Nicotine addiction is a chronic condition with a very high rate of relapse. Pharmacologic agents significantly increase a person's chances of quitting, particularly when used as part of a comprehensive plan that also includes counseling and peer support.
In 2000, governmental and nonprofit organizations issued the clinical practice guideline "Treating Tobacco Use and Dependence." TTUD lists five products as first-line agents: sustained-release bupropion and four nicotine-replacement products (gum, patch, nasal spray, and inhaler). A nicotine lozenge is also available now.
Patient preference is the biggest determinant of product choice. Within each product category, experts see no difference between the prescription and over-the-counter formulations. Sustained-release bupropion (Zyban) is the only nonnicotine product currently approved as a first-line agent. It can be used as monotherapy or combined with nicotine replacement.
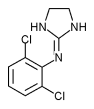
Clonidine and nortriptyline are considered secondline agents. They are not approved by the Food and Drug Administration for this indication, but there is evidence that they make smoking cessation easier.
Patients should start bupropion 1-2 weeks before they stop smoking, to achieve a therapeutic level by the time they quit. Nicotine replacement agents should be started after a patient stops smoking. Information on the activity of nicotine replacement therapy in elderly people is scarce. It's believed that no special dosage adjustments are necessary.
Pregnant women who smoke are urged to use nonpharmacologic means to help them quit. The TTUD states that pharmacologic interventions should be used only if the increased likelihood of abstinence, with its potential benefits, outweighs the risks of drug treatment. If a woman uses nicotine replacement during lactation, the nicotine is excreted into milk, making it safest not to breast-feed. However, both the patch and gum are preferable to smoking if there is no other alternative. There is some evidence that first-trimester bupropion exposure may be related to cardiovascular defects, but additional data are required to confirm this association. Bupropion is also excreted into milk. Although no adverse effects have been noted in nursing infants, the American Academy of Pediatrics has expressed concern that long-term exposure could harm the central nervous system function of these infants. Pregnant women should not start using clonidine because it might cause maternal hypotension and thus decrease placental perfusion. This does not appear to be a risk if the drug is started before pregnancy. Nortriptyline use has not been associated with structural anomalies in developing fetuses, but there have been reports of urinary retention in neonates who had drug exposure in utero. Both clonidine and nortriptyline are excreted into breast milk. There have been no reports of adverse effects in exposed infants.
Mitchel L. Zoler, Editor
Norra MacReady, Writer
COPYRIGHT 2004 International Medical News Group
COPYRIGHT 2004 Gale Group