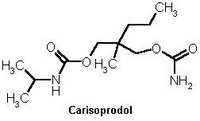
Carisoprodol (Soma, others), a nonscheduled prescription medication, is a centrally acting synthetic skeletal muscle relaxant structurally and pharmacologically related to meprobamate (Miltown, Equinil), a potentially addictive agent. Carisoprodol undergoes hepatic biotransformation to three primary metabolites: hydroxycarisoprodol, hydroxymeprobamate, and meprobamate. The significant serum levels of meprobamate after chronic use of carisoprodol may lead to meprobarnate dependency: Withdrawal from meprobamate may result in severe reactions including seizures and coma.
Ms. A, a 37-year-old White female, was admitted to the University of Kentucky Medical Center on June 16, 1990, following a motor vehicle accident in which she sustained Cl, T6, right ankle, and multiple rib fractures. A routine urine drug screen revealed the presence of meprobamate and phenothiazine metabolites. A quantitative serum analysis revealed a meprobamate level of 19.8 [mu]g/L which is equivalent to peak levels observed after ingestion of 400 mg oral meprobamate in normal volunteers. Ms. A denied recent use of meprobamate. Despite the use of greater than 100 mg intravenous morphine for 3 days postoperatively, the patient continued to complain of pain. A psychiatry consult uncovered a history of multiple drug abuse including sleeping pills, muscle relaxants, and marijuana. The patient had been hospitalized once in 1987 for detoxification. Ms. A admitted to taking carisoprodol (Soma) for lower back pain and that she had taken some just prior to her motor vehicle accident. She continued, however, to deny recent use of meprobamate. She required higher than normal doses of narcotics throughout her hospital stay. Ms. A was discharged in stable condition on hospital day 11 with prescriptions for methadone 12.5 mg orally every 8 hours and ibuprofen 600 mg orally every 6 hours. She also was given an appointment with a substance abuse counselor and instructed that all prescriptions for methadone would be written only by physicians in the Pain Management Clinic. It was agreed that die patient would remain carisoprodol-free. Following discharge, the patient did not consistently attend appointments with her counselor but was successfully weaned from methadone by Pain Management physicians. Recently it was learned that the patient is under legal investigation for passing forged carisoprodol prescriptions at numerous pharmacies in the area of her residence.
Meprobamate dependence is a possible complication of chronic carisoprodol use due to hepatic conversion of carisoprodol to meprobamate. Two previous reports[1, 2] have described such dependence and we report an additional case. Carisoprodol (Soma) is prescribed frequently by family physicians, internists, orthopedic surgeons, neurologists, neurosurgeons, anesthesiologists, and psychiatrists as well as other healthcare professionals. Carisoprodol prescribers need to be made aware of its abuse potential. Stricter controls may be necessary in the future to properly control the prescribing and distribution of this potentially addictive agent.
REFERENCES
[1] Morse, R. M., and Chua, L., Carisoprodol dependence: A case report, Am. J. Drug Alcohol Abuse 5:527-530 (1978). [2] Luehr, J. G., Meyerle, K. A., and Larson, E. W., Mail-order (veterinary) drug dependence, JAMA 263:657 (1990).
Letters
Methadone Maintenance and Recovery
In their recent article, Maddux and Desmond[1] reviewed follow-up studies of patients who had been treated with methadone maintenance and of others who received drug-free treatment.
Comparisons of different addiction treatment modalities are always difficult. The difficulty is compounded, however, when comparing posttreatment outcomes. Many methadone programs discontinue treatment primarily as a result of what is deemed therapeutic failure, e.g., continued use of illicit drugs, noncompliance with program rules, etc. On the other hand, most drug-free programs plan from the day of admission for "graduation" of patients after a prescribed course of treatment is completed, and those discharged in this fashion are defined as successful clients. Analysis of follow-up studies when programs have such disparate goals inevitably will yield data which are difficult to interpret. Nevertheless, one can hardly quarrel with the cautions conclusion of the authors that the articles they reviewed "... do not suggest that methadone maintenance impedes eventual recovery from opioid dependence, but they do not clearly exclude such an effect."
A more fundamental question raised by this article, however, is whether "recovery from opioid dependence" is a meaningful concept. To date, no one knows what "opioid dependence" is, let alone how to define, identify, or help patients achieve "recovery. " The authors whose studies are quoted by Maddux and Desmond merely determined whether or not there was a state of abstinence from heroin (and, in some instances, from other drugs and alcohol as well) at some arbitrary interval after treatment ended. This can hardly be deemed synonymous with "recovery" from such a notoriously recidivist condition as "addiction."
