected whole brain counts/pixel/minute}. Difference scores (naloxone day - saline day) were calculated for whole brain count density and regional brain activity ratios. Within subject comparisons were conducted using two-tailed paired t-tests and between subject comparisons employed Student's t-tests.
The time period between injection and imaging did not differ in healthy subjects between test days (saline day: 40.2 [+ or -] 11.1 min, naloxone day: 52.8 [+ or -] 12.7 min; t = 1.3, df = 9, p = .2). In patients, the elicitation of withdrawal symptoms produced a nonsignificant increase in this interval (saline day: 75.4 [+ or -] 9.3 min, naloxone day: 137.2 [+ or -] 22.2 min; t = 2.2, df = 9, p = .06). Patients had longer injection-to-scan delays than healthy subjects on both the saline day (t = 2.4, df = 18, p = .03) and the naloxone day (t = 3.3, df = 18, p = .004). Comparison of the difference between the naloxone and saline days revealed a nonsignificant trend for patients relative to healthy subjects (healthy subjects: 12.6 [+ or -] 10.9 min, patients: 70.2 [+ or -] 33.0 min; t = 1.6, df = 18, p = .1). In light of published data on the rate of backdiffusion (14), the increase in the injection-to-scan interval in patients should have reduced counts on the naloxone day in patients by approximately 0.4%, a statistically insignificant amount.
RESULTS
Assessments of Opiate Abstinence
Repeated measures analysis of variance of opiate withdrawal signs and symptoms assessed by the RARS, showed significant main effects of diagnosis ([F.sub.1.18] = 50 3, p = .0001), naloxone ([F.sub.1.18] = 70.2, p = .0001), and time ([F.sub.1.18] = 33.6, p = .0001). The interactions of naloxone and time ([F.sub.1.18] = 39.0, p = .0001) and the interaction of diagnosis x naloxone x time ([F.sub.1.18] = 38.8, p = .0001) were statistically significant. Naloxone did not produce measurable opiate withdrawal symptoms in any healthy subject (naloxone day: RARS baseline: 24.8 [+ or -] 0.6 {SEM}; RARS postnaloxone: 24.2 [+ or -] 0.1). In patients, saline infusion had no demonstrable behavioral effects upon withdrawal ratings (saline day: RARS baseline: 25.8 [+ or -] 0.7; RARS postnaloxone: 25.5 [+ or -] 1.2). However, naloxone produced moderateto-severe opiate withdrawal symptoms in all patients (naloxone day: RARS baseline: 28.4 [+ or -] 1.3; RARS postnaloxone: 72.3 [+ or -] 6.7). Almost all patients experienced anxiety, irritability, tremor, sweating, nausea, myalgia, piloerection, ataxia, and increased craving for opiates. Approximately half of the patients had vomiting, lacrimation, diarrhea, rhinorrhea, and yawning. All of these symptoms abated prior to completion of the test day.
Vital Signs
Systolic blood pressure. Repeated measures analysis of variance of systolic blood pressure showed significant effects of time ([F.sub.2.28] = 8.4, p = .001), the interaction of naloxone and time ([F.sub.2.28] = 6.9, p = .004), and the diagnosis x naloxone x time interaction (F228 = 8.7, p = .001). Naloxone did not have significant effects on systolic blood pressure in healthy subjects. Baseline systolic blood pressure did not differ in healthy subjects and patients (placebo day, healthy subjects: 99.7 [+ or -] 2.1 mmHg; patients: 101.1 [+ or -] 8.6 mmHg. naloxone day, healthy subjects: 94.7 [+ or -] 2.2 mmHg; patients: 103.3 [+ or -] 8.0 mmHg). Patients increased systolic blood pressure at the 15-minute timepoint on the naloxone day (130.0 [+ or -] 13.0 mmHg), but not on the saline day (100.2 [+ or -] 8.8 mmHg).
Diastolic blood pressure. Repeated measures ANOVA of diastolic blood pressure showed significant effects of time ([F.sub.2.28] = 10.1, p = .0001) and the diagnosis x naloxone x time interaction ([F.sub.2.28] = 15.1, p = .0001). Naloxone did not have significant effects on diastolic blood pressure in healthy subjects. Baseline diastolic blood pressure did not differ in healthy subjects and patients (placebo day, healthy subjects: 64.6 _ 1.9 mmHg; patients: 64.4 [+ or -] 4.7 mmHg. naloxone day, healthy subjects: 59.7 [+ or -] 0.6 mmHg; patients: 64.9 [+ or -] 3.7 mmHg). Patients increased diastolic blood pressure at the 15-minute timepoint on the naloxone day (77.8 [+ or -] 6.0 mmHg), but not the saline day (65.3 [+ or -] 5.0 mmHg).
Pulse. ANOVA did not reveal any significant main effects or interactions for pulse data.
Whole Brain Count Density
As described in Table 1, naloxone had no significant effect on whole brain count density in healthy subjects. Patients and healthy subjects did not significantly differ in their saline day whole brain count densities, but patients had lower count densities following naloxone. Analysis of difference scores revealed significant group effects. Relative to their saline day, healthy subjects exhibited a nonsignificant increase following naloxone, and patients significantly decreased their whole brain counts during withdrawal.
[TABULAR DATA OMITTED]
Region/Whole Brain Activity Ratios
Table 1 presents activity ratio data for healthy subjects and opiate-dependent patients. Comparison of naloxone and saline day scores indicated that healthy subjects exhibited a statistically significant reduction in the right parietal cortex activity ratio and significant increases in the right temporal cortex and left basal ganglia activity ratios on the naloxone day relative to the saline day. Patients showed no significant regional activity differences between their test days.
Regional differences associated with opiate dependence were assessed by comparing saline days in healthy subjects and patients. Patients exhibited significant lower activity ratios bilaterally in the frontal and parietal cortices, with a nonsignificant trend in the anterior cingulate gyrus. Patients also exhibited increased bilateral thalamic activity ratios.
Regional differences associated with opiate withdrawal were assessed by comparing patients and healthy subjects on their naloxone test days. Patients had lower bilateral frontal and parietal activity ratios and greater bilateral thalamic activity ratios than healthy subjects on the naloxone test day.
Withdrawal was also assessed by comparing the difference on naloxone and saline test days. In the right temporal cortex, healthy subjects exhibited a small but significant activity ratio increase while patients exhibited a nonsignificant decrease of comparable magnitude. This group comparison reached statistical significance. In the left frontal cortex, healthy subjects showed a nonsignificant activity ratio reduction while patients exhibited a smaller nonsignificant decrease, resulting in a group difference at the level of a nonsignificant trend.
DISCUSSION
This preliminary study is the first attempt, to our knowledge, to characterize regional changes in brain function associated with opiate dependence and naloxone-precipitated withdrawal in humans with a functional brain imaging technique. Opiate dependence was associated with decreased frontal and parietal activity ratios and increased thalamic activity ratios. The decreases do not appear to be secondary to volumetric loss since anatomical studies using MRI have been normal in healthy opiate abusers (19). Adjusting for saline day differences, opiate withdrawal was associated with decreased whole brain count density, a slight increase in the right temporal cortex activity ratio, and a trend toward a decreased frontal cortical activity ratio. Neither of the regional changes were large in magnitude. The significant decline in whole brain count density in patients undergoing withdrawal could reflect the effects of withdrawal-induced hyperventilation. Hyperventilation has been previously shown to reduce HMPAO-SPECT whole brain count density without altering regional brain activity ratios (20). Measurement of PC[O.sub. 2] and quantitative cerebral blood flow during opiate withdrawal would be useful in future studies. In addition, future studies may benefit from controlling for the degree of tobacco smoking in the subjects studied, since nicotine may alter regional brain metabolism rates (21). Although this study demonstrated significant group differences using HMPAOSPECT associated with opiate dependence and withdrawal, this study failed to find regional changes in brain activity ratios in patients when the resting state and opiate withdrawal were compared within individuals.