It is not unreasonable to postulate today, as Dole and Nyswander did a quarter-century ago[2], that "opioid dependence" reflects a physiological perturbation that is neither resolved nor even mitigated by any of the therapeutic modalities which are employed in the treatment of narcotic addicts. Should the possibility that this hypothesis is correct be the cause for gloom? Not at all! Unlike so many other diseases whose nature and etiology are unknown, and/or which defy "cure," heroin addiction is a condition which can be treated successfully - as measured by cessation of heroin use, sharply reduced morbidity and mortality, and restoration of the ability to lead a productive and self-fulfilling life. Not a bad set of objectives - objectives which, as Desmond and Maddux acknowledge, are achievable with methadone maintenance and, presumably, with other modalities as well.
We do a disservice to methadone maintenance programs and their patients by suggesting that "completion" of treatment and subsequent abstinence are the sine qua non of therapeutic success in the treatment of opioid dependence. Research efforts certainly should focus on understanding the factors which cause or contribute to addiction, and identifying potential "cures" of addictive disease(s). At the same time, our public policy should be focused on making effective treatment available promptly to all those who want it and need it.
REFERENCES
[1] Maddux, J. F., and Desmond, D. P., Methadone maintenance and recovery from opioid dependence, Am. J. Drug Alcohol Abuse 18(1):63-74 (1992). [2] Dole, V.P., and Nyswander, M.E., Heroin addiction - A metabolic disease, Arch. Intern. Med. 120:19-24 (1967).
Response. Our review did not attempt to compare the treatment success or failure of methadone maintenance programs with those of drug-free treatment programs. As Dr. Newman points out, the disparate goals make such comparison difficult. Our inquiry focused narrowly on the long-term outcomes with respect to recovery from opioid dependence.
Dr. Newman questions the concept of "recovery from opioid dependence." We used "recovery" in the usual dictionary sense of "regaining or returning toward a normal or usual state"[1]. We used abstinence not as a synonym for recovery but as an indicator of some degree of recovery. Similarly, a return to a normal temperature may serve as an indicator of recovery from an infection. The National Institute on Drug Abuse apparently considers recovery from substance abuse (including opioid dependence) to be a useful concept. The agency sponsored a conference which focused on this topic and published a research monograph entitled Relapse and Recovery in Substance Abuse[2]. Of course, "recovery" is an abstract term, and it can be limited by specific criteria. If we limit "recovery" to mean total and complete return to a premorbid state, then recovery from opioid dependence (and from many other disorders) seems unlikely.
The studies of the acute and protracted abstinence syndromes which we cited in our article support the concept of a "physiological perturbation," but they do not provide evidence of irreversible neural change. The evidence, in our interpretation, suggests a slow recovery after cessation of opioid use.
We do not know if the authors of the article are included in the "We" who "do a disservice to methadone maintenance programs and their patients by suggesting that |completion' of treatment and subsequent abstinence are the sine qua non of therapeutic success in the treatment of opioid dependence." We cannot find an assertion resembling this one in our article. As we mentioned earlier, our review was not focused on treatment success or failure. We wish to assure Dr. Newman that we do not oppose methadone maintenance. He may not be aware that the senior author reported one of the early studies which supported the effectiveness of methadone maintenance[3]. Currently we are conducting a five-year NIDA-supported project entitled "Improving Retention on Methadone Maintenance." We advocate both methadone maintenance and drug-free modes of treatment. We also advocate research into all aspects of treatment of drug abuse.
REFERENCES
[1] Webster's Third New International Dictionary, Unabridged. G. and C. Merriam, Springfield, Massachusetts, 1971. [2] Tims, F. M., and Leukefeld, C. G. (Eds.), Relapse and Recovery in Drug Abuse [National Institute on Drug Abuse Research Monograph 72, DHHS Publication (ADM) 86-14731, U.S. Department of Health and Human Services, Rockville, Maryland, 1986. [3] Maddux, J. F., and McDonald, L. K., Status of 100 San Antonio addicts one year after admission to methadone maintenance, Drug Forum 2:239-252 (1973).
COPYRIGHT 1993 Taylor & Francis Ltd.
COPYRIGHT 2004 Gale Group