Studies in the rat using the 2-deoxyglucose technique (22) found a complex array of regional alterations in brain glucose metabolism associated with acute opiate administration, chronic opiate administration, and antagonistprecipitated withdrawal. Acute opiate administration appears to be associated with subcortical decreases in metabolic activity (23, 24). Chronic opiate administration is associated with tolerance to these effects (23, 24). In their initial study, Wooten and his colleagues found metabolic increases in thalamic, amygdalar, and preoptic nuclei, and metabolic decreases in hippocampal structures during withdrawal (25). Later studies, under different conditions and by quantitative methods, found withdrawal-induced activation of additional brain structures (24, 26). Naloxone-precipitated withdrawal is associated with alterations in glucose utilization similar to spontaneous withdrawal (27), while naloxone administration to nondependent rats appears to have little effect on local glucose utilization (28). Regional metabolic alterations measured in association with opiate withdrawal appear to be dependent on the degree of opiate dependence (29), the dose of naloxone used to precipitate withdrawal (30), the display of particular withdrawal behaviors (30, 31), and the period between the initiation of withdrawal and the injection of deoxyglucose (32). Pharmacologic suppression of opiate withdrawal with clonidine attenuates the regional brain metabolic changes associated with naloxone-precipitated withdrawal (31). A study examining cerebral blood flow in the rat using the iodoantipyrine technique failed to find regional changes (26), perhaps consistent with the limited findings of the current study.
In light of the relatively subtle findings of the current study, further research may be needed to determine optimal approaches for perfusion- or metabolism-related assessments of regional brain function associated with opiate withdrawal in humans. Also, SPECT may be inferior to high-speed magnetic resonance imaging (MRI) (33) techniques for assessing brain functions related to blood flow or perfusion. The animal literature cited above suggests that glucose metabolism, as measured by PET, may be more sensitive than perfusion techniques in detecting functional alterations associated with opiate withdrawal. In addition, the evaluation of the association of specific regional brain activity ratio patterns with the degree of opiate dependency, naloxone dose, and particular withdrawal behaviors elicited will require further evaluation in a larger sample of patients.
The current study illustrates the feasibility of HMPAO-SPECT for evaluating transient dysphoric states, such as opiate withdrawal. The ability to image the patient after treatment or the resolution of dysphoria is a significant advantage of HMPAO-SPECT. As a result, HMPAO-SPECT has been used to evaluate regional cerebral perfusion under a variety of adverse conditions including seizures (34) and yohimbine-induced panic attacks (35). This technique correlates highly with other SPECT and PET techniques for assessing functions related to regional cerebral blood flow (rCBF) (15, 36, 37). Although rCBF estimates generally correlate with measures of metabolism (38-40), these measures differ under many conditions due to 1) differential activation of rCBF and metabolism under certain physiologic challenges (39, 41); 2) the increased rapidity of rCBF responses relative to metabolism (42, 43); and 3) differing microanatomical localization of processes reflected in rCBF and metabolism (20, 42). Evaluations of human opiate withdrawal based on assessments of regional glucose metabolism with PET or rCBF with PET or high-speed MRI will present challenges. Using these techniques, subjects will need to remain still while suffering abstinence symptoms. However, the limited utility of the HMPAO-SPECT methods employed in the current study necessitates the evaluation of these alternative strategies relative to HMPAO-SPECT for assessing regional brain contributions to opiate dependence and withdrawal in humans. Future SPECT studies should incorporate recent advances in SPECT methodology, such as coregistration of anatomical (magnetic resonance imaging) and functional images in the data analysis (43) and cerebral blood flow quantification (36).
ACKNOWLEDGMENTS
The investigators thank the staffs of the Clinical Neuroscience Research Unit, the Yale Substance Abuse Treatment Unit (SATU), and the Department of Nuclear Medicine who made this study possible. In particular, Mr. Mark Hayes and Ms. Eileen Smith are thanked for their critical contributions. Ms. Deborah Herbst and Mr. Pedro Mendia are thanked for assistance with data analysis. These studies were supported by the National Institute on Drug Abuse (NIDA) through the following grants: P50-DA04060, R18DA06190, KO2-DA00112 (T.R.K.). Additional support was provided by the Department of Veterans Affairs for the VA-Yale Alcoholism Research Center (J.H.K.) .
REFERENCES